Monday Poster Session
Category: Small Intestine
P4116 - Unmasking a Duodenal Lipoma: When Benign Looks Malignant
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AS
Apurva Pravin Shrigiriwar, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Apurva Shrigiriwar, MD1, Bishr Swar, MD2, Ashlee Barr, 1, Shruti Mony, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma Health Sciences Center, Oklahoma CIty, OK
Introduction: Ulcerated duodenal lesions are uncommon and often raise concern for malignancy, particularly when they appear to be fungating or ulcerative during endoscopy. Benign lesions, such as lipomas, can mimic this appearance. Endoscopic ultrasound (EUS) plays a critical role in characterizing such lesions and guiding appropriate therapy.
Case Description/
Methods: A 79-year-old male was referred for an esophagogastroduodenoscopy (EGD) for evaluation of melena. EGD demonstrated a fungating, infiltrative mass with an ulcerated base in the second part of the duodenum (D2) opposite the ampulla (Figure 1A). The ulcer base was clear without a visible vessel (Figure 1B). The mass was biopsied and sent to pathology. Based on the ulcerated appearance of the mass, the likelihood of malignancy was presumed to be high. Therefore, CT abdomen and pelvis was obtained which revealed a 2.3cm well-circumscribed fatty lesion within the duodenal wall likely representing a lipoma (Figure 2 A, B). Pathology revealed duodenal mucosal fragments and fibrofatty tissue with inflammation and reactive changes. Given the atypical, ulcerated appearance, a liposarcoma component could not be excluded, hence, we decided to perform a repeat EGD with endoscopic ultrasound (EUS). EUS revealed a 20 x 35mm hyperechoic mass arising from the submucosal layer with well-defined borders (Figure 3). Since EUS images were highly suggestive of a lipomatous lesion in the setting of symptomatic anemia, a decision was made to perform polyloop assisted endoscopic mucosal resection (EMR). A detachable polyloop was deployed at the base of the lesion for tamponade effect followed by resection using a 33mm captivator snare (Figure 4A). Successful EMR was performed without evidence of residual polyp at the resection site (Figure 4B). Pathology was suggestive of submucosal lipoma. The overlying duodenum had fibrofatty replacement with the presence of granulation tissue and ulceration. Additionally, immunohistochemical stain was positive for pan-keratin highlights in the epithelium.
Discussion: Symptomatic, ulcerated duodenal lipomas are rare and may appear malignant on endoscopy. An EUS should be considered to rule out a liposarcomal component followed by mucosal resection for symptomatic relief.
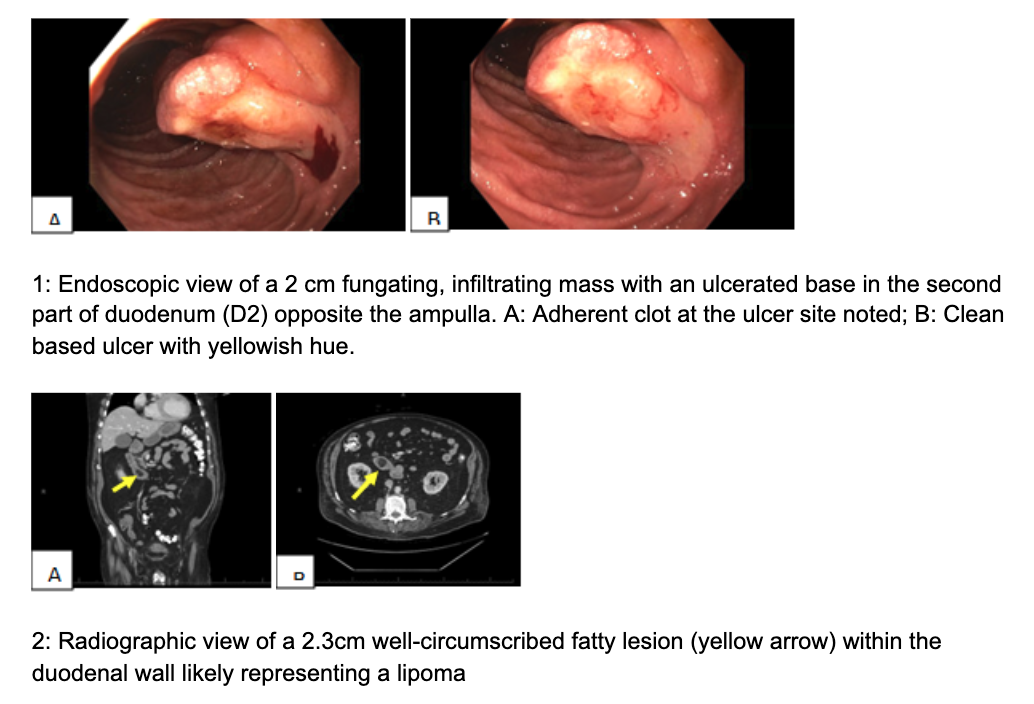
Figure: Figure 1: Endoscopic view of a 2 cm fungating, infiltrating mass with an ulcerated base in the second part of duodenum (D2) opposite the ampulla. A: Adherent clot at the ulcer site noted; B: Clean based ulcer with yellowish hue. Figure 2: Radiographic view of a 2.3cm well-circumscribed fatty lesion (yellow arrow) within the duodenal wall likely representing a lipoma
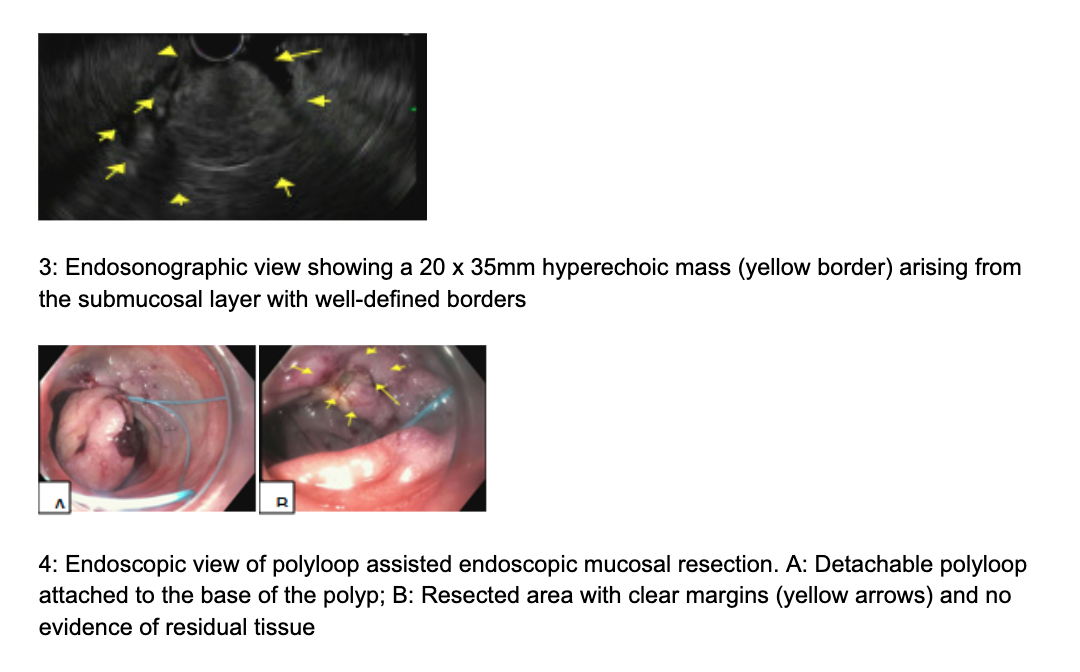
Figure: Figure 3: Endosonographic view showing a 20 x 35mm hyperechoic mass (yellow border) arising from the submucosal layer with well-defined borders. Figure 4: Endoscopic view of polyloop-assisted endoscopic mucosal resection. A: Detachable polyloop attached to the base of the polyp; B: Resected area with clear margins (yellow arrows) and no evidence of residual tissue
Disclosures:
Apurva Shrigiriwar indicated no relevant financial relationships.
Bishr Swar indicated no relevant financial relationships.
Ashlee Barr indicated no relevant financial relationships.
Shruti Mony indicated no relevant financial relationships.
Apurva Shrigiriwar, MD1, Bishr Swar, MD2, Ashlee Barr, 1, Shruti Mony, MD1. P4116 - Unmasking a Duodenal Lipoma: When Benign Looks Malignant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma Health Sciences Center, Oklahoma CIty, OK
Introduction: Ulcerated duodenal lesions are uncommon and often raise concern for malignancy, particularly when they appear to be fungating or ulcerative during endoscopy. Benign lesions, such as lipomas, can mimic this appearance. Endoscopic ultrasound (EUS) plays a critical role in characterizing such lesions and guiding appropriate therapy.
Case Description/
Methods: A 79-year-old male was referred for an esophagogastroduodenoscopy (EGD) for evaluation of melena. EGD demonstrated a fungating, infiltrative mass with an ulcerated base in the second part of the duodenum (D2) opposite the ampulla (Figure 1A). The ulcer base was clear without a visible vessel (Figure 1B). The mass was biopsied and sent to pathology. Based on the ulcerated appearance of the mass, the likelihood of malignancy was presumed to be high. Therefore, CT abdomen and pelvis was obtained which revealed a 2.3cm well-circumscribed fatty lesion within the duodenal wall likely representing a lipoma (Figure 2 A, B). Pathology revealed duodenal mucosal fragments and fibrofatty tissue with inflammation and reactive changes. Given the atypical, ulcerated appearance, a liposarcoma component could not be excluded, hence, we decided to perform a repeat EGD with endoscopic ultrasound (EUS). EUS revealed a 20 x 35mm hyperechoic mass arising from the submucosal layer with well-defined borders (Figure 3). Since EUS images were highly suggestive of a lipomatous lesion in the setting of symptomatic anemia, a decision was made to perform polyloop assisted endoscopic mucosal resection (EMR). A detachable polyloop was deployed at the base of the lesion for tamponade effect followed by resection using a 33mm captivator snare (Figure 4A). Successful EMR was performed without evidence of residual polyp at the resection site (Figure 4B). Pathology was suggestive of submucosal lipoma. The overlying duodenum had fibrofatty replacement with the presence of granulation tissue and ulceration. Additionally, immunohistochemical stain was positive for pan-keratin highlights in the epithelium.
Discussion: Symptomatic, ulcerated duodenal lipomas are rare and may appear malignant on endoscopy. An EUS should be considered to rule out a liposarcomal component followed by mucosal resection for symptomatic relief.
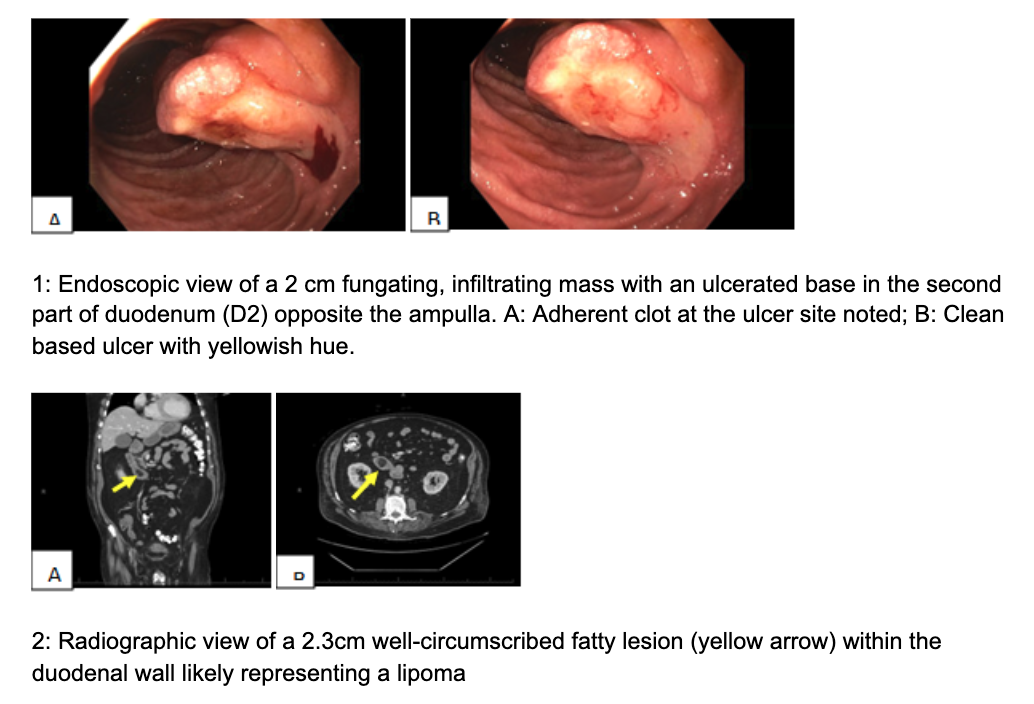
Figure: Figure 1: Endoscopic view of a 2 cm fungating, infiltrating mass with an ulcerated base in the second part of duodenum (D2) opposite the ampulla. A: Adherent clot at the ulcer site noted; B: Clean based ulcer with yellowish hue. Figure 2: Radiographic view of a 2.3cm well-circumscribed fatty lesion (yellow arrow) within the duodenal wall likely representing a lipoma
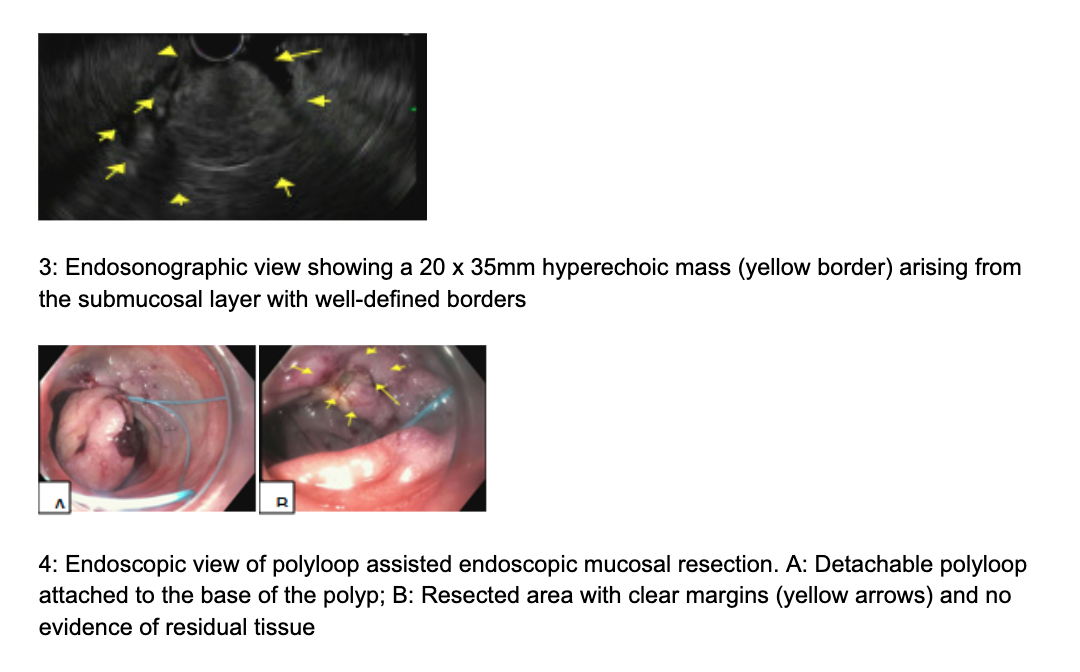
Figure: Figure 3: Endosonographic view showing a 20 x 35mm hyperechoic mass (yellow border) arising from the submucosal layer with well-defined borders. Figure 4: Endoscopic view of polyloop-assisted endoscopic mucosal resection. A: Detachable polyloop attached to the base of the polyp; B: Resected area with clear margins (yellow arrows) and no evidence of residual tissue
Disclosures:
Apurva Shrigiriwar indicated no relevant financial relationships.
Bishr Swar indicated no relevant financial relationships.
Ashlee Barr indicated no relevant financial relationships.
Shruti Mony indicated no relevant financial relationships.
Apurva Shrigiriwar, MD1, Bishr Swar, MD2, Ashlee Barr, 1, Shruti Mony, MD1. P4116 - Unmasking a Duodenal Lipoma: When Benign Looks Malignant, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
