Monday Poster Session
Category: Small Intestine
P4151 - Beyond Colitis: A Case of Checkpoint Inhibitor-Associated Small Bowel Obstruction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Alkasabrah, MD (he/him/his)
Landmark Medical Center
Woonsocket, RI
Presenting Author(s)
Jatin Thukral, MD1, Omar Alkasabrah, MD1, Harbir Kaur, MD2, Nikhil Thukral, OT3, Sooraj Gopu, MD1, Amanda Lussier, MD4, Abdullah Hafeez, MD1, Avneet Kaur, MBBS5, Syed Naqvi, MD4
1Landmark Medical Center, Woonsocket, RI; 2Hamilton Medical Center, Dalton, GA; 3Pt. Deendayal Upadhyay National Institute for Persons with Physical disability, Delhi, Delhi, India; 4NYMC/Landmark Medical Center, Woonsocket, RI; 5SUNY Upstate Medical University, Syracuse, NY
Introduction: Immune checkpoint inhibitors (ICIs) have become standard therapy for advanced renal cell carcinoma (RCC), but immune-related adverse events (irAEs), particularly involving the gastrointestinal (GI) tract, remain an area of concern. Diarrhea and colitis are relatively common, while small bowel obstruction (SBO) as a complication is exceedingly rare.
Case Description/
Methods: An 87-year-old male with benign prostatic hyperplasia and elevated PSA underwent a prostate biopsy, revealing adenocarcinoma. During staging, a CT scan incidentally revealed a renal mass. Renal biopsy confirmed clear cell RCC, Fuhrman grade 2, with metastasis to retrocrural and periaortic lymph nodes. The patient began treatment with nivolumab and cabozantinib and had stable disease for two years. Due to insurance issues, his regimen was changed to pembrolizumab and lenvatinib.
Following the second session of the new regimen, the patient developed mid-right abdominal pain and diarrhea with initial outpatient management with loperamide, later progressing to constipation and receiving bowel regimen providing minimal relief. With worsening abdominal pain and distension, he presented to the emergency department. A CT abdomen/pelvis showed a high-grade SBO, with a transition point near the ileocecal valve. No history of abdominal surgeries in the past. Surgery recommended conservative management with bowel rest, nasogastric tube with intermittent suctioning, pantoprazole, avoidance of opioids, serial abdominal radiographs and hydration.
After four days of no improvement, oncology was consulted due to concerns for ICI-related toxicity. Given the timing and lack of mechanical cause, pembrolizumab-associated ileus or SBO was suspected. The patient was started on IV Steroids. This was followed by improvement in symptoms and gradual return of bowel function.
Discussion: This case illustrates a rare but clinically significant GI toxicity associated with ICIs. While colitis is well-documented, ICI-induced ileus or SBO is rarely reported, with fewer than 10 such cases documented in the literature. The mechanism is thought to involve immune-mediated inflammation of the enteric nervous system or bowel wall. Prompt recognition and initiation of corticosteroids can prevent complications and avoid unnecessary surgery. Clinicians should maintain a high index of suspicion for ICI-related SBO in patients presenting with new abdominal symptoms, especially when imaging lacks a clear mechanical cause.
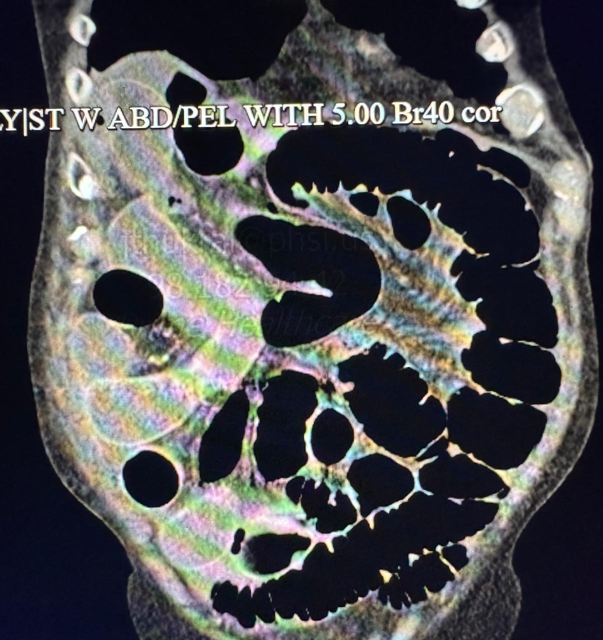
Figure: CT abdomen pelvis with transition point
Disclosures:
Jatin Thukral indicated no relevant financial relationships.
Omar Alkasabrah indicated no relevant financial relationships.
Harbir Kaur indicated no relevant financial relationships.
Nikhil Thukral indicated no relevant financial relationships.
Sooraj Gopu indicated no relevant financial relationships.
Amanda Lussier indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Avneet Kaur indicated no relevant financial relationships.
Syed Naqvi indicated no relevant financial relationships.
Jatin Thukral, MD1, Omar Alkasabrah, MD1, Harbir Kaur, MD2, Nikhil Thukral, OT3, Sooraj Gopu, MD1, Amanda Lussier, MD4, Abdullah Hafeez, MD1, Avneet Kaur, MBBS5, Syed Naqvi, MD4. P4151 - Beyond Colitis: A Case of Checkpoint Inhibitor-Associated Small Bowel Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Landmark Medical Center, Woonsocket, RI; 2Hamilton Medical Center, Dalton, GA; 3Pt. Deendayal Upadhyay National Institute for Persons with Physical disability, Delhi, Delhi, India; 4NYMC/Landmark Medical Center, Woonsocket, RI; 5SUNY Upstate Medical University, Syracuse, NY
Introduction: Immune checkpoint inhibitors (ICIs) have become standard therapy for advanced renal cell carcinoma (RCC), but immune-related adverse events (irAEs), particularly involving the gastrointestinal (GI) tract, remain an area of concern. Diarrhea and colitis are relatively common, while small bowel obstruction (SBO) as a complication is exceedingly rare.
Case Description/
Methods: An 87-year-old male with benign prostatic hyperplasia and elevated PSA underwent a prostate biopsy, revealing adenocarcinoma. During staging, a CT scan incidentally revealed a renal mass. Renal biopsy confirmed clear cell RCC, Fuhrman grade 2, with metastasis to retrocrural and periaortic lymph nodes. The patient began treatment with nivolumab and cabozantinib and had stable disease for two years. Due to insurance issues, his regimen was changed to pembrolizumab and lenvatinib.
Following the second session of the new regimen, the patient developed mid-right abdominal pain and diarrhea with initial outpatient management with loperamide, later progressing to constipation and receiving bowel regimen providing minimal relief. With worsening abdominal pain and distension, he presented to the emergency department. A CT abdomen/pelvis showed a high-grade SBO, with a transition point near the ileocecal valve. No history of abdominal surgeries in the past. Surgery recommended conservative management with bowel rest, nasogastric tube with intermittent suctioning, pantoprazole, avoidance of opioids, serial abdominal radiographs and hydration.
After four days of no improvement, oncology was consulted due to concerns for ICI-related toxicity. Given the timing and lack of mechanical cause, pembrolizumab-associated ileus or SBO was suspected. The patient was started on IV Steroids. This was followed by improvement in symptoms and gradual return of bowel function.
Discussion: This case illustrates a rare but clinically significant GI toxicity associated with ICIs. While colitis is well-documented, ICI-induced ileus or SBO is rarely reported, with fewer than 10 such cases documented in the literature. The mechanism is thought to involve immune-mediated inflammation of the enteric nervous system or bowel wall. Prompt recognition and initiation of corticosteroids can prevent complications and avoid unnecessary surgery. Clinicians should maintain a high index of suspicion for ICI-related SBO in patients presenting with new abdominal symptoms, especially when imaging lacks a clear mechanical cause.
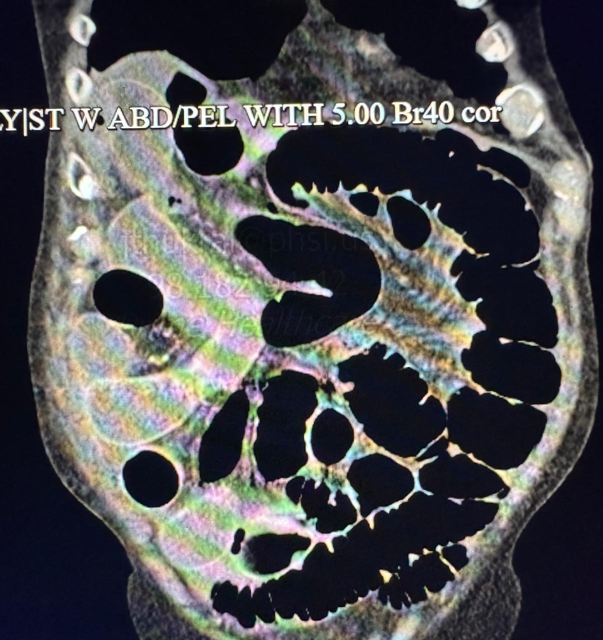
Figure: CT abdomen pelvis with transition point
Disclosures:
Jatin Thukral indicated no relevant financial relationships.
Omar Alkasabrah indicated no relevant financial relationships.
Harbir Kaur indicated no relevant financial relationships.
Nikhil Thukral indicated no relevant financial relationships.
Sooraj Gopu indicated no relevant financial relationships.
Amanda Lussier indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Avneet Kaur indicated no relevant financial relationships.
Syed Naqvi indicated no relevant financial relationships.
Jatin Thukral, MD1, Omar Alkasabrah, MD1, Harbir Kaur, MD2, Nikhil Thukral, OT3, Sooraj Gopu, MD1, Amanda Lussier, MD4, Abdullah Hafeez, MD1, Avneet Kaur, MBBS5, Syed Naqvi, MD4. P4151 - Beyond Colitis: A Case of Checkpoint Inhibitor-Associated Small Bowel Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
