Monday Poster Session
Category: Small Intestine
A Rare Case of Invasive <i>Candida</i> Infection Leading to Duodenitis in an Immunocompetent Host
P4139 - A Rare Case of Invasive Candida Infection Leading to Duodenitis in an Immunocompetent Host
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KV
Kirsten Valaas, DO
Wright State University
Dayton, OH
Presenting Author(s)
Yesol Oh, MD1, Erin Currey, MD2, Kirsten Valaas, DO1, Rawan Aljaras, MD3, Sangeeta Agrawal, MD3
1Wright State University, Dayton, OH; 2Wright Patterson Medical Center, Dayton, OH; 3Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Invasive fungal infections of the gastrointestinal (GI) tract are rare in immunocompetent individuals. Among these, Candida and Aspergillus species are the most commonly implicated pathogens. Invasive GI fungal infections are typically associated with immunocompromised states, including HIV infection, chemotherapy, solid organ or hematopoietic stem cell transplantation, and primary immunodeficiencies. We present a case of pigmented duodenal ulcer caused by Candida species, likely secondary to recurrent bowel obstructions and ileus in the context of known intra-abdominal adhesions.
Case Description/
Methods: A 60-year-old female initially presented to the emergency department (ED) with intractable abdominal pain, diarrhea, nausea, and vomiting. Her medical history was significant for peptic ulcer disease, prior Helicobacter Pylori infection with confirmed eradication, and coronary artery disease. Computed tomography (CT) of the abdomen showed a partial small bowel obstruction (SBO), and the patient subsequently underwent exploratory laparoscopy with lysis of adhesions from a prior cholecystectomy. The surgery was completed successfully without major complications. However, following surgery, the patient was admitted multiple times for recurrent episodes of SBO, which was treated non-surgically. Esophagogastroduodenoscopy (EGD) showed a 6 cm duodenal ulcer in the second portion of the duodenum (D2) with a pigmented spot causing partial duodenal obstruction. Biopsies were obtained, and histopathology was positive for fungal organisms morphologically consistent with Candida species. The patient was started on a 3-week course of fluconazole therapy for Candida duodenitis, with repeat EGD planned in 8 weeks.
Discussion: Duodenal ulcers are common findings on EGD, with the majority attributed to either non-steroidal anti-inflammatory drug use or Helicobacter Pylori infection.1 The GI tract is equipped with a robust innate and adaptive immune system that generally offers significant protection against invasive pathogens. The primary pathogenic mechanism for most duodenal ulcers involves mucosal injury, either through mechanical disruption or prostaglandin dysregulation.1 In this patient, bowel obstruction due to intra-abdominal adhesions likely contributed to mucosal injury through bile stasis, thereby predisposing the duodenum to invasive fungal infection.
References:
1. Ocasio Quinones GA, Woolf A. Duodenal Ulcer. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
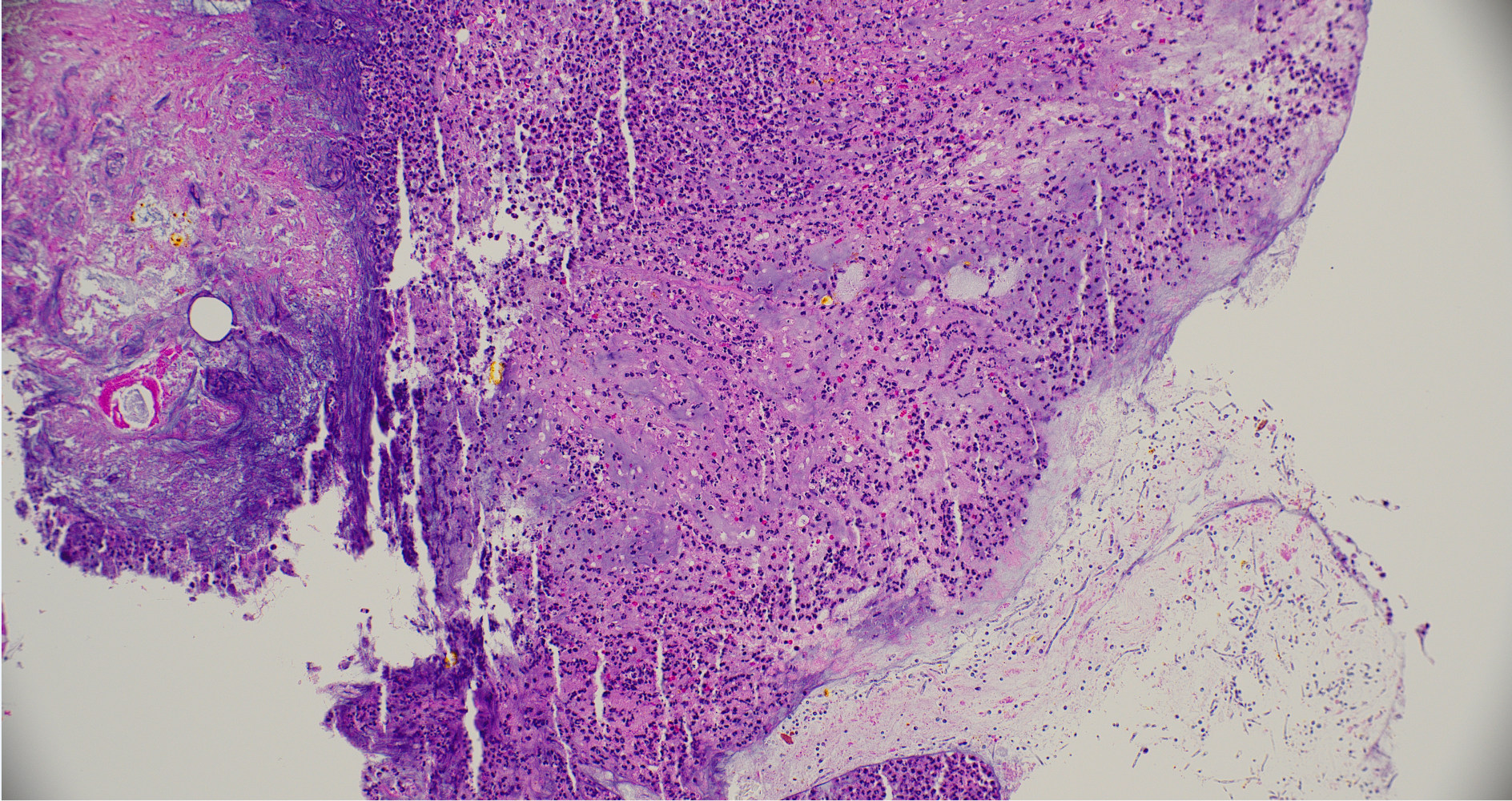
Figure: GMS stain, positive for fungal organisms, morphologically consistent with Candida species
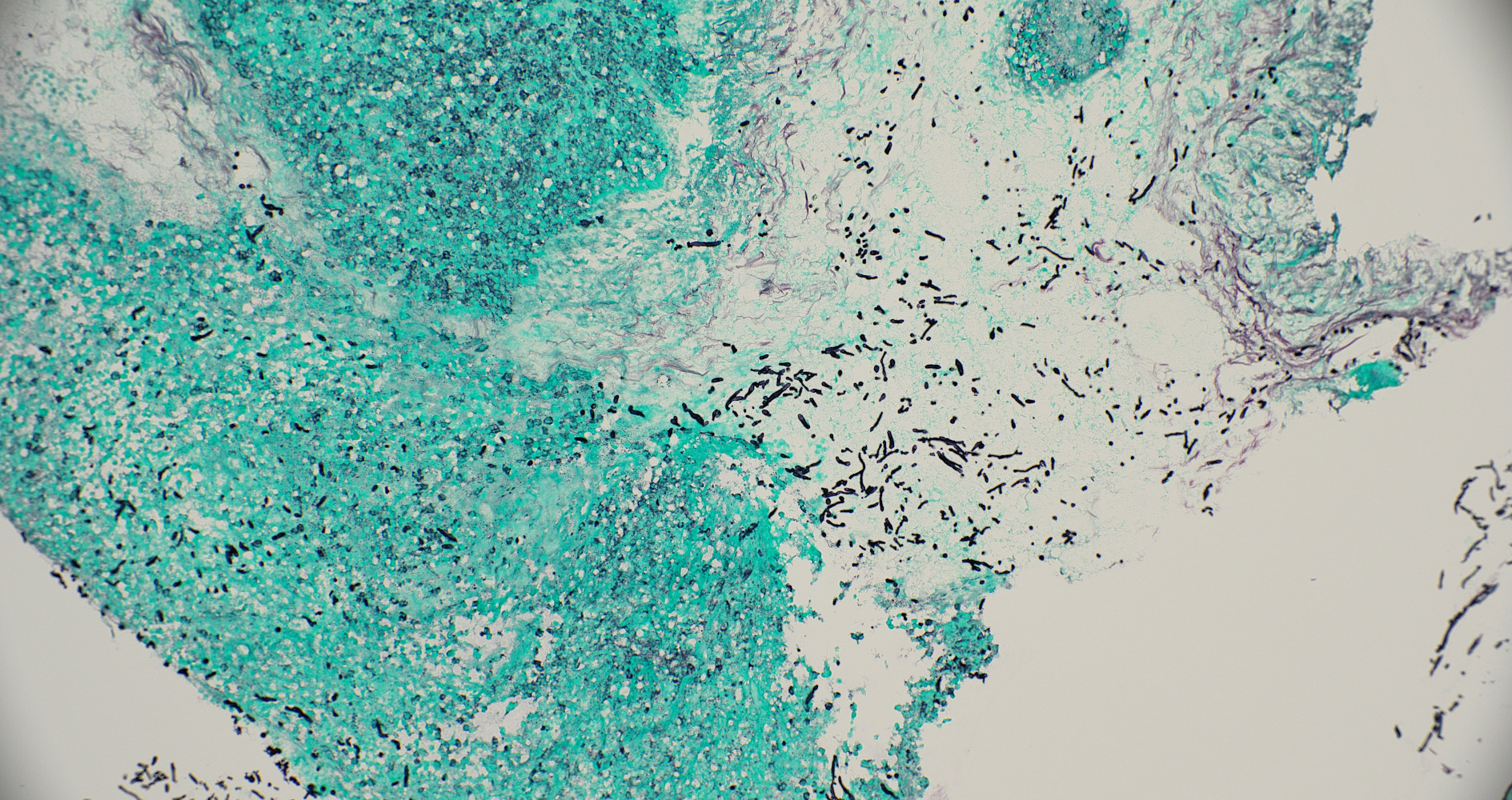
Figure: H&E Stain, positive for fungal organisms morphologically consistent with Candida species
Disclosures:
Yesol Oh indicated no relevant financial relationships.
Erin Currey indicated no relevant financial relationships.
Kirsten Valaas indicated no relevant financial relationships.
Rawan Aljaras indicated no relevant financial relationships.
Sangeeta Agrawal indicated no relevant financial relationships.
Yesol Oh, MD1, Erin Currey, MD2, Kirsten Valaas, DO1, Rawan Aljaras, MD3, Sangeeta Agrawal, MD3. P4139 - A Rare Case of Invasive <i>Candida</i> Infection Leading to Duodenitis in an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright State University, Dayton, OH; 2Wright Patterson Medical Center, Dayton, OH; 3Wright State University Boonshoft School of Medicine, Dayton, OH
Introduction: Invasive fungal infections of the gastrointestinal (GI) tract are rare in immunocompetent individuals. Among these, Candida and Aspergillus species are the most commonly implicated pathogens. Invasive GI fungal infections are typically associated with immunocompromised states, including HIV infection, chemotherapy, solid organ or hematopoietic stem cell transplantation, and primary immunodeficiencies. We present a case of pigmented duodenal ulcer caused by Candida species, likely secondary to recurrent bowel obstructions and ileus in the context of known intra-abdominal adhesions.
Case Description/
Methods: A 60-year-old female initially presented to the emergency department (ED) with intractable abdominal pain, diarrhea, nausea, and vomiting. Her medical history was significant for peptic ulcer disease, prior Helicobacter Pylori infection with confirmed eradication, and coronary artery disease. Computed tomography (CT) of the abdomen showed a partial small bowel obstruction (SBO), and the patient subsequently underwent exploratory laparoscopy with lysis of adhesions from a prior cholecystectomy. The surgery was completed successfully without major complications. However, following surgery, the patient was admitted multiple times for recurrent episodes of SBO, which was treated non-surgically. Esophagogastroduodenoscopy (EGD) showed a 6 cm duodenal ulcer in the second portion of the duodenum (D2) with a pigmented spot causing partial duodenal obstruction. Biopsies were obtained, and histopathology was positive for fungal organisms morphologically consistent with Candida species. The patient was started on a 3-week course of fluconazole therapy for Candida duodenitis, with repeat EGD planned in 8 weeks.
Discussion: Duodenal ulcers are common findings on EGD, with the majority attributed to either non-steroidal anti-inflammatory drug use or Helicobacter Pylori infection.1 The GI tract is equipped with a robust innate and adaptive immune system that generally offers significant protection against invasive pathogens. The primary pathogenic mechanism for most duodenal ulcers involves mucosal injury, either through mechanical disruption or prostaglandin dysregulation.1 In this patient, bowel obstruction due to intra-abdominal adhesions likely contributed to mucosal injury through bile stasis, thereby predisposing the duodenum to invasive fungal infection.
References:
1. Ocasio Quinones GA, Woolf A. Duodenal Ulcer. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
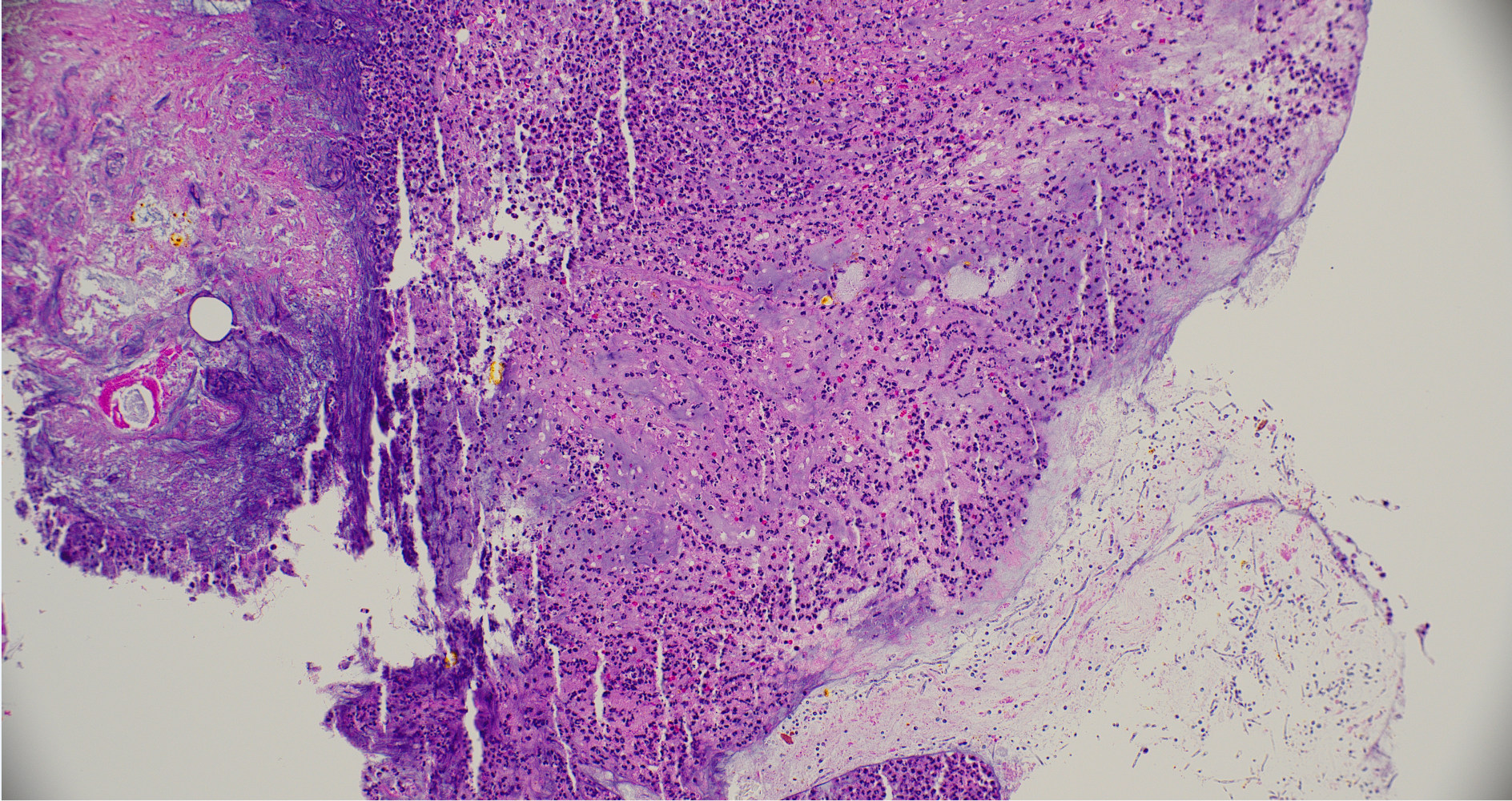
Figure: GMS stain, positive for fungal organisms, morphologically consistent with Candida species
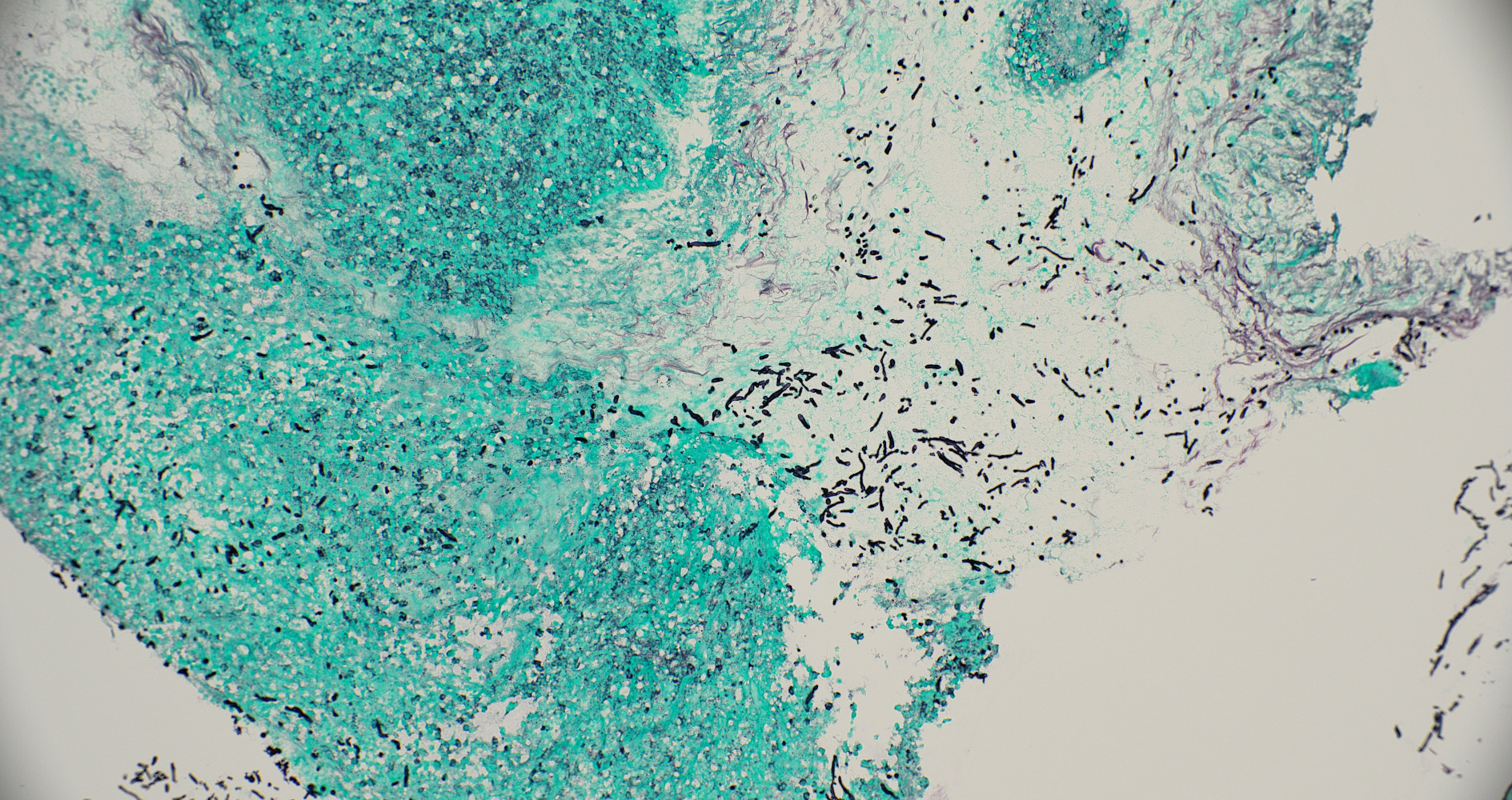
Figure: H&E Stain, positive for fungal organisms morphologically consistent with Candida species
Disclosures:
Yesol Oh indicated no relevant financial relationships.
Erin Currey indicated no relevant financial relationships.
Kirsten Valaas indicated no relevant financial relationships.
Rawan Aljaras indicated no relevant financial relationships.
Sangeeta Agrawal indicated no relevant financial relationships.
Yesol Oh, MD1, Erin Currey, MD2, Kirsten Valaas, DO1, Rawan Aljaras, MD3, Sangeeta Agrawal, MD3. P4139 - A Rare Case of Invasive <i>Candida</i> Infection Leading to Duodenitis in an Immunocompetent Host, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
