Monday Poster Session
Category: Small Intestine
P4114 - Unmasking the Connection: Collagenous Enteritis, AVMs, and Iron Deficiency Anemia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kristie Liao, DO
University of Tennessee Health Science Center
Chattanooga, TN
Presenting Author(s)
Kristie Liao, DO, Christopher Butler, DO, Priya Vijayvargiya, MD
University of Tennessee Health Science Center, Chattanooga, TN
Introduction: Collagenous enteritis is a rare small intestinal disorder characterized by a thickened subepithelial collagen band accompanied by varying degrees of villous atrophy and chronic mucosal inflammation. Patients typically present with chronic diarrhea, malabsorption, and weight loss. Its pathology is not fully understood; however it is thought to be associated with immune-mediated mechanisms including celiac disease, autoimmune conditions, and certain medications.
Case Description/
Methods: Here, we present a 79 year old male with recurrent iron deficiency anemia (IDA), GERD, and bladder cancer status post cystoprostatectomy who presented with fatigue and dyspnea on exertion. He had been taking ferrous sulfate and vitamin C every other day for a few years with no improvement in his IDA. He endorsed occasional diarrhea, but denied dysphagia, melena, hematochezia, or weight loss. He underwent a video capsule endoscopy (VCE) that revealed granular and edematous mucosa within the small intestine for up to 20% of the small bowel transit time (SBTT), and multiple nonbleeding arteriovenous malformations (AVMs) noted from 4-18% SBTT (Figure A). A small bowel enteroscopy was performed, revealing diffuse moderate mucosal changes characterized by atrophy, congestion, and significant granularity in the second and third portion of the duodenum and jejunum (Figure B, Figure C) as well as a few angiodysplastic lesions that were treated with argon plasma coagulation (APC). Biopsies of the duodenum and jejunum revealed mucosa with shortened villi, mucosal erosion, and patchy thickening of the subepithelial collagen layer (Figure D, Figure E). Collectively, these findings were all consistent with a diagnosis of collagenous enteritis. His vitamin B12 level was normal and serology for celiac sprue was negative.
Discussion: This rare case illustrates a unique presentation of small bowel collagenous enteritis, ultimately explaining the patient’s recurrent IDA that was refractory to oral iron supplementation. Although treatment with corticosteroids was planned to alleviate his symptoms, the patient was unfortunately lost to follow up. While collagenous enteritis is an exceedingly uncommon diagnosis, it remains an important consideration in the differential for patients presenting with unexplained malabsorption and persistent IDA.
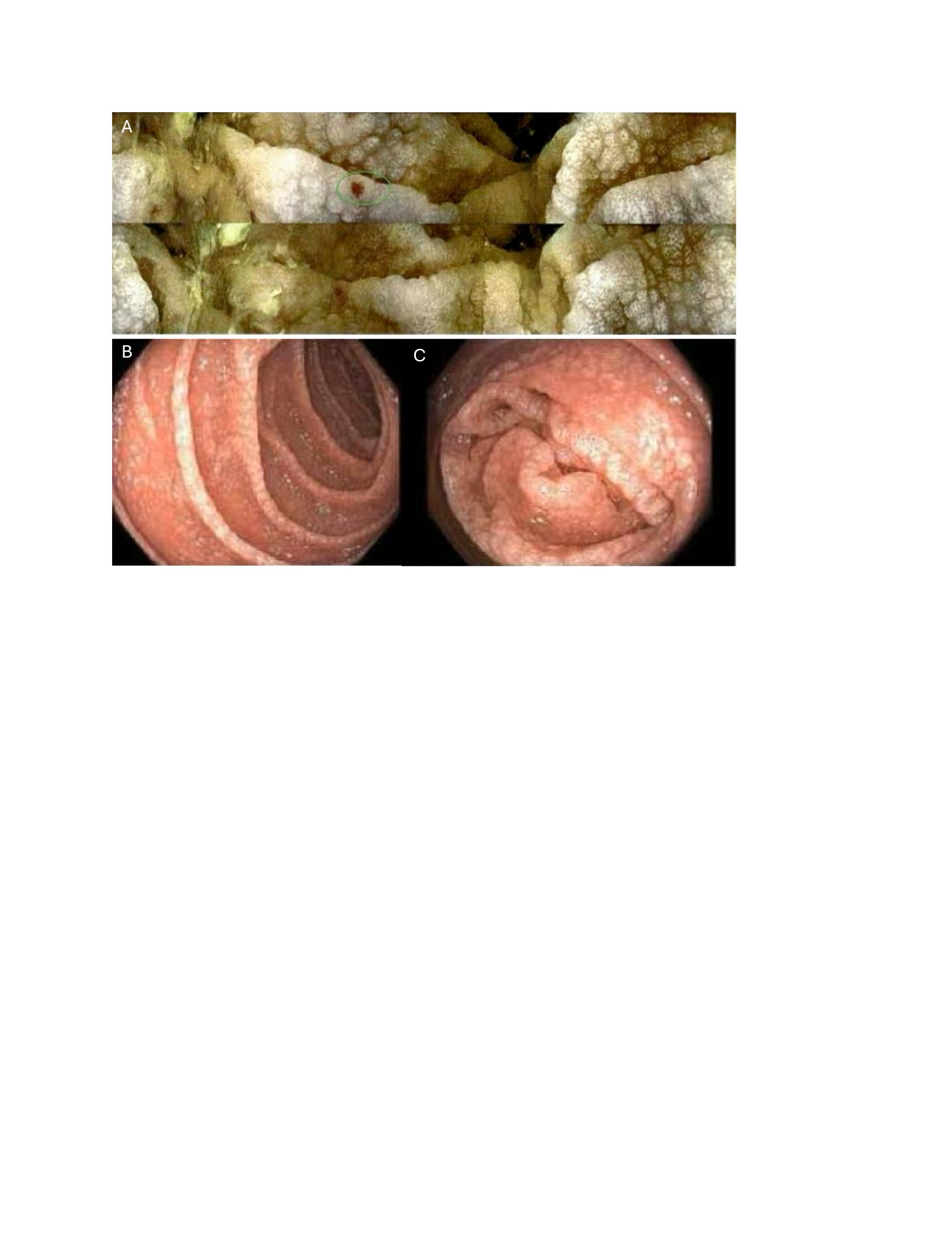
Figure: FIgure A: Video capsule endoscopy revealing granular, edematous mucosa within the small intestine with associated arteriovenous malformation (circled)
Figure B, C: Small bowel enteroscopy photos revealing mucosal atrophy, congestion, and significant granularity in the duodenum & jejunum
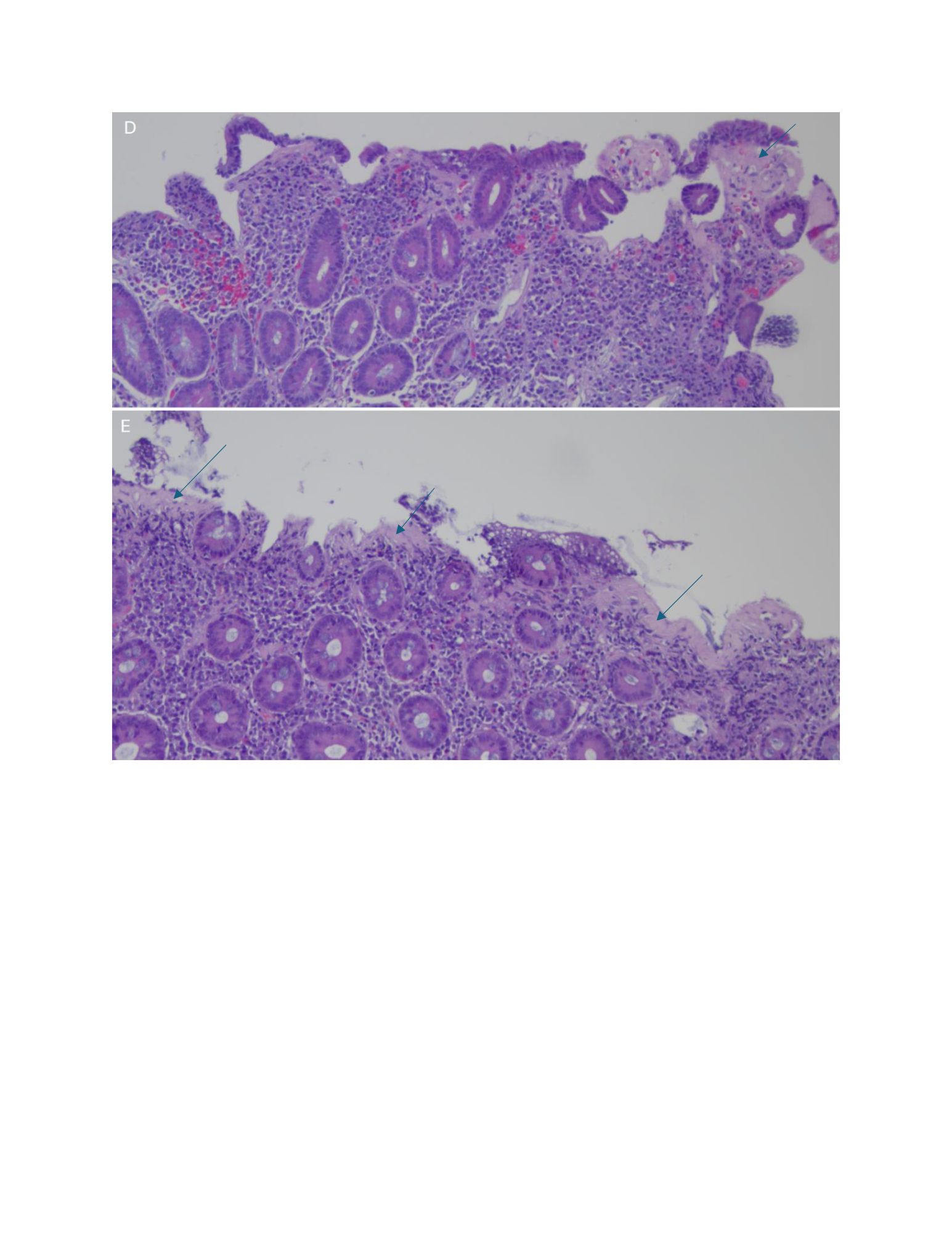
Figure: FIgure D, E: H&E stain of duodenum and jejunum with shortened villi, mucosal erosion, and patchy thickening of the subepithelial collagen layer (shown with arrows)
Disclosures:
Kristie Liao indicated no relevant financial relationships.
Christopher Butler indicated no relevant financial relationships.
Priya Vijayvargiya indicated no relevant financial relationships.
Kristie Liao, DO, Christopher Butler, DO, Priya Vijayvargiya, MD. P4114 - Unmasking the Connection: Collagenous Enteritis, AVMs, and Iron Deficiency Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Tennessee Health Science Center, Chattanooga, TN
Introduction: Collagenous enteritis is a rare small intestinal disorder characterized by a thickened subepithelial collagen band accompanied by varying degrees of villous atrophy and chronic mucosal inflammation. Patients typically present with chronic diarrhea, malabsorption, and weight loss. Its pathology is not fully understood; however it is thought to be associated with immune-mediated mechanisms including celiac disease, autoimmune conditions, and certain medications.
Case Description/
Methods: Here, we present a 79 year old male with recurrent iron deficiency anemia (IDA), GERD, and bladder cancer status post cystoprostatectomy who presented with fatigue and dyspnea on exertion. He had been taking ferrous sulfate and vitamin C every other day for a few years with no improvement in his IDA. He endorsed occasional diarrhea, but denied dysphagia, melena, hematochezia, or weight loss. He underwent a video capsule endoscopy (VCE) that revealed granular and edematous mucosa within the small intestine for up to 20% of the small bowel transit time (SBTT), and multiple nonbleeding arteriovenous malformations (AVMs) noted from 4-18% SBTT (Figure A). A small bowel enteroscopy was performed, revealing diffuse moderate mucosal changes characterized by atrophy, congestion, and significant granularity in the second and third portion of the duodenum and jejunum (Figure B, Figure C) as well as a few angiodysplastic lesions that were treated with argon plasma coagulation (APC). Biopsies of the duodenum and jejunum revealed mucosa with shortened villi, mucosal erosion, and patchy thickening of the subepithelial collagen layer (Figure D, Figure E). Collectively, these findings were all consistent with a diagnosis of collagenous enteritis. His vitamin B12 level was normal and serology for celiac sprue was negative.
Discussion: This rare case illustrates a unique presentation of small bowel collagenous enteritis, ultimately explaining the patient’s recurrent IDA that was refractory to oral iron supplementation. Although treatment with corticosteroids was planned to alleviate his symptoms, the patient was unfortunately lost to follow up. While collagenous enteritis is an exceedingly uncommon diagnosis, it remains an important consideration in the differential for patients presenting with unexplained malabsorption and persistent IDA.
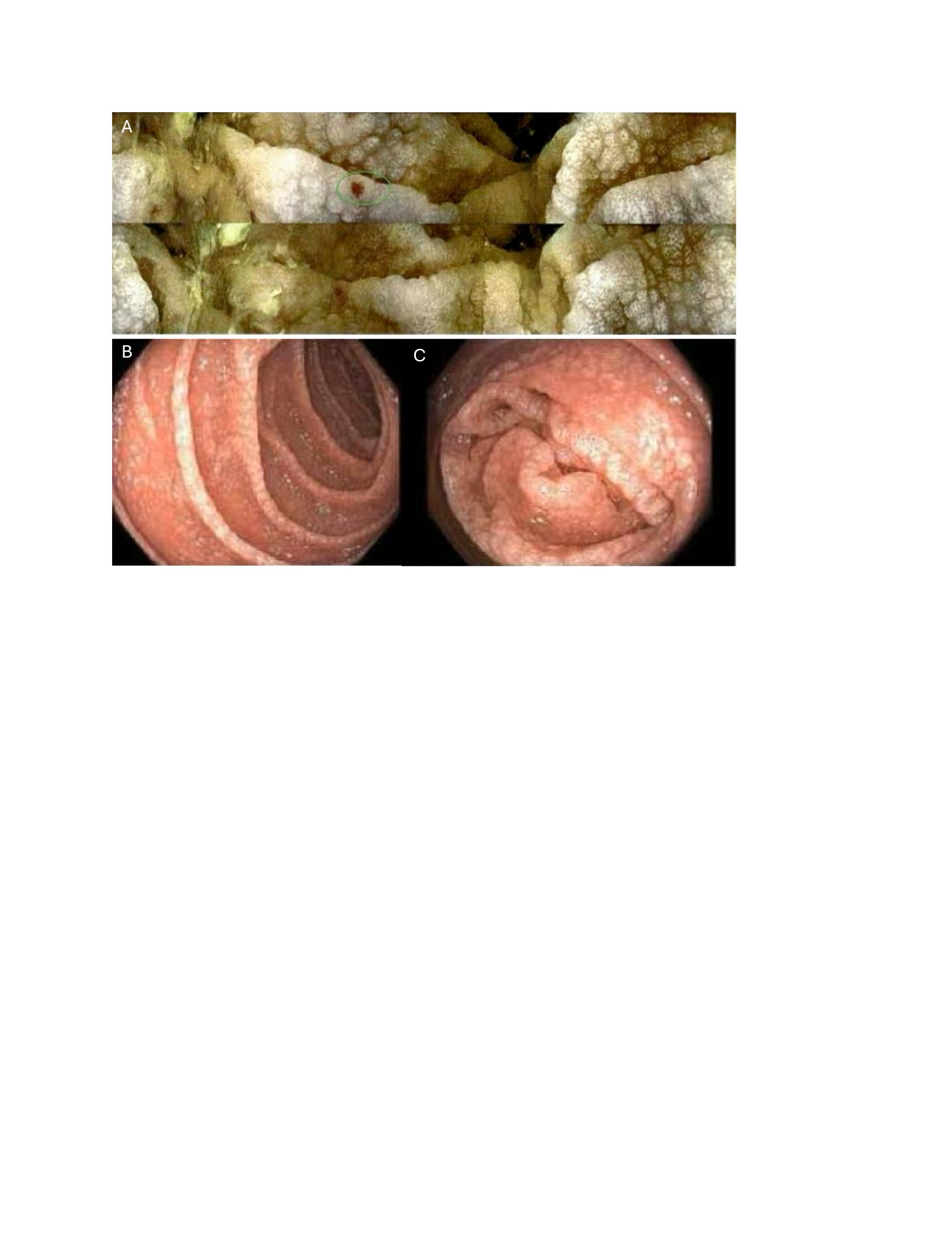
Figure: FIgure A: Video capsule endoscopy revealing granular, edematous mucosa within the small intestine with associated arteriovenous malformation (circled)
Figure B, C: Small bowel enteroscopy photos revealing mucosal atrophy, congestion, and significant granularity in the duodenum & jejunum
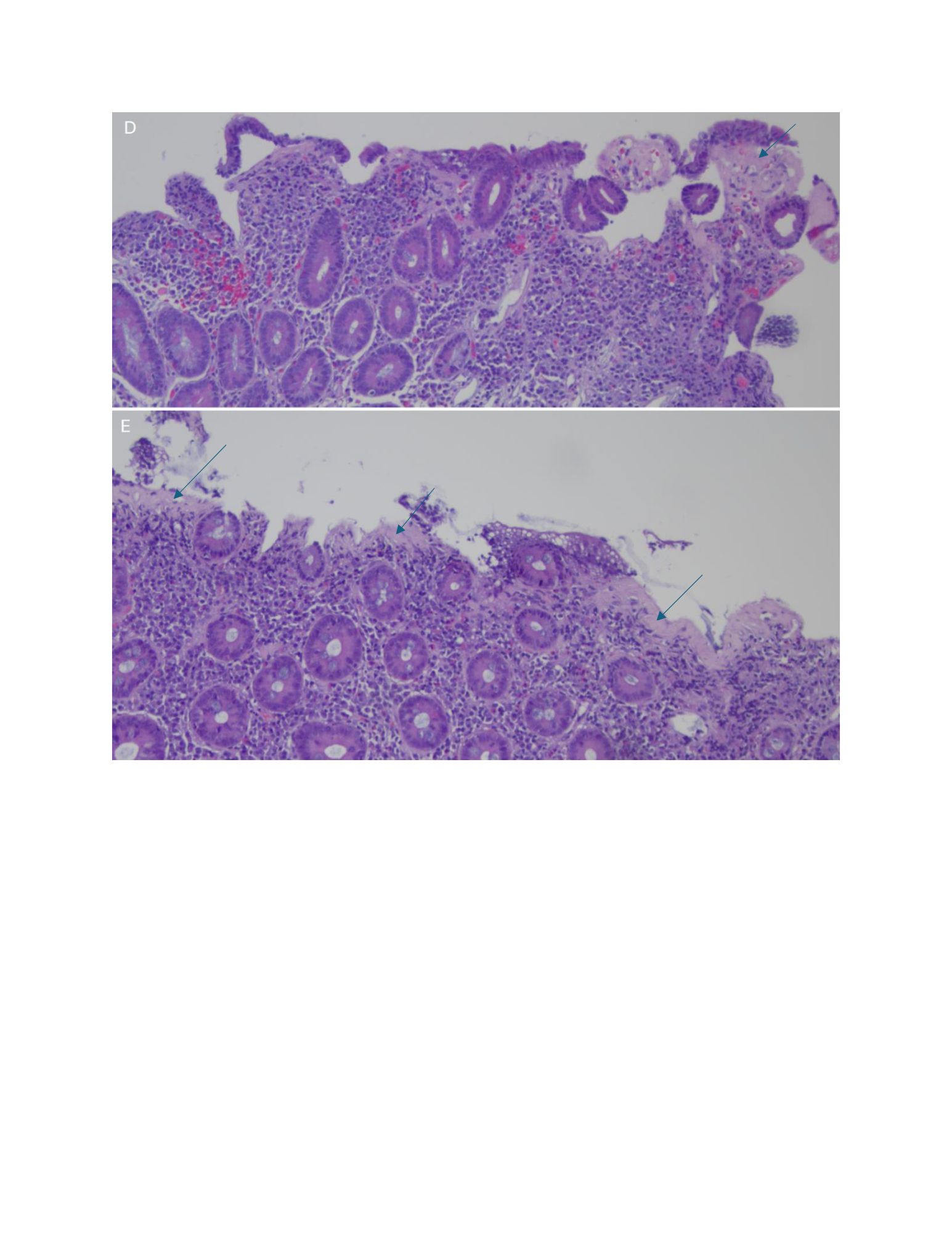
Figure: FIgure D, E: H&E stain of duodenum and jejunum with shortened villi, mucosal erosion, and patchy thickening of the subepithelial collagen layer (shown with arrows)
Disclosures:
Kristie Liao indicated no relevant financial relationships.
Christopher Butler indicated no relevant financial relationships.
Priya Vijayvargiya indicated no relevant financial relationships.
Kristie Liao, DO, Christopher Butler, DO, Priya Vijayvargiya, MD. P4114 - Unmasking the Connection: Collagenous Enteritis, AVMs, and Iron Deficiency Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
