Monday Poster Session
Category: Small Intestine
P4112 - CMV Duodenitis Mimicking Malignancy: First Reported Case of Obstructive Pseudotumor in CVID Treated Endoscopically
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pratiksha Moliya, MD
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Pratiksha Moliya, MD, Natapat Chaisidhivej, MD, Pauline Yasmeh, MD, Faruq Pradhan, MBBCh, Ishfaq Bhat, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: CMV GI infection is common in immunocompromised patients, but isolated CMV pseudotumors are rare, with < 25 cases reported. Most involve the colon (~40%), stomach (~20%), and other GI sites, duodenal involvement is extremely rare (< 1%). This is the first reported case of CMV duodenitis pseudotumor in a CVID patient.
Case Description/
Methods: A 66-year-old male with CVID and cirrhosis underwent screening EGD, revealing a fungating duodenal mass due to CMV duodenitis, treated with ganciclovir. A month later, he presented with vomiting, dysphagia, weight loss & elevated LFTs (AST 65, ALT 74, ALP 552, TBili 1.1). CT showed a CBD filling defect and duodenal mass with omental caking (biopsy negative for malignancy). LFTs worsened (AST 326, ALT 217, ALP 1487, TBili 26). MRCP deferred due to claustrophobia. Liver biopsy revealed interface hepatitis, likely viral or DILI. Tumor markers, hepatitis panel, and AMA were negative, CMV viremia also ruled out. EGD showed duodenal ulceration with high-grade narrowing. Balloon dilation to 13.5 mm disrupted the stricture, but the scope could not pass. Biopsies confirmed CMV duodenitis. He received ganciclovir/valganciclovir for 4 weeks, with mild improvement in symptoms and LFTs. A month later, EGD showed persistent stricture, LAMS was placed. At follow-up, mild narrowing remained, prompting a second LAMS. Three months later, EGD showed stricture improvement, and the stent was removed. At follow-up, his symptoms resolved and LFTs normalized.
Discussion: CMV duodenitis can cause ulceration, bleeding, perforation, pseudotumor, strictures, fistulas, malabsorption, and cholestatic liver injury. Our patient with CVID and cirrhosis developed obstructive symptoms and cholestatic LFT elevation due to CMV duodenitis mimicking malignancy. CMV pseudotumors are inflammatory, mass-like lesions with granulation tissue and viral inclusions. He had high-grade duodenal narrowing with bile duct compression. Diagnosis was challenging due to nonspecific imaging and endoscopic findings. Omental caking and persistent stricture raised concern for malignancy, but repeat biopsies confirmed CMV. Negative CMV PCR highlighted the importance of tissue biopsy and immunohistochemistry. He required serial dilations and LAMS placements. While most CMV duodenitis cases respond to antivirals alone, this rare duodenal pseudotumor is the first reported to be successfully treated with combined antiviral and advanced endoscopic therapy, avoiding surgery and achieving full clinical resolution.
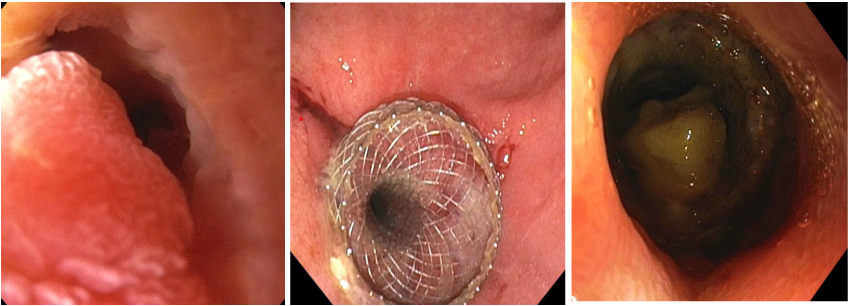
Figure: Figure 1: Severe duodenal narrowing with mass-like obstruction
Figure 2: 15 x 15 mm LAMS placed at the site of mass related stricture.
Figure 3: Follow-up EGD showing stent removal and improvement in stricture.
Disclosures:
Pratiksha Moliya indicated no relevant financial relationships.
Natapat Chaisidhivej indicated no relevant financial relationships.
Pauline Yasmeh indicated no relevant financial relationships.
Faruq Pradhan: Ipsen Biopharmaceuticals – Advisory Committee/Board Member. Madrigal Pharmaceuticals – Advisory Committee/Board Member.
Ishfaq Bhat indicated no relevant financial relationships.
Pratiksha Moliya, MD, Natapat Chaisidhivej, MD, Pauline Yasmeh, MD, Faruq Pradhan, MBBCh, Ishfaq Bhat, MD. P4112 - CMV Duodenitis Mimicking Malignancy: First Reported Case of Obstructive Pseudotumor in CVID Treated Endoscopically, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Nebraska Medical Center, Omaha, NE
Introduction: CMV GI infection is common in immunocompromised patients, but isolated CMV pseudotumors are rare, with < 25 cases reported. Most involve the colon (~40%), stomach (~20%), and other GI sites, duodenal involvement is extremely rare (< 1%). This is the first reported case of CMV duodenitis pseudotumor in a CVID patient.
Case Description/
Methods: A 66-year-old male with CVID and cirrhosis underwent screening EGD, revealing a fungating duodenal mass due to CMV duodenitis, treated with ganciclovir. A month later, he presented with vomiting, dysphagia, weight loss & elevated LFTs (AST 65, ALT 74, ALP 552, TBili 1.1). CT showed a CBD filling defect and duodenal mass with omental caking (biopsy negative for malignancy). LFTs worsened (AST 326, ALT 217, ALP 1487, TBili 26). MRCP deferred due to claustrophobia. Liver biopsy revealed interface hepatitis, likely viral or DILI. Tumor markers, hepatitis panel, and AMA were negative, CMV viremia also ruled out. EGD showed duodenal ulceration with high-grade narrowing. Balloon dilation to 13.5 mm disrupted the stricture, but the scope could not pass. Biopsies confirmed CMV duodenitis. He received ganciclovir/valganciclovir for 4 weeks, with mild improvement in symptoms and LFTs. A month later, EGD showed persistent stricture, LAMS was placed. At follow-up, mild narrowing remained, prompting a second LAMS. Three months later, EGD showed stricture improvement, and the stent was removed. At follow-up, his symptoms resolved and LFTs normalized.
Discussion: CMV duodenitis can cause ulceration, bleeding, perforation, pseudotumor, strictures, fistulas, malabsorption, and cholestatic liver injury. Our patient with CVID and cirrhosis developed obstructive symptoms and cholestatic LFT elevation due to CMV duodenitis mimicking malignancy. CMV pseudotumors are inflammatory, mass-like lesions with granulation tissue and viral inclusions. He had high-grade duodenal narrowing with bile duct compression. Diagnosis was challenging due to nonspecific imaging and endoscopic findings. Omental caking and persistent stricture raised concern for malignancy, but repeat biopsies confirmed CMV. Negative CMV PCR highlighted the importance of tissue biopsy and immunohistochemistry. He required serial dilations and LAMS placements. While most CMV duodenitis cases respond to antivirals alone, this rare duodenal pseudotumor is the first reported to be successfully treated with combined antiviral and advanced endoscopic therapy, avoiding surgery and achieving full clinical resolution.
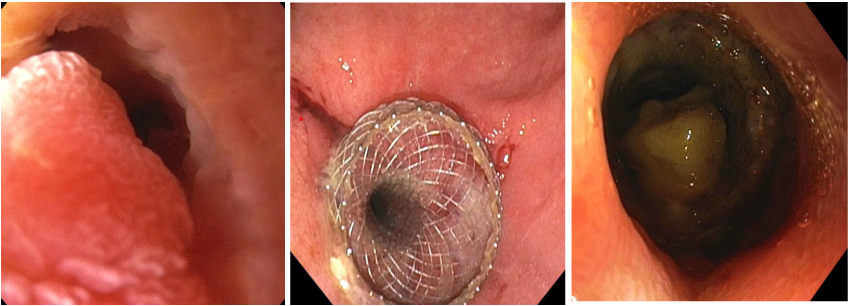
Figure: Figure 1: Severe duodenal narrowing with mass-like obstruction
Figure 2: 15 x 15 mm LAMS placed at the site of mass related stricture.
Figure 3: Follow-up EGD showing stent removal and improvement in stricture.
Disclosures:
Pratiksha Moliya indicated no relevant financial relationships.
Natapat Chaisidhivej indicated no relevant financial relationships.
Pauline Yasmeh indicated no relevant financial relationships.
Faruq Pradhan: Ipsen Biopharmaceuticals – Advisory Committee/Board Member. Madrigal Pharmaceuticals – Advisory Committee/Board Member.
Ishfaq Bhat indicated no relevant financial relationships.
Pratiksha Moliya, MD, Natapat Chaisidhivej, MD, Pauline Yasmeh, MD, Faruq Pradhan, MBBCh, Ishfaq Bhat, MD. P4112 - CMV Duodenitis Mimicking Malignancy: First Reported Case of Obstructive Pseudotumor in CVID Treated Endoscopically, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
