Monday Poster Session
Category: Small Intestine
P4049 - Clinico-Histologic Correlation of Small Bowel Ulcers: Differentiating NSAIDs, Crohn’s, CMUSE and CNSU
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rangesh Modi, MBBS, MD
University of Chicago Medical Center
Chicago, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Rangesh Modi, MBBS, MD1, Namrata Setia, MD1, John Hart, MD1, Edwin McDonald, MD1, Carol Semrad, MD, FACG1, Dejan Micic, MD2
1University of Chicago Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL
Introduction: Small bowel (SB) ulcers and strictures can stem from many underlying pathologies. Crohn’s disease (CD), NSAID injury, and the emerging genetic disorders of prostaglandin production (cryptogenic multifocal ulcerous stenosing enteritis [CMUSE]) or reuptake (chronic nonspecific ulcers of the small intestine [CNSU]) have significant overlapping clinical and endoscopic features. Device-assisted enteroscopy (DAE) has allowed direct visualization and tissue sampling of ulcers deep in the small bowel. We aim to assess the correlation frequency between the clinical and histologic diagnoses of CD, NSAID, and CMUSE/CNSU SB ulcers.
Methods: A retrospective cohort study at The University of Chicago (04/2004–04/2024) included adults with jejunal or ileal SB ulcers/strictures identified during DAE and recorded in ProVation (Minneapolis, MN). Patients with clinical diagnoses of CD, NSAID injury, or CMUSE/CNSU based on history, labs, imaging, and endoscopy were included. Exclusions applied to those with duodenal, terminal ileal, anastomotic ulcers, ulcers from other etiologies, or missing data (n=38). Two gastroenterologists (DM, CS) and RM assigned diagnoses; a blinded expert pathologist (JH) performed a histologic review. Cohen’s kappa (κ) assessed agreement between clinical and histologic diagnoses.
Results: Among 102 patients with SB ulcers/strictures, 41 met the inclusion criteria (Table 1). Based on clinical consensus, 26 (63.5%) had NSAID injury, 12 (29.5%) had CD, and 3 (7%) were CMUSE/CNSU. Of 26 patients with a clinical diagnosis of NSAID injury, blinded histology review reported 23/26 (88%) as NSAID injury (Table 2). Of 12 patients with a clinical diagnosis of CD, blinded histology review reported 5/12 (41%) as CD. Of 3 patients with a clinical diagnosis of CMUSE/CNSU, blinded histology review reported 2/3 (67%) as NSAID or CMUSE/CNSU and 1/3 (33%) as NSAID enteropathy. The correlation between a clinical diagnosis and histology was 28/41 (68%), corresponding to a k of 0.45, indicating moderate agreement. Of the 13 discordant cases, 6 (46%) remained uncertain after longitudinal follow-up for a median of 7 years. Of 7 discordant CD cases, 4 (57%) required multiple biologics and surgical resections, with 2/4 (50%) developing short bowel syndrome needing parenteral nutrition (PN).
Discussion: Differentiating the underlying cause of SB ulcers/strictures is challenging due to overlapping clinical and histologic features with only moderate agreement necessitating additional diagnostic tools.
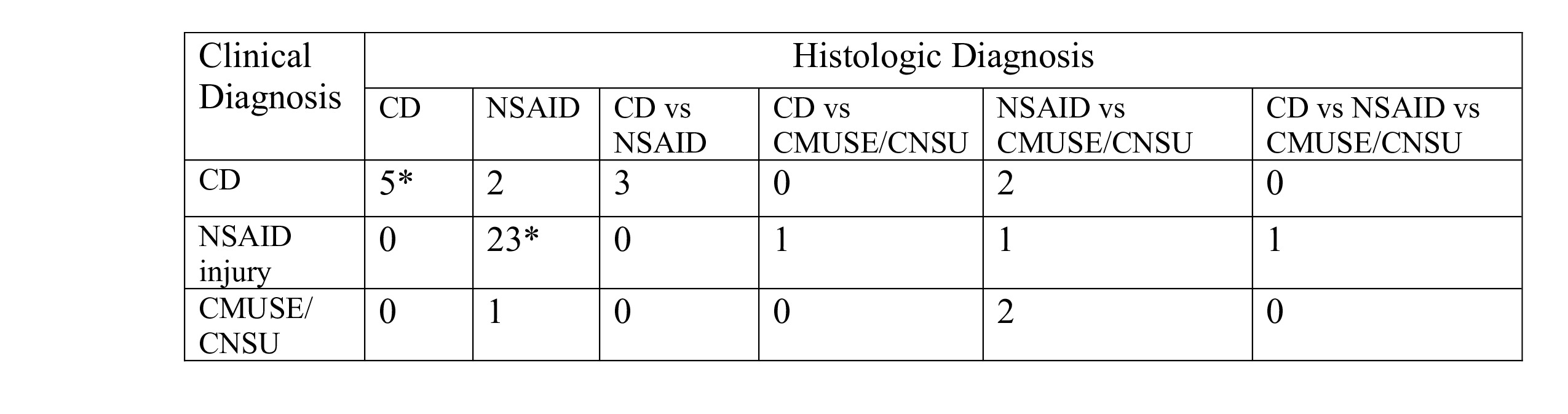
Figure: Table 1: Patient characteristics
Mo: Months; AA: African American
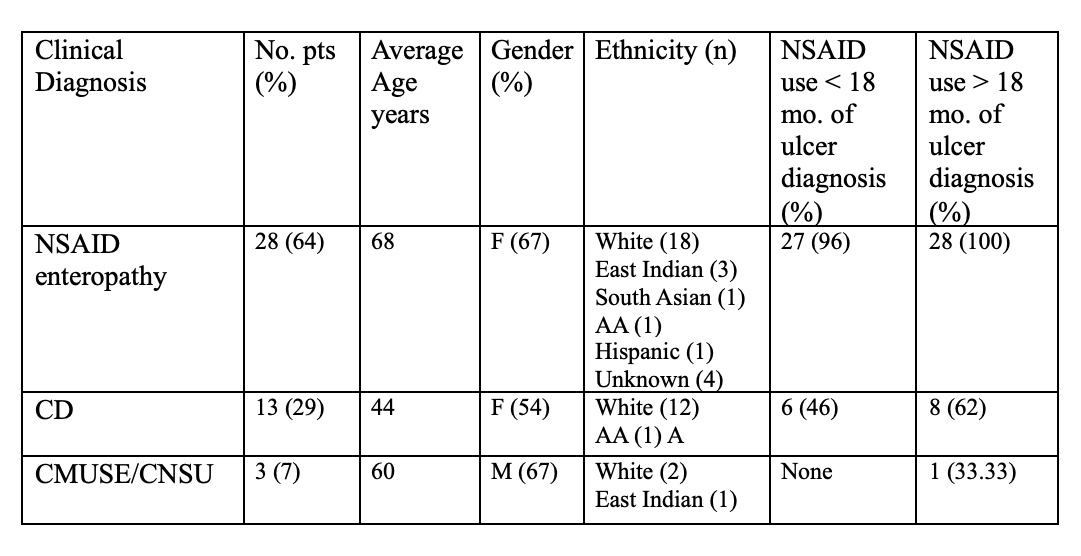
Figure: Table 2: Clinical and histologic correlation for small bowel ulcer diagnosis
* concordant cases
Disclosures:
Rangesh Modi indicated no relevant financial relationships.
Namrata Setia indicated no relevant financial relationships.
John Hart indicated no relevant financial relationships.
Edwin McDonald indicated no relevant financial relationships.
Carol Semrad indicated no relevant financial relationships.
Dejan Micic: Ironwood Pharmaceuticals – Advisor or Review Panel Member. Protara Therapeutics – Advisor or Review Panel Member. Takeda Pharmaceuticals – Advisor or Review Panel Member, Speakers Bureau.
Rangesh Modi, MBBS, MD1, Namrata Setia, MD1, John Hart, MD1, Edwin McDonald, MD1, Carol Semrad, MD, FACG1, Dejan Micic, MD2. P4049 - Clinico-Histologic Correlation of Small Bowel Ulcers: Differentiating NSAIDs, Crohn’s, CMUSE and CNSU, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rangesh Modi, MBBS, MD1, Namrata Setia, MD1, John Hart, MD1, Edwin McDonald, MD1, Carol Semrad, MD, FACG1, Dejan Micic, MD2
1University of Chicago Medical Center, Chicago, IL; 2Loyola University Medical Center, Maywood, IL
Introduction: Small bowel (SB) ulcers and strictures can stem from many underlying pathologies. Crohn’s disease (CD), NSAID injury, and the emerging genetic disorders of prostaglandin production (cryptogenic multifocal ulcerous stenosing enteritis [CMUSE]) or reuptake (chronic nonspecific ulcers of the small intestine [CNSU]) have significant overlapping clinical and endoscopic features. Device-assisted enteroscopy (DAE) has allowed direct visualization and tissue sampling of ulcers deep in the small bowel. We aim to assess the correlation frequency between the clinical and histologic diagnoses of CD, NSAID, and CMUSE/CNSU SB ulcers.
Methods: A retrospective cohort study at The University of Chicago (04/2004–04/2024) included adults with jejunal or ileal SB ulcers/strictures identified during DAE and recorded in ProVation (Minneapolis, MN). Patients with clinical diagnoses of CD, NSAID injury, or CMUSE/CNSU based on history, labs, imaging, and endoscopy were included. Exclusions applied to those with duodenal, terminal ileal, anastomotic ulcers, ulcers from other etiologies, or missing data (n=38). Two gastroenterologists (DM, CS) and RM assigned diagnoses; a blinded expert pathologist (JH) performed a histologic review. Cohen’s kappa (κ) assessed agreement between clinical and histologic diagnoses.
Results: Among 102 patients with SB ulcers/strictures, 41 met the inclusion criteria (Table 1). Based on clinical consensus, 26 (63.5%) had NSAID injury, 12 (29.5%) had CD, and 3 (7%) were CMUSE/CNSU. Of 26 patients with a clinical diagnosis of NSAID injury, blinded histology review reported 23/26 (88%) as NSAID injury (Table 2). Of 12 patients with a clinical diagnosis of CD, blinded histology review reported 5/12 (41%) as CD. Of 3 patients with a clinical diagnosis of CMUSE/CNSU, blinded histology review reported 2/3 (67%) as NSAID or CMUSE/CNSU and 1/3 (33%) as NSAID enteropathy. The correlation between a clinical diagnosis and histology was 28/41 (68%), corresponding to a k of 0.45, indicating moderate agreement. Of the 13 discordant cases, 6 (46%) remained uncertain after longitudinal follow-up for a median of 7 years. Of 7 discordant CD cases, 4 (57%) required multiple biologics and surgical resections, with 2/4 (50%) developing short bowel syndrome needing parenteral nutrition (PN).
Discussion: Differentiating the underlying cause of SB ulcers/strictures is challenging due to overlapping clinical and histologic features with only moderate agreement necessitating additional diagnostic tools.
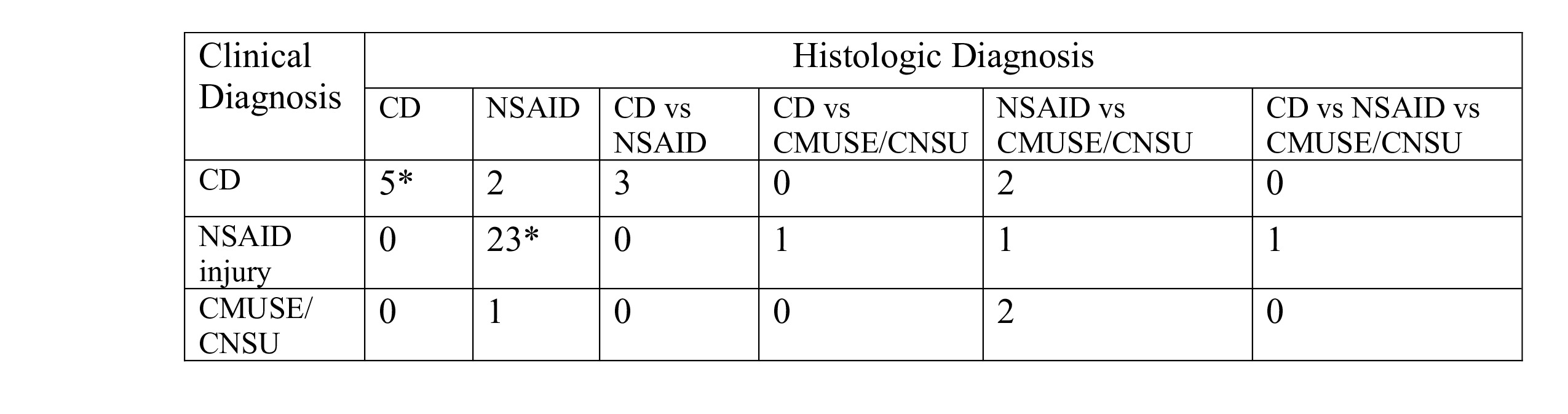
Figure: Table 1: Patient characteristics
Mo: Months; AA: African American
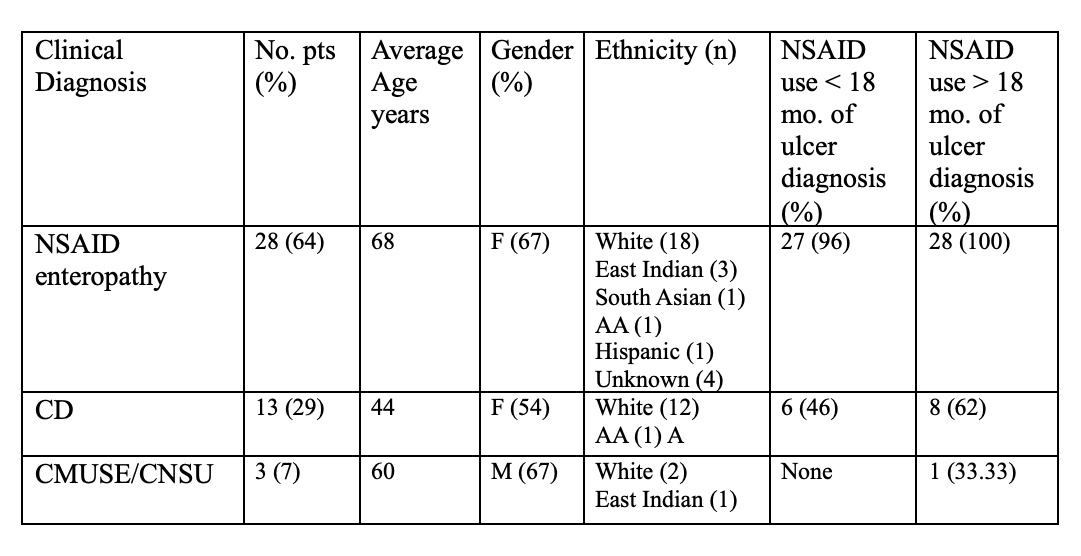
Figure: Table 2: Clinical and histologic correlation for small bowel ulcer diagnosis
* concordant cases
Disclosures:
Rangesh Modi indicated no relevant financial relationships.
Namrata Setia indicated no relevant financial relationships.
John Hart indicated no relevant financial relationships.
Edwin McDonald indicated no relevant financial relationships.
Carol Semrad indicated no relevant financial relationships.
Dejan Micic: Ironwood Pharmaceuticals – Advisor or Review Panel Member. Protara Therapeutics – Advisor or Review Panel Member. Takeda Pharmaceuticals – Advisor or Review Panel Member, Speakers Bureau.
Rangesh Modi, MBBS, MD1, Namrata Setia, MD1, John Hart, MD1, Edwin McDonald, MD1, Carol Semrad, MD, FACG1, Dejan Micic, MD2. P4049 - Clinico-Histologic Correlation of Small Bowel Ulcers: Differentiating NSAIDs, Crohn’s, CMUSE and CNSU, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

