Monday Poster Session
Category: Small Intestine
P4081 - Melena and Iron Deficiency Anemia in a Patient With Blue Rubber Bleb Nevus Syndrome: A Rare Cause of Chronic Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Huai-En Rachel Chang, MD, MPH, MBA (she/her/hers)
East Carolina University Medical Center
Greenville, NC
Presenting Author(s)
Huai-En Chang, MD, MPH, MBA, Zarak Khan, MD, Rahul Pamarthy, MD, Swethaa Manickam, MD, Hassam Ali, MD, Marykate Kratzer, MD, Danielle Hoo-Fatt, MD
East Carolina University Medical Center, Greenville, NC
Introduction: Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare congenital vascular malformation disorder with an incidence of 1:14,000 and approximately 350 cases reported worldwide (Xia H et al., 2021). It features multifocal venous malformations of the skin and gastrointestinal tract, leading to chronic blood loss and iron deficiency anemia. Gastrointestinal involvement occurs in up to 75% of patients, but diagnosis is often delayed due to nonspecific symptoms and frequently absent cutaneous findings.
Case Description/
Methods: A 58-year-old female with coronary artery disease, atrial fibrillation status post Watchman procedure on clopidogrel, and multiple prior abdominal surgeries presented with 3 years of intermittent melena and fatigue. Laboratory studies revealed hemoglobin 5.7 g/dL, requiring blood transfusion. EGD and colonoscopy were unrevealing for a source of bleeding. Video capsule endoscopy identified multiple bluish nodular lesions occupying the proximal 40% of the small intestine, consistent with BRBNS, without active bleeding. No cutaneous lesions were noted. Surgical resection was deemed high risk given her comorbidities; conservative management with oral iron supplementation and hematologic monitoring was recommended.
Discussion: This case highlights BRBNS as a cause of obscure GI bleeding and iron deficiency anemia, especially when skin findings are absent. Capsule endoscopy is the most sensitive modality for small‐bowel vascular malformations. Double‐balloon enteroscopy may allow targeted therapy for accessible lesions. Endoscopic options include argon plasma coagulation, snare polypectomy, and sclerotherapy for focal bleeding. Sirolimus has demonstrated efficacy in refractory cases by reducing transfusion requirements and stabilizing hemoglobin. Surgical resection is reserved for localized disease in low‐risk patients but may be contraindicated in those with extensive prior surgeries or diffuse lesions.
BRBNS should be included in the differential for unexplained iron deficiency anemia and melena when standard endoscopies are negative. Early diagnosis via capsule endoscopy and a multidisciplinary approach—combining endoscopic therapy, pharmacotherapy (e.g., sirolimus), and supportive iron supplementation—are key to reducing morbidity and transfusion dependence.
Disclosure: I personally provided care for the patient described in this case and wrote the substantial content and information presented in this work. I used ChatGPT solely for proofreading and spellchecking purposes.
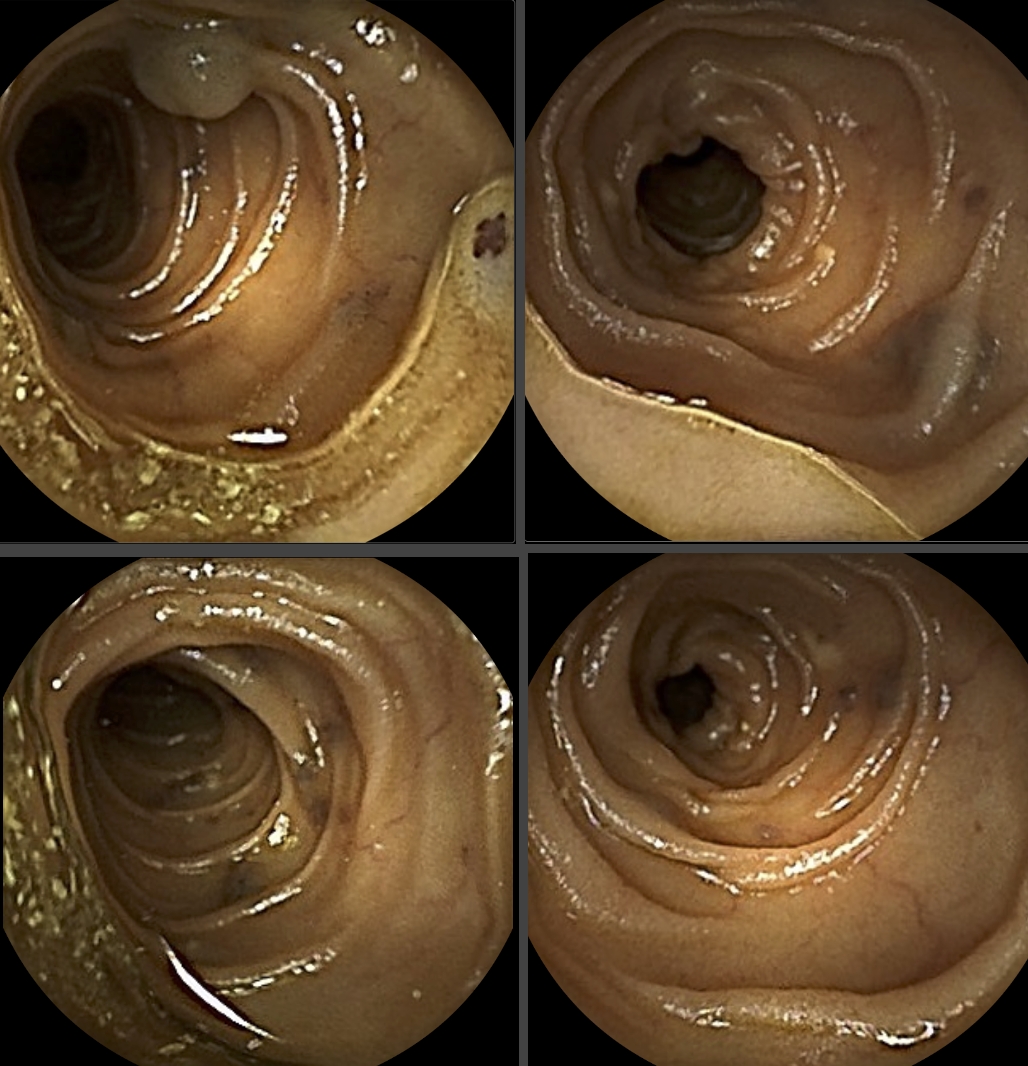
Figure: Figure 1. Capsule endoscopy revealing multiple bluish, submucosal vascular lesions as venous malformations throughout the small intestine, characteristic of Blue Rubber Bleb Nevus Syndrome.
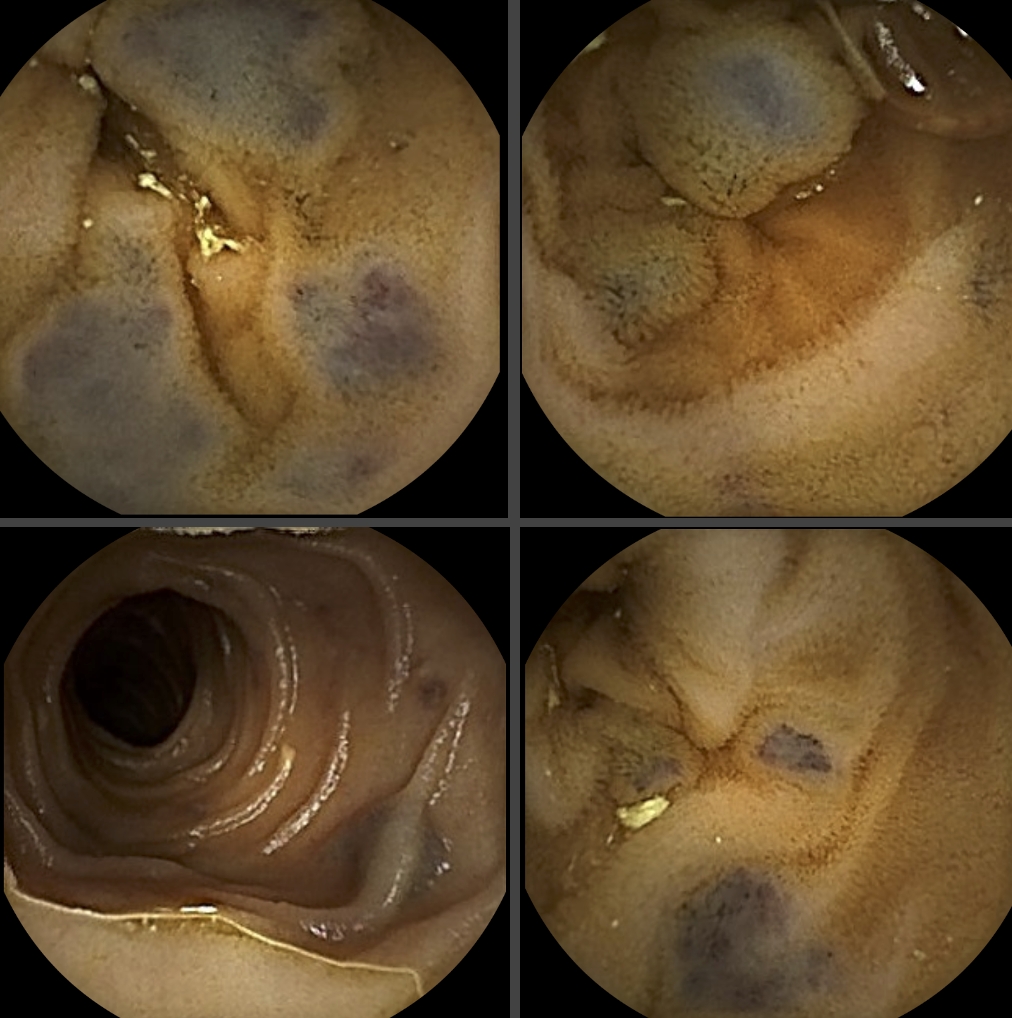
Figure: Figure 2. Capsule endoscopy demonstrating relatively normal small bowel mucosa with preserved villous pattern without active bleeding and the intermittent distribution of venous malformations.
Disclosures:
Huai-En Chang indicated no relevant financial relationships.
Zarak Khan indicated no relevant financial relationships.
Rahul Pamarthy indicated no relevant financial relationships.
Swethaa Manickam indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Marykate Kratzer indicated no relevant financial relationships.
Danielle Hoo-Fatt indicated no relevant financial relationships.
Huai-En Chang, MD, MPH, MBA, Zarak Khan, MD, Rahul Pamarthy, MD, Swethaa Manickam, MD, Hassam Ali, MD, Marykate Kratzer, MD, Danielle Hoo-Fatt, MD. P4081 - Melena and Iron Deficiency Anemia in a Patient With Blue Rubber Bleb Nevus Syndrome: A Rare Cause of Chronic Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
East Carolina University Medical Center, Greenville, NC
Introduction: Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare congenital vascular malformation disorder with an incidence of 1:14,000 and approximately 350 cases reported worldwide (Xia H et al., 2021). It features multifocal venous malformations of the skin and gastrointestinal tract, leading to chronic blood loss and iron deficiency anemia. Gastrointestinal involvement occurs in up to 75% of patients, but diagnosis is often delayed due to nonspecific symptoms and frequently absent cutaneous findings.
Case Description/
Methods: A 58-year-old female with coronary artery disease, atrial fibrillation status post Watchman procedure on clopidogrel, and multiple prior abdominal surgeries presented with 3 years of intermittent melena and fatigue. Laboratory studies revealed hemoglobin 5.7 g/dL, requiring blood transfusion. EGD and colonoscopy were unrevealing for a source of bleeding. Video capsule endoscopy identified multiple bluish nodular lesions occupying the proximal 40% of the small intestine, consistent with BRBNS, without active bleeding. No cutaneous lesions were noted. Surgical resection was deemed high risk given her comorbidities; conservative management with oral iron supplementation and hematologic monitoring was recommended.
Discussion: This case highlights BRBNS as a cause of obscure GI bleeding and iron deficiency anemia, especially when skin findings are absent. Capsule endoscopy is the most sensitive modality for small‐bowel vascular malformations. Double‐balloon enteroscopy may allow targeted therapy for accessible lesions. Endoscopic options include argon plasma coagulation, snare polypectomy, and sclerotherapy for focal bleeding. Sirolimus has demonstrated efficacy in refractory cases by reducing transfusion requirements and stabilizing hemoglobin. Surgical resection is reserved for localized disease in low‐risk patients but may be contraindicated in those with extensive prior surgeries or diffuse lesions.
BRBNS should be included in the differential for unexplained iron deficiency anemia and melena when standard endoscopies are negative. Early diagnosis via capsule endoscopy and a multidisciplinary approach—combining endoscopic therapy, pharmacotherapy (e.g., sirolimus), and supportive iron supplementation—are key to reducing morbidity and transfusion dependence.
Disclosure: I personally provided care for the patient described in this case and wrote the substantial content and information presented in this work. I used ChatGPT solely for proofreading and spellchecking purposes.
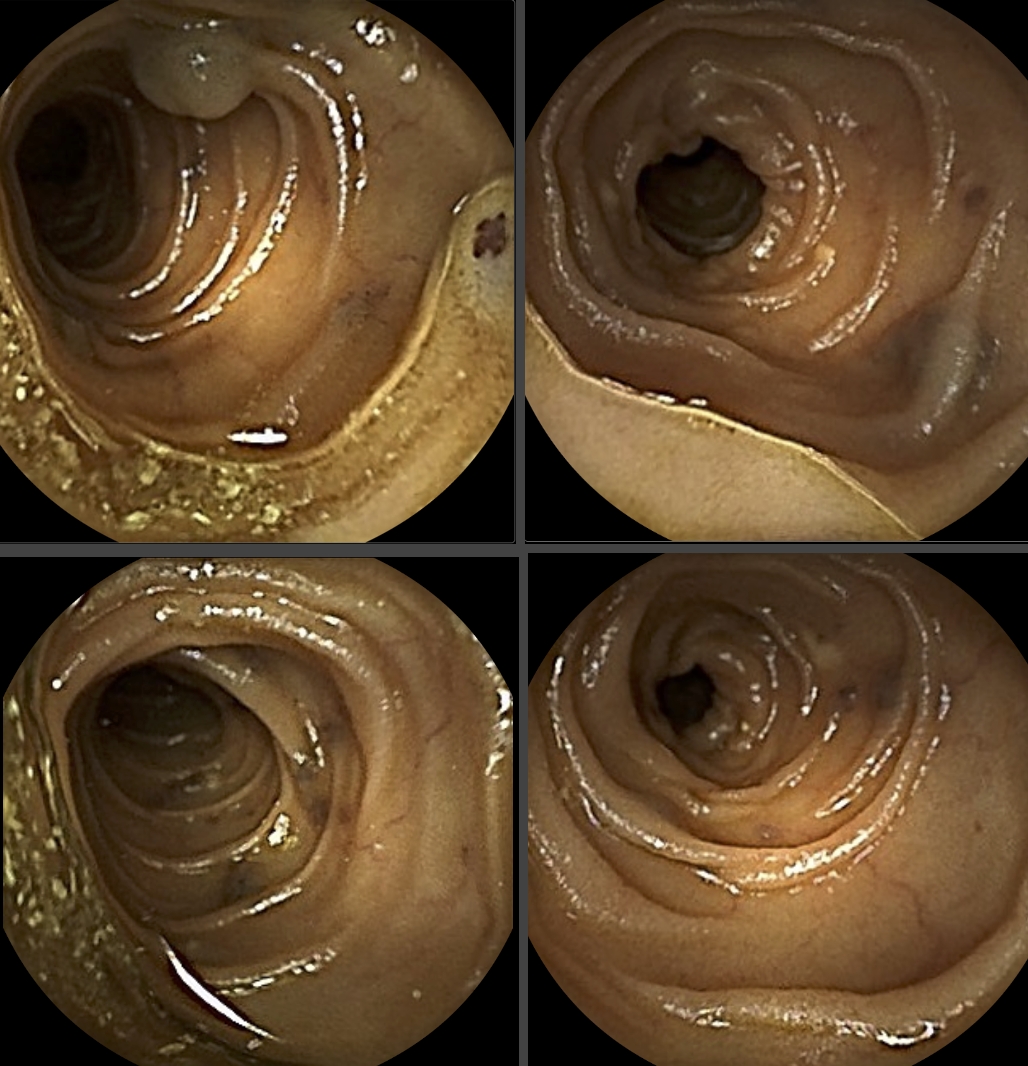
Figure: Figure 1. Capsule endoscopy revealing multiple bluish, submucosal vascular lesions as venous malformations throughout the small intestine, characteristic of Blue Rubber Bleb Nevus Syndrome.
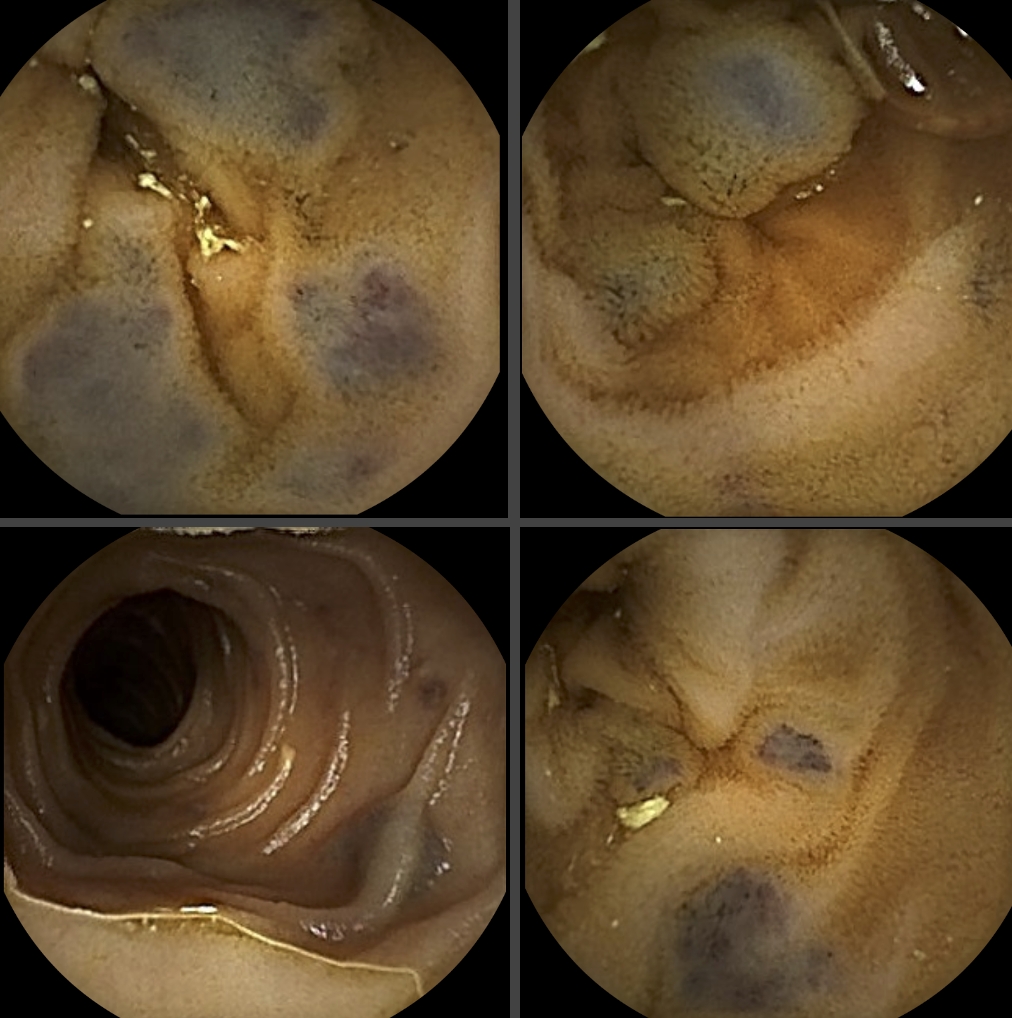
Figure: Figure 2. Capsule endoscopy demonstrating relatively normal small bowel mucosa with preserved villous pattern without active bleeding and the intermittent distribution of venous malformations.
Disclosures:
Huai-En Chang indicated no relevant financial relationships.
Zarak Khan indicated no relevant financial relationships.
Rahul Pamarthy indicated no relevant financial relationships.
Swethaa Manickam indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Marykate Kratzer indicated no relevant financial relationships.
Danielle Hoo-Fatt indicated no relevant financial relationships.
Huai-En Chang, MD, MPH, MBA, Zarak Khan, MD, Rahul Pamarthy, MD, Swethaa Manickam, MD, Hassam Ali, MD, Marykate Kratzer, MD, Danielle Hoo-Fatt, MD. P4081 - Melena and Iron Deficiency Anemia in a Patient With Blue Rubber Bleb Nevus Syndrome: A Rare Cause of Chronic Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
