Monday Poster Session
Category: Small Intestine
P4061 - Temporal Trends in Vascular Catastrophe: Acute Mesenteric Ischemia and Atrial Fibrillation in Older Americans (1999-2023)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aisha Rehman Siddiqui, MD (she/her/hers)
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Aisha Siddiqui, MD1, Rizwana Noor, 2, Sadaf Iftikhar, MBBS3, Muhammad Abdullah, MBBS4, Noor-us-Sahar Siddiqui, MBBS5, Farina Siddiqui, MBBS5
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Khyber Medical College, Peshawar, North-West Frontier, Pakistan; 3Akhtar Saeed Medical and dental college, Lahore, Punjab, Pakistan; 4Shalamar Institute of Health Sciences, Lahore, Punjab, Pakistan; 5Liaquat University of Medical and Health Science, Hyderabad, Sindh, Pakistan
Introduction: Acute Mesenteric Ischemia (AMI) is a life-threatening
abdominal vascular emergency frequently associated with cardiovascular conditions such as atrial fibrillation (AF). Sharing several common risk factors, AMI and AF may mutually worsen clinical outcomes when coexisting. This study analyzes nationwide mortality trends and patterns over the past two decades to explore the relationship between these conditions among older adults in the United States.
Methods: We analyzed CDC WONDER data to calculate age-adjusted and crude mortality rates per 100,000 for adults aged ≥65 who died from acute mesenteric ischemia (K55.0) and atrial fibrillation (I48). Trends were evaluated using Joinpoint regression to estimate APC and AAPC with 95% confidence intervals
Results: According to our study, from 1999 to 2023, 8,849 AMI deaths occurred in AF patients. Age-adjusted mortality declined from 1.61 to 0.68 per 100,000 (AAPC −3.39%), with a nonsignificant rise after 2020 (APC +6.61%). Female mortality was higher but declined more rapidly. Non-Hispanic Black mortality rose (AAPC +12.32%), while non-Hispanic White mortality declined. The South and Northeast saw the largest drops. Rural rates stayed higher despite sharper urban declines. Adults aged 75–84 bore the highest burden; 8034 (91%) of deaths occurred in medical facilities.
Discussion: These findings demonstrate a sustained decline in AMI mortality among AF patients, likely reflecting advances in evidence-based treatments and risk-factor control. The modest post-2020 rebound aligns with pandemic-related healthcare disruptions. Despite overall declines, female patients had a higher initial mortality but greater declines, suggesting narrowing sex gaps, possibly due to increased awareness and targeted interventions for women. Rising mortality among non-Hispanic Blacks, in contrast to declines in Whites, highlights persistent racial inequities in care and outcomes. Geographically, the largest improvements were in the South and Northeast, whereas persistently higher rates in rural areas (despite larger urban declines) underscore access gaps. Adults aged 75–84 bore the highest burden, and >90% of deaths occurred in medical facilities, emphasizing the need for age-focused strategies and robust hospital care pathways. Ongoing surveillance and targeted interventions are warranted to address remaining inequities.
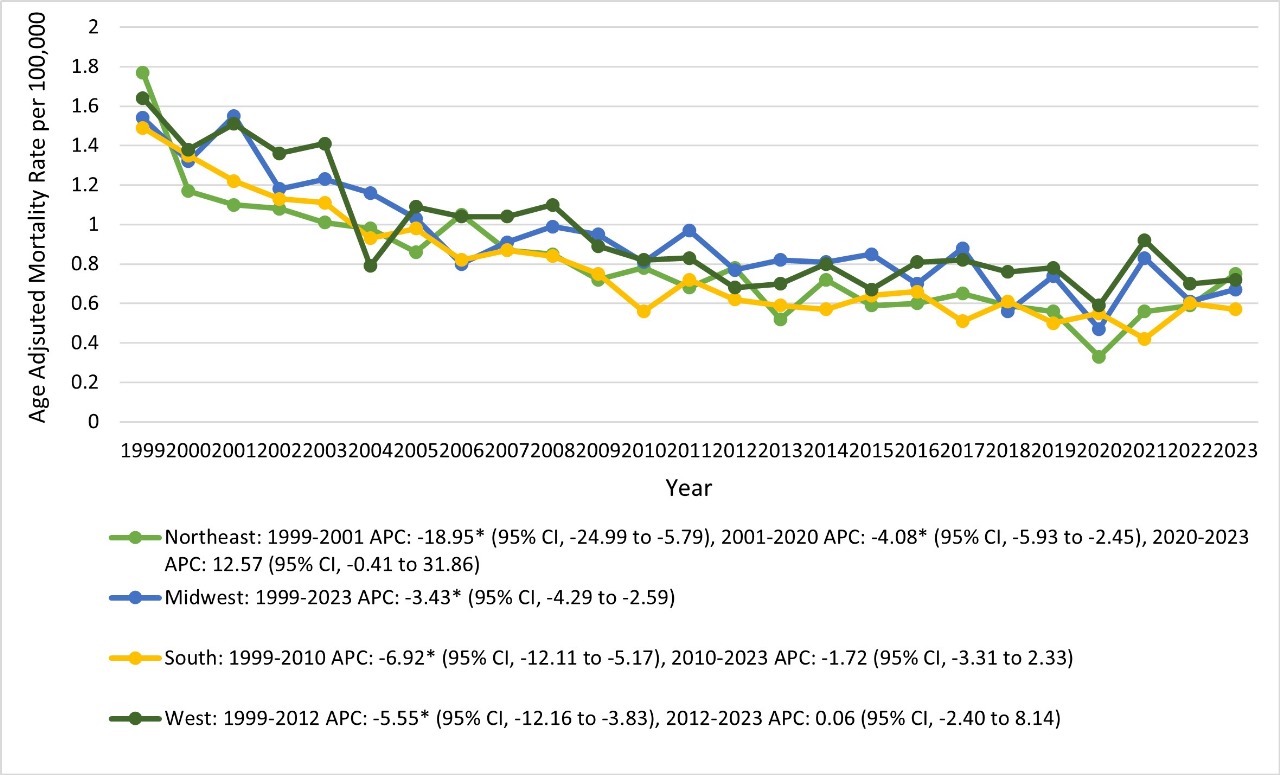
Figure: Trends in acute mesenteric ischemia and mortality related to atrial fibrillation stratified by census regions in the United States from 1999 to 2023.
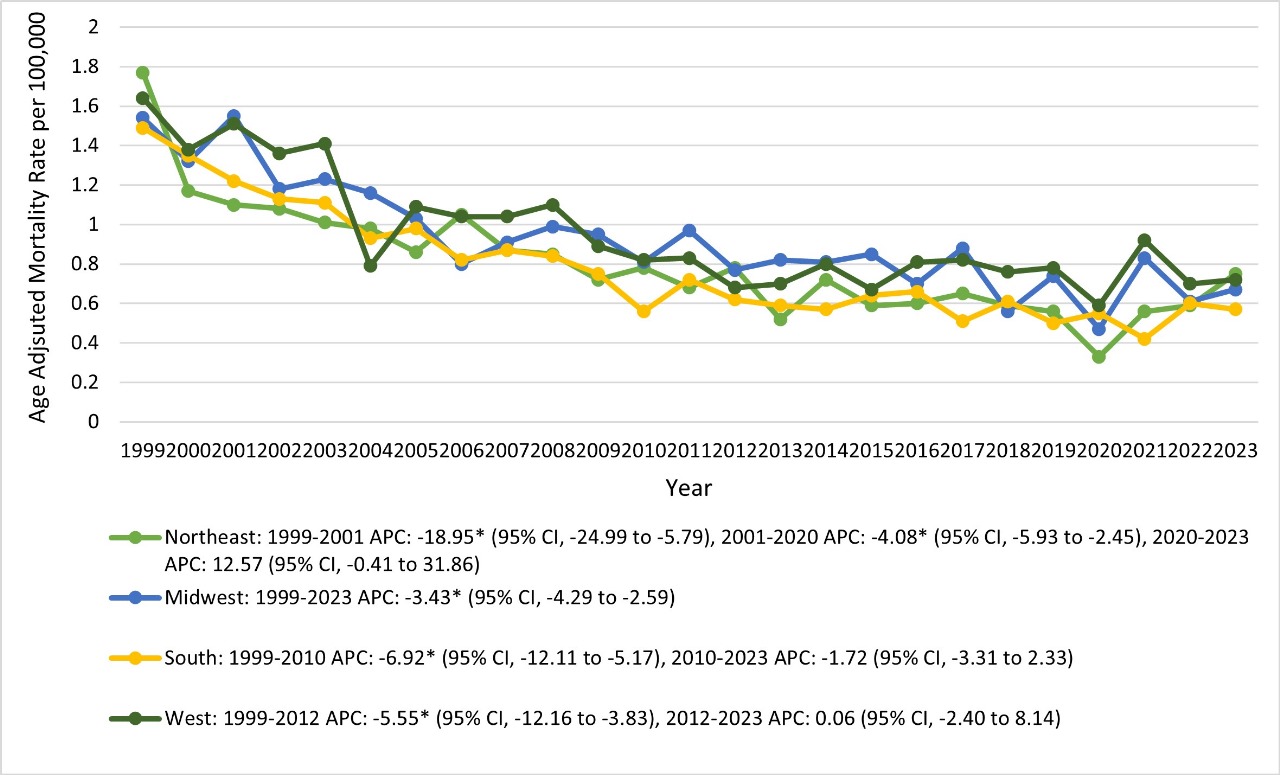
Figure: Trends in acute mesenteric ischemia and atrial fibrillation-related mortality stratified by sex in the United States from 1999 to 2023.
Disclosures:
Aisha Siddiqui indicated no relevant financial relationships.
Rizwana Noor indicated no relevant financial relationships.
Sadaf Iftikhar indicated no relevant financial relationships.
Muhammad Abdullah indicated no relevant financial relationships.
Noor-us-Sahar Siddiqui indicated no relevant financial relationships.
Farina Siddiqui indicated no relevant financial relationships.
Aisha Siddiqui, MD1, Rizwana Noor, 2, Sadaf Iftikhar, MBBS3, Muhammad Abdullah, MBBS4, Noor-us-Sahar Siddiqui, MBBS5, Farina Siddiqui, MBBS5. P4061 - Temporal Trends in Vascular Catastrophe: Acute Mesenteric Ischemia and Atrial Fibrillation in Older Americans (1999-2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Khyber Medical College, Peshawar, North-West Frontier, Pakistan; 3Akhtar Saeed Medical and dental college, Lahore, Punjab, Pakistan; 4Shalamar Institute of Health Sciences, Lahore, Punjab, Pakistan; 5Liaquat University of Medical and Health Science, Hyderabad, Sindh, Pakistan
Introduction: Acute Mesenteric Ischemia (AMI) is a life-threatening
abdominal vascular emergency frequently associated with cardiovascular conditions such as atrial fibrillation (AF). Sharing several common risk factors, AMI and AF may mutually worsen clinical outcomes when coexisting. This study analyzes nationwide mortality trends and patterns over the past two decades to explore the relationship between these conditions among older adults in the United States.
Methods: We analyzed CDC WONDER data to calculate age-adjusted and crude mortality rates per 100,000 for adults aged ≥65 who died from acute mesenteric ischemia (K55.0) and atrial fibrillation (I48). Trends were evaluated using Joinpoint regression to estimate APC and AAPC with 95% confidence intervals
Results: According to our study, from 1999 to 2023, 8,849 AMI deaths occurred in AF patients. Age-adjusted mortality declined from 1.61 to 0.68 per 100,000 (AAPC −3.39%), with a nonsignificant rise after 2020 (APC +6.61%). Female mortality was higher but declined more rapidly. Non-Hispanic Black mortality rose (AAPC +12.32%), while non-Hispanic White mortality declined. The South and Northeast saw the largest drops. Rural rates stayed higher despite sharper urban declines. Adults aged 75–84 bore the highest burden; 8034 (91%) of deaths occurred in medical facilities.
Discussion: These findings demonstrate a sustained decline in AMI mortality among AF patients, likely reflecting advances in evidence-based treatments and risk-factor control. The modest post-2020 rebound aligns with pandemic-related healthcare disruptions. Despite overall declines, female patients had a higher initial mortality but greater declines, suggesting narrowing sex gaps, possibly due to increased awareness and targeted interventions for women. Rising mortality among non-Hispanic Blacks, in contrast to declines in Whites, highlights persistent racial inequities in care and outcomes. Geographically, the largest improvements were in the South and Northeast, whereas persistently higher rates in rural areas (despite larger urban declines) underscore access gaps. Adults aged 75–84 bore the highest burden, and >90% of deaths occurred in medical facilities, emphasizing the need for age-focused strategies and robust hospital care pathways. Ongoing surveillance and targeted interventions are warranted to address remaining inequities.
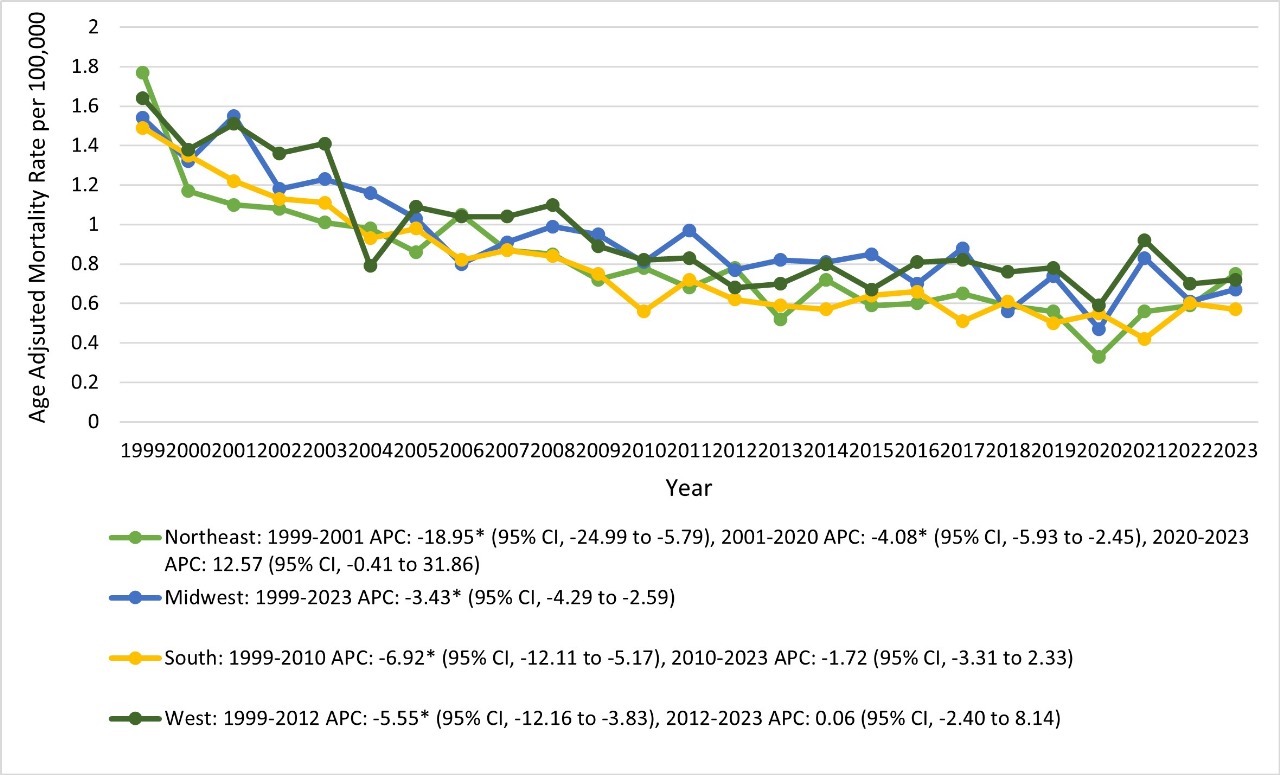
Figure: Trends in acute mesenteric ischemia and mortality related to atrial fibrillation stratified by census regions in the United States from 1999 to 2023.
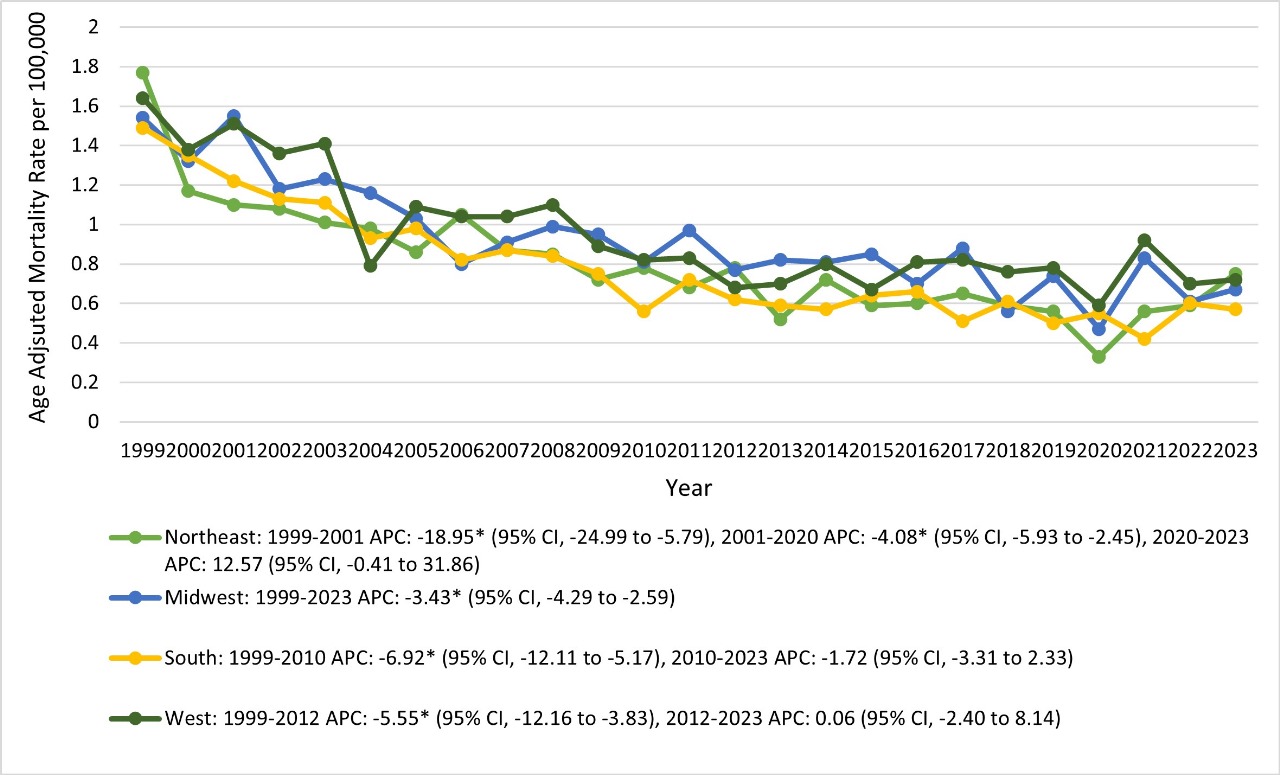
Figure: Trends in acute mesenteric ischemia and atrial fibrillation-related mortality stratified by sex in the United States from 1999 to 2023.
Disclosures:
Aisha Siddiqui indicated no relevant financial relationships.
Rizwana Noor indicated no relevant financial relationships.
Sadaf Iftikhar indicated no relevant financial relationships.
Muhammad Abdullah indicated no relevant financial relationships.
Noor-us-Sahar Siddiqui indicated no relevant financial relationships.
Farina Siddiqui indicated no relevant financial relationships.
Aisha Siddiqui, MD1, Rizwana Noor, 2, Sadaf Iftikhar, MBBS3, Muhammad Abdullah, MBBS4, Noor-us-Sahar Siddiqui, MBBS5, Farina Siddiqui, MBBS5. P4061 - Temporal Trends in Vascular Catastrophe: Acute Mesenteric Ischemia and Atrial Fibrillation in Older Americans (1999-2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
