Monday Poster Session
Category: Small Intestine
P4150 - Steroid-Responsive Small Bowel Enteritis in Sjögren’s Syndrome: A Rare Gastrointestinal Manifestation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FJ
Fares Jamal, MD (he/him/his)
Mayo Clinic
Phoenix, AZ
Presenting Author(s)
Oudai Sahwan, MBBS, Fares Jamal, MD, Amani Elshaer, MBBS, Tala B. Shahin, MD, Micheal M. Pham, MD
Mayo Clinic, Phoenix, AZ
Introduction: Sjögren’s syndrome (SS) is a chronic autoimmune disease mainly affecting exocrine glands, often presenting with xerostomia and keratoconjunctivitis sicca. Gastrointestinal (GI) involvement is uncommon and typically limited to upper GI tract. Small bowel enteritis is exceedingly rare and more often linked with systemic lupus erythematosus. We present a unique case of SS-associated small bowel enteritis responsive to immunosuppressive therapy.
Case Description/
Methods: This patient was diagnosed with SS in 2018 with positive ANA, RF, SSA antibodies and salivary lip gland biopsy. By 2021, she developed unusual cyclic episodes of nausea, vomiting, and poor oral intake, resulting in significant weight loss and recurrent hospitalizations. She had frequent hospitalizations due to her recurrent symptoms. Evaluations included EGD and colonoscopy, but pathology was nondiagnostic. Several abdominal and pelvis CT scans demonstrated bladder edema, pancolitis and terminal ileitis with mucosal hyperenhancement of the bowel and moderate ascites, likely inflammatory. Her gastric emptying study showed hypermotility. Multiple teams, including Rheumatology, Allergy/Immunology, Gastroenterology, Hematology and Surgery were involved. C1 esterase antigen was normal, ruling out hereditary angioedema. PET-CT scan did not show lymphadenopathy or significant inflammation. Full biopsy for definitive diagnosis was deferred due to concerns of decreased healing with an edematous intestine. She was trialed on Icatibant without benefit. Differentials included lupus peritonitis, protein-losing enteropathy, and SS intestinal lymphoma. She was discharged on a trial of empiric high-dose steroids with Rheumatology follow-up. Symptoms recurred with steroid tapering. Her complement levels decreased with flares and increased with treatment. Rituximab was added, leading to steady clinical improvement and reduced hospitalizations.
Discussion: This case highlights the potential for small bowel involvement in SS, an entity rarely reported. While enteritis is well described in lupus, its occurrence in SS is exceptional. The patient’s clinical and radiologic response to steroids and rituximab highlights the autoimmune basis of her enteritis and supports early immunosuppressive therapy in severe or relapsing cases. Gastroenterologists should maintain a high index of suspicion for atypical SS manifestations when evaluating unexplained GI symptoms, particularly in the setting of systemic autoimmune features.

Figure: CT of abdomen and pelvis showing pancolitis, terminal ileitis, and abnormal bladder wall thickening
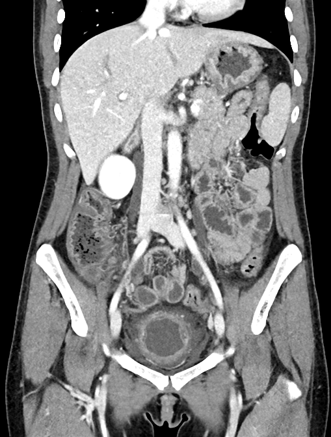
Figure: CT of abdomen and pelvis showing decreased small bowel wall thickening compared to prior study
Disclosures:
Oudai Sahwan indicated no relevant financial relationships.
Fares Jamal indicated no relevant financial relationships.
Amani Elshaer indicated no relevant financial relationships.
Tala Shahin indicated no relevant financial relationships.
Micheal M. Pham indicated no relevant financial relationships.
Oudai Sahwan, MBBS, Fares Jamal, MD, Amani Elshaer, MBBS, Tala B. Shahin, MD, Micheal M. Pham, MD. P4150 - Steroid-Responsive Small Bowel Enteritis in Sjögren’s Syndrome: A Rare Gastrointestinal Manifestation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mayo Clinic, Phoenix, AZ
Introduction: Sjögren’s syndrome (SS) is a chronic autoimmune disease mainly affecting exocrine glands, often presenting with xerostomia and keratoconjunctivitis sicca. Gastrointestinal (GI) involvement is uncommon and typically limited to upper GI tract. Small bowel enteritis is exceedingly rare and more often linked with systemic lupus erythematosus. We present a unique case of SS-associated small bowel enteritis responsive to immunosuppressive therapy.
Case Description/
Methods: This patient was diagnosed with SS in 2018 with positive ANA, RF, SSA antibodies and salivary lip gland biopsy. By 2021, she developed unusual cyclic episodes of nausea, vomiting, and poor oral intake, resulting in significant weight loss and recurrent hospitalizations. She had frequent hospitalizations due to her recurrent symptoms. Evaluations included EGD and colonoscopy, but pathology was nondiagnostic. Several abdominal and pelvis CT scans demonstrated bladder edema, pancolitis and terminal ileitis with mucosal hyperenhancement of the bowel and moderate ascites, likely inflammatory. Her gastric emptying study showed hypermotility. Multiple teams, including Rheumatology, Allergy/Immunology, Gastroenterology, Hematology and Surgery were involved. C1 esterase antigen was normal, ruling out hereditary angioedema. PET-CT scan did not show lymphadenopathy or significant inflammation. Full biopsy for definitive diagnosis was deferred due to concerns of decreased healing with an edematous intestine. She was trialed on Icatibant without benefit. Differentials included lupus peritonitis, protein-losing enteropathy, and SS intestinal lymphoma. She was discharged on a trial of empiric high-dose steroids with Rheumatology follow-up. Symptoms recurred with steroid tapering. Her complement levels decreased with flares and increased with treatment. Rituximab was added, leading to steady clinical improvement and reduced hospitalizations.
Discussion: This case highlights the potential for small bowel involvement in SS, an entity rarely reported. While enteritis is well described in lupus, its occurrence in SS is exceptional. The patient’s clinical and radiologic response to steroids and rituximab highlights the autoimmune basis of her enteritis and supports early immunosuppressive therapy in severe or relapsing cases. Gastroenterologists should maintain a high index of suspicion for atypical SS manifestations when evaluating unexplained GI symptoms, particularly in the setting of systemic autoimmune features.

Figure: CT of abdomen and pelvis showing pancolitis, terminal ileitis, and abnormal bladder wall thickening
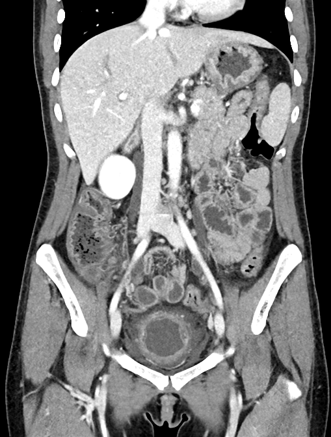
Figure: CT of abdomen and pelvis showing decreased small bowel wall thickening compared to prior study
Disclosures:
Oudai Sahwan indicated no relevant financial relationships.
Fares Jamal indicated no relevant financial relationships.
Amani Elshaer indicated no relevant financial relationships.
Tala Shahin indicated no relevant financial relationships.
Micheal M. Pham indicated no relevant financial relationships.
Oudai Sahwan, MBBS, Fares Jamal, MD, Amani Elshaer, MBBS, Tala B. Shahin, MD, Micheal M. Pham, MD. P4150 - Steroid-Responsive Small Bowel Enteritis in Sjögren’s Syndrome: A Rare Gastrointestinal Manifestation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
