Monday Poster Session
Category: Small Intestine
P4051 - Elevated Risk of Developing Small Intestinal Bacterial Overgrowth Following Influenza Infection: A Nationwide Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yilin Song, MD (she/her/hers)
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Thai Hau Koo, MD1, Yilin Song, MD2, Rishi Chowdhary, MD3, Xue Leong, 1, Kewin Tien Ho Siah, MD4, Tao Bai, MD5, Lei Tu, MD6, Gengqing Song, MD7
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2University of Maryland Medical Center, Baltimore, MD; 3Case Western Reserve University / MetroHealth, Cleveland, OH; 4National University of Singapore, Singapore, Singapore; 5Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Tianjin, China; 6Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China; 7Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: The prevalence of small intestinal bacterial overgrowth (SIBO) following an influenza infection remains unclear, despite sporadic reports. This study aimed to evaluate the incidence of SIBO following influenza across the United States.
Methods: This retrospective cohort study analyzed data from the TriNetX database, including adult inpatients (≥18 years) diagnosed with confirmed influenza between Jan 1, 2021, and May 1, 2024, to align with the global adoption of SIBO diagnostic coding starting in 2021 and to allow for up to 12 months of follow-up through May 1, 2025. Patients with prior SIBO or concurrent viral infections, including COVID-19, were excluded. Propensity score matching (1:1) was adjusted for demographic and SIBO risk factors. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of SIBO within 3, 6, and 12 months. Subgroup analyses were assessed by influenza type, sex, and race/ethnicity. Sensitivity analyses restricted cohorts to influenza diagnoses from January 2023 onward to address confounding by undiagnosed COVID-19.
Results: The analysis included 2,094,587 influenza patients (type A: 1,381,865; type B: 189,190) and 4,993,447 matched controls. SIBO was diagnosed in 1,433 influenza patients (356 by hydrogen breath test [BT], 1,077 by diagnostic coding) and 1,747 controls (213 by BT, 1,534 by coding). Influenza patients demonstrated significantly higher odds of developing SIBO within 3 months (OR 1.86; 95% CI 1.23-2.80; p=0.003), 6 months (OR 1.69; 95% CI 1.27-2.25; p< 0.001), and 12 months (OR 1.89; 95% CI 1.54-2.31; p< 0.001). Influenza type A showed the strongest association (12-month OR 2.01; 95% CI 1.58-2.56; p< 0.001). Subgroup analyses revealed significantly higher 12-month SIBO incidence among females (OR 2.05; 95% CI 1.62-2.60; p< 0.001) and white patients (OR 1.99; 95% CI 1.58-2.51; p< 0.001), with peak rates in patients aged≥75 years (0.048%) and females (0.028%). No significant associations were observed in influenza type B, Black/African American, or Hispanic subgroups. Sensitivity analyses confirmed similar trends across all follow-up periods.
Discussion: This nationwide study identifies significantly increased SIBO risk following influenza, especially type A, with higher risks in females and white patients. Further research into underlying mechanisms and healthcare disparities is warranted.
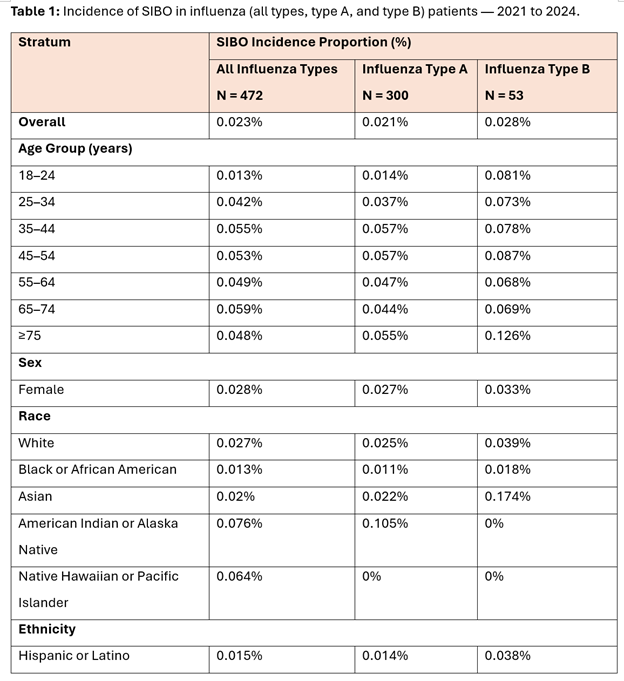
Figure: Table 1: Incidence of SIBO in influenza (all types, type A, and type B) patients — 2021 to 2024.
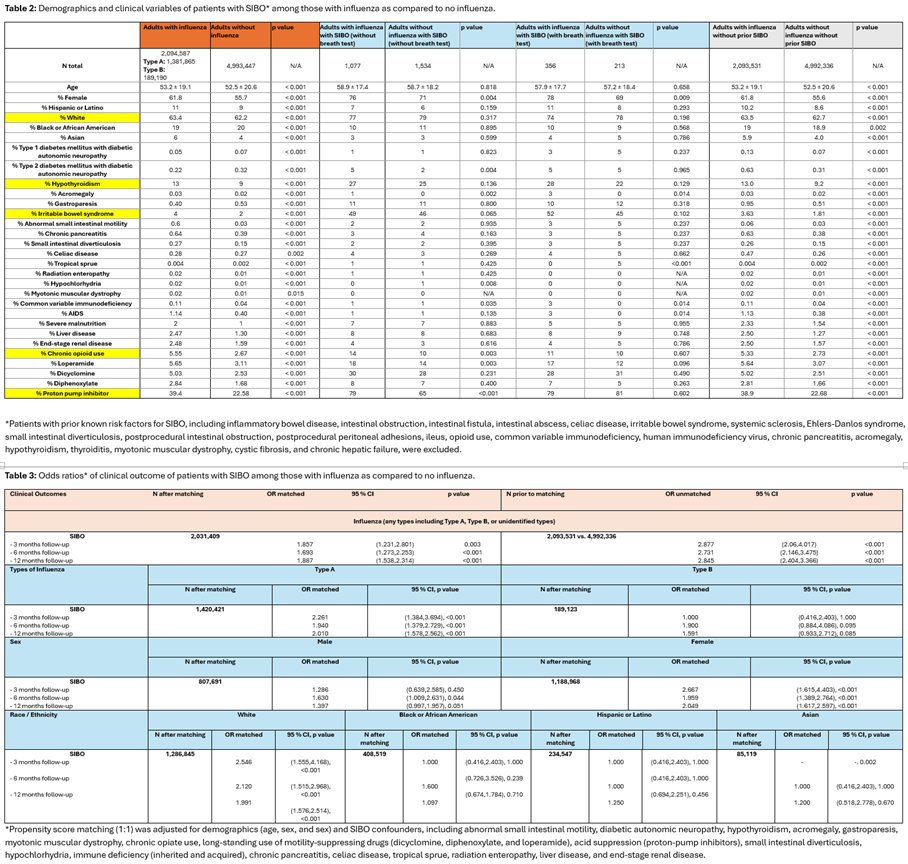
Figure: Table 2: Demographics and clinical variables of patients with SIBO* among those with influenza as compared to no influenza. Table 3: Odds ratios* of clinical outcome of patients with SIBO among those with influenza as compared to no influenza.
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Yilin Song indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Xue Leong indicated no relevant financial relationships.
Kewin Tien Ho Siah indicated no relevant financial relationships.
Tao Bai indicated no relevant financial relationships.
Lei Tu indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Thai Hau Koo, MD1, Yilin Song, MD2, Rishi Chowdhary, MD3, Xue Leong, 1, Kewin Tien Ho Siah, MD4, Tao Bai, MD5, Lei Tu, MD6, Gengqing Song, MD7. P4051 - Elevated Risk of Developing Small Intestinal Bacterial Overgrowth Following Influenza Infection: A Nationwide Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2University of Maryland Medical Center, Baltimore, MD; 3Case Western Reserve University / MetroHealth, Cleveland, OH; 4National University of Singapore, Singapore, Singapore; 5Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Tianjin, China; 6Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China; 7Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: The prevalence of small intestinal bacterial overgrowth (SIBO) following an influenza infection remains unclear, despite sporadic reports. This study aimed to evaluate the incidence of SIBO following influenza across the United States.
Methods: This retrospective cohort study analyzed data from the TriNetX database, including adult inpatients (≥18 years) diagnosed with confirmed influenza between Jan 1, 2021, and May 1, 2024, to align with the global adoption of SIBO diagnostic coding starting in 2021 and to allow for up to 12 months of follow-up through May 1, 2025. Patients with prior SIBO or concurrent viral infections, including COVID-19, were excluded. Propensity score matching (1:1) was adjusted for demographic and SIBO risk factors. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of SIBO within 3, 6, and 12 months. Subgroup analyses were assessed by influenza type, sex, and race/ethnicity. Sensitivity analyses restricted cohorts to influenza diagnoses from January 2023 onward to address confounding by undiagnosed COVID-19.
Results: The analysis included 2,094,587 influenza patients (type A: 1,381,865; type B: 189,190) and 4,993,447 matched controls. SIBO was diagnosed in 1,433 influenza patients (356 by hydrogen breath test [BT], 1,077 by diagnostic coding) and 1,747 controls (213 by BT, 1,534 by coding). Influenza patients demonstrated significantly higher odds of developing SIBO within 3 months (OR 1.86; 95% CI 1.23-2.80; p=0.003), 6 months (OR 1.69; 95% CI 1.27-2.25; p< 0.001), and 12 months (OR 1.89; 95% CI 1.54-2.31; p< 0.001). Influenza type A showed the strongest association (12-month OR 2.01; 95% CI 1.58-2.56; p< 0.001). Subgroup analyses revealed significantly higher 12-month SIBO incidence among females (OR 2.05; 95% CI 1.62-2.60; p< 0.001) and white patients (OR 1.99; 95% CI 1.58-2.51; p< 0.001), with peak rates in patients aged≥75 years (0.048%) and females (0.028%). No significant associations were observed in influenza type B, Black/African American, or Hispanic subgroups. Sensitivity analyses confirmed similar trends across all follow-up periods.
Discussion: This nationwide study identifies significantly increased SIBO risk following influenza, especially type A, with higher risks in females and white patients. Further research into underlying mechanisms and healthcare disparities is warranted.
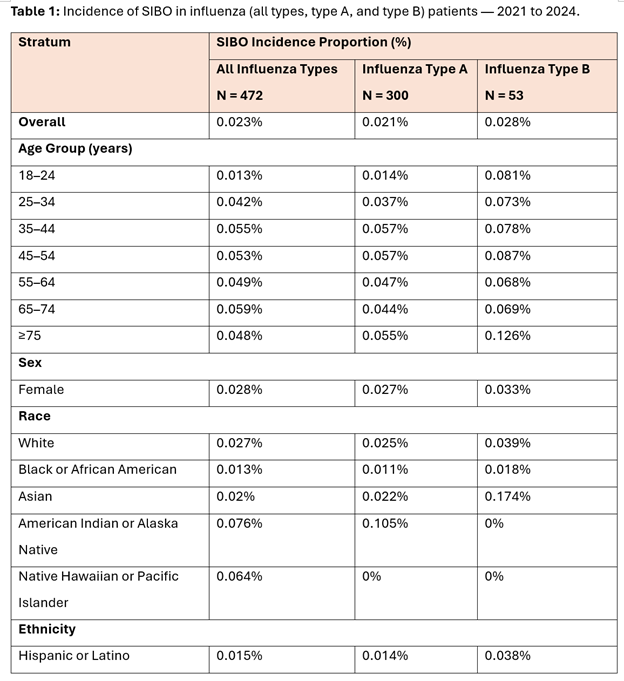
Figure: Table 1: Incidence of SIBO in influenza (all types, type A, and type B) patients — 2021 to 2024.
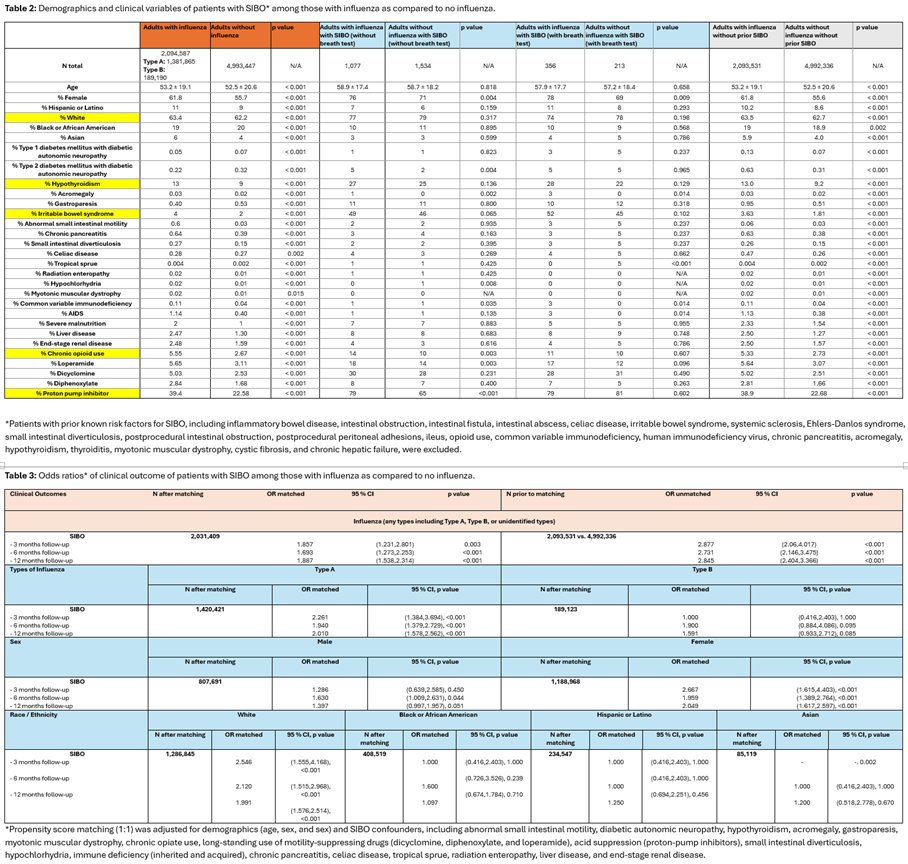
Figure: Table 2: Demographics and clinical variables of patients with SIBO* among those with influenza as compared to no influenza. Table 3: Odds ratios* of clinical outcome of patients with SIBO among those with influenza as compared to no influenza.
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Yilin Song indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Xue Leong indicated no relevant financial relationships.
Kewin Tien Ho Siah indicated no relevant financial relationships.
Tao Bai indicated no relevant financial relationships.
Lei Tu indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Thai Hau Koo, MD1, Yilin Song, MD2, Rishi Chowdhary, MD3, Xue Leong, 1, Kewin Tien Ho Siah, MD4, Tao Bai, MD5, Lei Tu, MD6, Gengqing Song, MD7. P4051 - Elevated Risk of Developing Small Intestinal Bacterial Overgrowth Following Influenza Infection: A Nationwide Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
