Monday Poster Session
Category: Small Intestine
P4149 - Mimicry in the Gut: IgA Vasculitis Presenting as Crohn’s Like Terminal Ileitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Brittney Shupp, DO (she/her/hers)
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Brittney Shupp, DO1, Monica Dzwonkowski, DO1, Vesselin Tomov, MD1, Kimberly J. Chaput, DO2
1St. Luke's University Health Network, Bethlehem, PA; 2St Luke's Gastroenterology, Center Valley, PA
Introduction: There are many mimickers of inflammatory bowel disease (IBD) which can lead to troubling diagnostic dilemmas. One rare mimicker is IgA vasculitis, an immune-mediated disease that leads to inflammation of the small vessels impacting multiple organ systems. IgA vasculitis is a rare systemic illness, but it is even more uncommon for it to lead to an IBD-type picture. We present a case of a young female who presented with a rash and terminal ileitis from presumed IgA vasculitis.
Case Description/
Methods: A 26-year-old female with a history of IgA nephropathy was evaluated for abdominal pain that had been progressive and developed after childbirth. Pain had been accompanied by arthralgias, extremity swelling, and a nonpruritic and purpuric rash that first appeared on her feet but spread caudally to her trunk and extremities. On initial presentation, her kidney function was stable but C-reactive protein was elevated to 114.6 mg/L. CT abdomen and pelvis revealed moderate thickening of the proximal duodenum along with mild colonic thickening. She underwent a skin biopsy and results were consistent with leukocytoclastic small vessels vasculitis leading to a short course of high dose Prednisone.
Prednisone led to improvement in her rash, but she continued to have abdominal pain and developed rectal bleeding. Bidirectional endoscopy was pursued. Upper endoscopy revealed mild duodenitis. Colonoscopy showed patchy areas of colitis and a severely ulcerated, scarred, and friable terminal ileum (Images A-D). Targeted colon and terminal ileum biopsies revealed ulceration with granulation tissue, cryptitis, and inflammatory exudate.
Although Crohn’s disease was considered, clinical symptoms and endoscopic findings were thought to be secondary to IgA vasculitis. Special immunofluorescence stains of ileal biopsies are still pending. Patient was restarted on Prednisone 60 mg daily which was slowly tapered. Patient overall responded to steroids resulting in disappearance of rash, improvement in clinical symptoms, and resolution of endoscopic findings 3 months later (Image E-F).
Discussion: IgA vasculitis is a rare condition in adults and one that requires a high clinical suspicion to diagnosis. Endoscopic findings will often mimic IBD and obtaining a histologic diagnosis has proven to be challenging. Close evaluation of a patient’s clinical history and presenting symptoms is imperative. Clinicians should maintain a high index of suspicion for IgA vasculitis in patients presenting with a rash and symptoms of IBD.
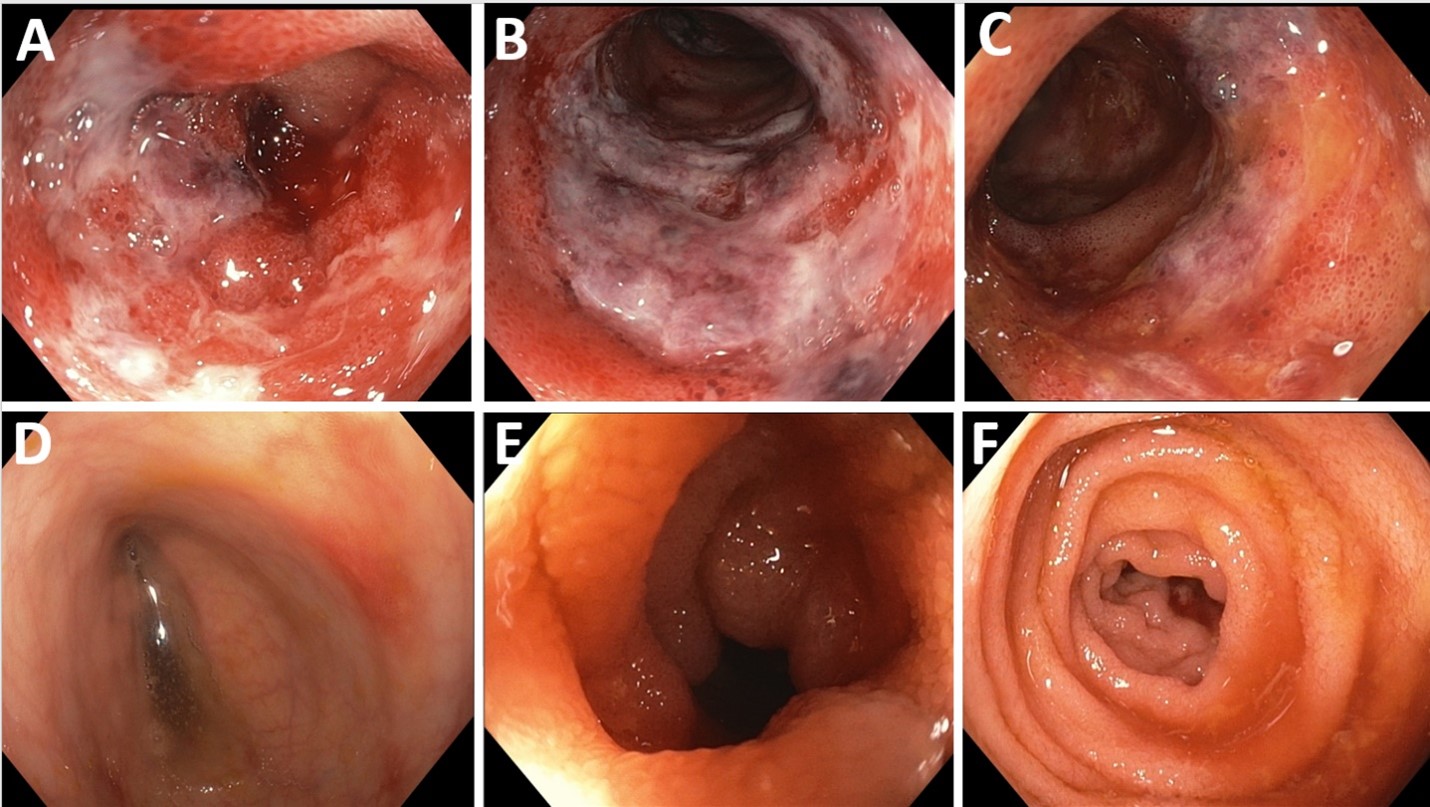
Figure: Image 1: Severely erythematous, ulcerated, and friable mucosa seen throughout the entirety of visualized terminal ileum on presenting colonoscopy (A-C). Focal areas of erythema and erosions seen throughout colon on presenting colonoscopy (D). Healthy appearing terminal ileum with complete resolution of previously identified terminal ileitis on follow up colonoscopy following completion of steroid treatment course (E-F).
Disclosures:
Brittney Shupp indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Vesselin Tomov indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Brittney Shupp, DO1, Monica Dzwonkowski, DO1, Vesselin Tomov, MD1, Kimberly J. Chaput, DO2. P4149 - Mimicry in the Gut: IgA Vasculitis Presenting as Crohn’s Like Terminal Ileitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St Luke's Gastroenterology, Center Valley, PA
Introduction: There are many mimickers of inflammatory bowel disease (IBD) which can lead to troubling diagnostic dilemmas. One rare mimicker is IgA vasculitis, an immune-mediated disease that leads to inflammation of the small vessels impacting multiple organ systems. IgA vasculitis is a rare systemic illness, but it is even more uncommon for it to lead to an IBD-type picture. We present a case of a young female who presented with a rash and terminal ileitis from presumed IgA vasculitis.
Case Description/
Methods: A 26-year-old female with a history of IgA nephropathy was evaluated for abdominal pain that had been progressive and developed after childbirth. Pain had been accompanied by arthralgias, extremity swelling, and a nonpruritic and purpuric rash that first appeared on her feet but spread caudally to her trunk and extremities. On initial presentation, her kidney function was stable but C-reactive protein was elevated to 114.6 mg/L. CT abdomen and pelvis revealed moderate thickening of the proximal duodenum along with mild colonic thickening. She underwent a skin biopsy and results were consistent with leukocytoclastic small vessels vasculitis leading to a short course of high dose Prednisone.
Prednisone led to improvement in her rash, but she continued to have abdominal pain and developed rectal bleeding. Bidirectional endoscopy was pursued. Upper endoscopy revealed mild duodenitis. Colonoscopy showed patchy areas of colitis and a severely ulcerated, scarred, and friable terminal ileum (Images A-D). Targeted colon and terminal ileum biopsies revealed ulceration with granulation tissue, cryptitis, and inflammatory exudate.
Although Crohn’s disease was considered, clinical symptoms and endoscopic findings were thought to be secondary to IgA vasculitis. Special immunofluorescence stains of ileal biopsies are still pending. Patient was restarted on Prednisone 60 mg daily which was slowly tapered. Patient overall responded to steroids resulting in disappearance of rash, improvement in clinical symptoms, and resolution of endoscopic findings 3 months later (Image E-F).
Discussion: IgA vasculitis is a rare condition in adults and one that requires a high clinical suspicion to diagnosis. Endoscopic findings will often mimic IBD and obtaining a histologic diagnosis has proven to be challenging. Close evaluation of a patient’s clinical history and presenting symptoms is imperative. Clinicians should maintain a high index of suspicion for IgA vasculitis in patients presenting with a rash and symptoms of IBD.
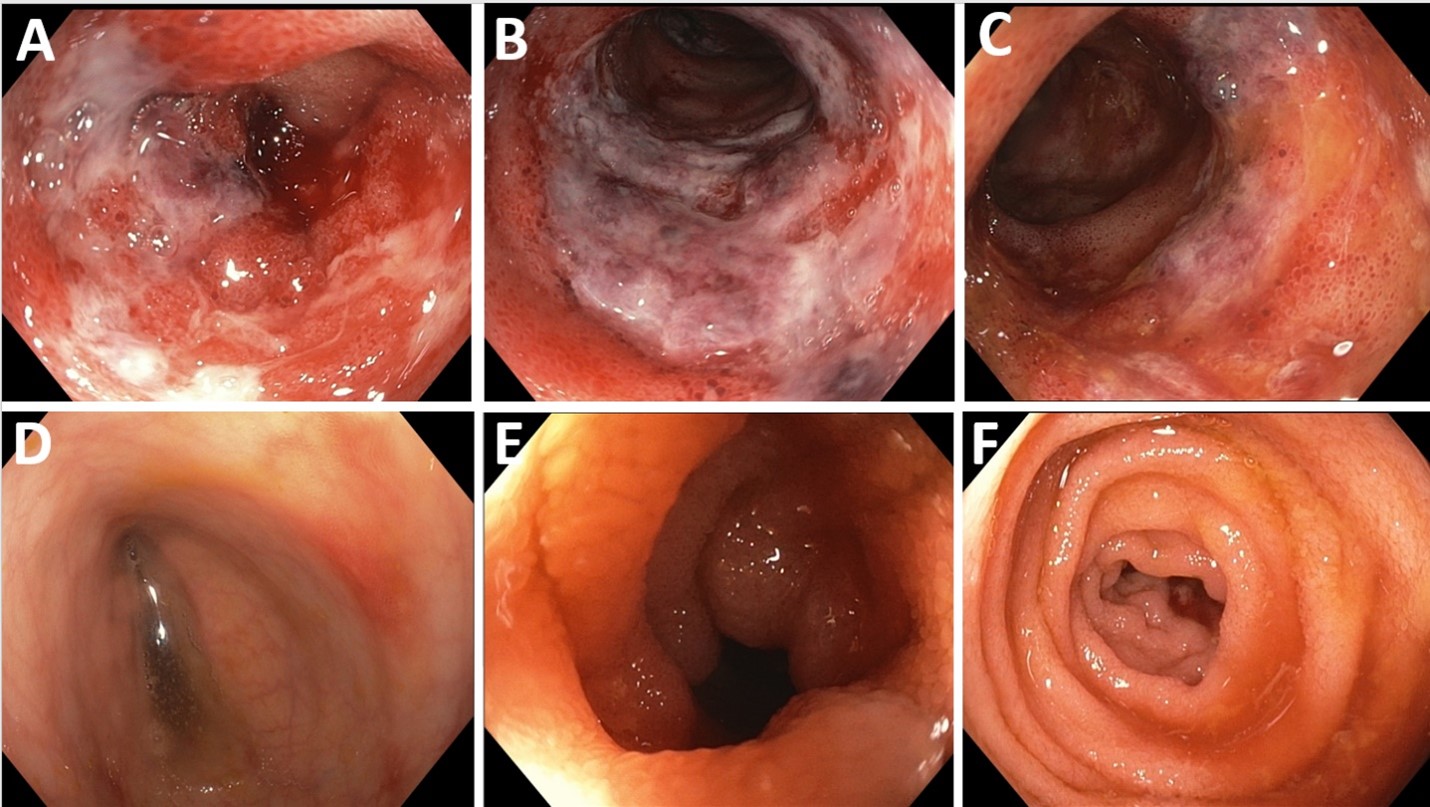
Figure: Image 1: Severely erythematous, ulcerated, and friable mucosa seen throughout the entirety of visualized terminal ileum on presenting colonoscopy (A-C). Focal areas of erythema and erosions seen throughout colon on presenting colonoscopy (D). Healthy appearing terminal ileum with complete resolution of previously identified terminal ileitis on follow up colonoscopy following completion of steroid treatment course (E-F).
Disclosures:
Brittney Shupp indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Vesselin Tomov indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Brittney Shupp, DO1, Monica Dzwonkowski, DO1, Vesselin Tomov, MD1, Kimberly J. Chaput, DO2. P4149 - Mimicry in the Gut: IgA Vasculitis Presenting as Crohn’s Like Terminal Ileitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
