Monday Poster Session
Category: Small Intestine
P4042 - Trends in Endoscopic Therapy and Survival Outcomes in Patients With Early-stage Duodenal Neuroendocrine Tumors: A Surveillance Epidemiology and End Results (SEER) Analysis From 2004 to 2022
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chawin Lopimpisuth, MD
University of Miami Miller School of Medicine at Jackson Memorial Hospital
Miami, FL
Presenting Author(s)
Chawin Lopimpisuth, MD1, Shyam Vedantam, DO2, Pojsakorn Danpanichkul, MD3, Mahmoud Mahfouz, MD4, Jordan Orr, MD4, Shria Kumar, MD, MSCE4, Jodie A. Barkin, MD, FACG4, Sunil Amin, MD, MPH5, Sean Bhalla, MD4
1University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 2University of Miami, Miami, FL; 3Department of Internal Medicine, Texas Tech University Healt, Lubbock, TX; 4University of Miami Miller School of Medicine, Miami, FL; 5University of Miami Health System, Miami, FL
Introduction: Duodenal neuroendocrine tumors (D-NETs) are rare, yet are the most common type of small bowel neoplasms. Despite growth in endoscopic therapy (ET), current European guidelines recommend surgical resection (SR) over ET for high-risk D-NETs (ie tumor size >10mm or invasion beyond the submucosa) due to risk of lymph node metastasis (LNM). We aim to investigate the trend and survival outcomes of patients with early-stage D-NETs treated with ET vs SR.
Methods: The National Cancer Institute SEER program, the SEER17 registry, was used to extract data on adult patients (age>18yr) with histologically confirmed D-NET with T1-2 staging, diagnosed in 2004-2022. We compared characteristics and trends in use of ET. Multivariate logistic regression was used to identify factors associated with ET. Cancer-specific survival (CSS) and overall survival (OS) were calculated using Kaplan-Meier’s (KM) estimate and the log-rank test. A Cox proportional hazards model was performed after controlling for other covariates.
Results: 3,406 patients with T1-2 D-NET were identified (median age 65; 49.8% male; 53.1% White). Overall, 2,543 patients underwent tumor resection (1,761 ET vs 782 SR). Baseline characteristics were compared and shown in Table 1. There was an increase in ET over time (65.5% in 2012 to 82.0% in 2022) (Fig 1a). In multivariate logistic regression, ET was more likely in female patients (OR 1.22, 95%CI 1.00-1.49, p=0.05), 2018-2022 (OR 2.88, 95%CI 1.39-5.98, p< 0.01), T1 stage (OR 2.38, 95%CI 1.57-3.60, p< 0.01), well-differentiated tumor (OR 1.38, 95%CI 1.00-1.89, p=0.04), and no LNM (OR 21.8, 95%CI 12.80-36.96, p< 0.01). Median follow-up time was 43 months. The 5-year OS in ET was similar to SR (5-yr OS ET 82.0% vs 80.2%, p=0.52, Fig 1b). The 5-year CSS was significantly higher in ET group (5-yr CSS ET 98.1% vs 95.8%, p=0.04, Fig 1c). In subgroup analysis of tumor size 11–20 mm, 5-year CSS was similar in ET and SR (5-yr CSS ET 96.7% vs 95.5%, p=0.57, Fig 1d). In a Cox proportional hazards model, there was no significant difference in either overall mortality (hazard ratio (HR) 1.01, 95%CI 0.82-1.24, p=0.90) or cancer-specific mortality (HR 0.69, 95%CI 0.38-1.25, p=0.23) between ET and SR.
Discussion: We found a rising trend in the use of ET for D-NETs in the past decade. 5-year CSS was higher in the ET group, however, OS remained similar. In larger D-NETs (11-20 mm), patients who received ET and SR exhibited comparable long-term survival outcomes, indicating that ET is a viable treatment option.
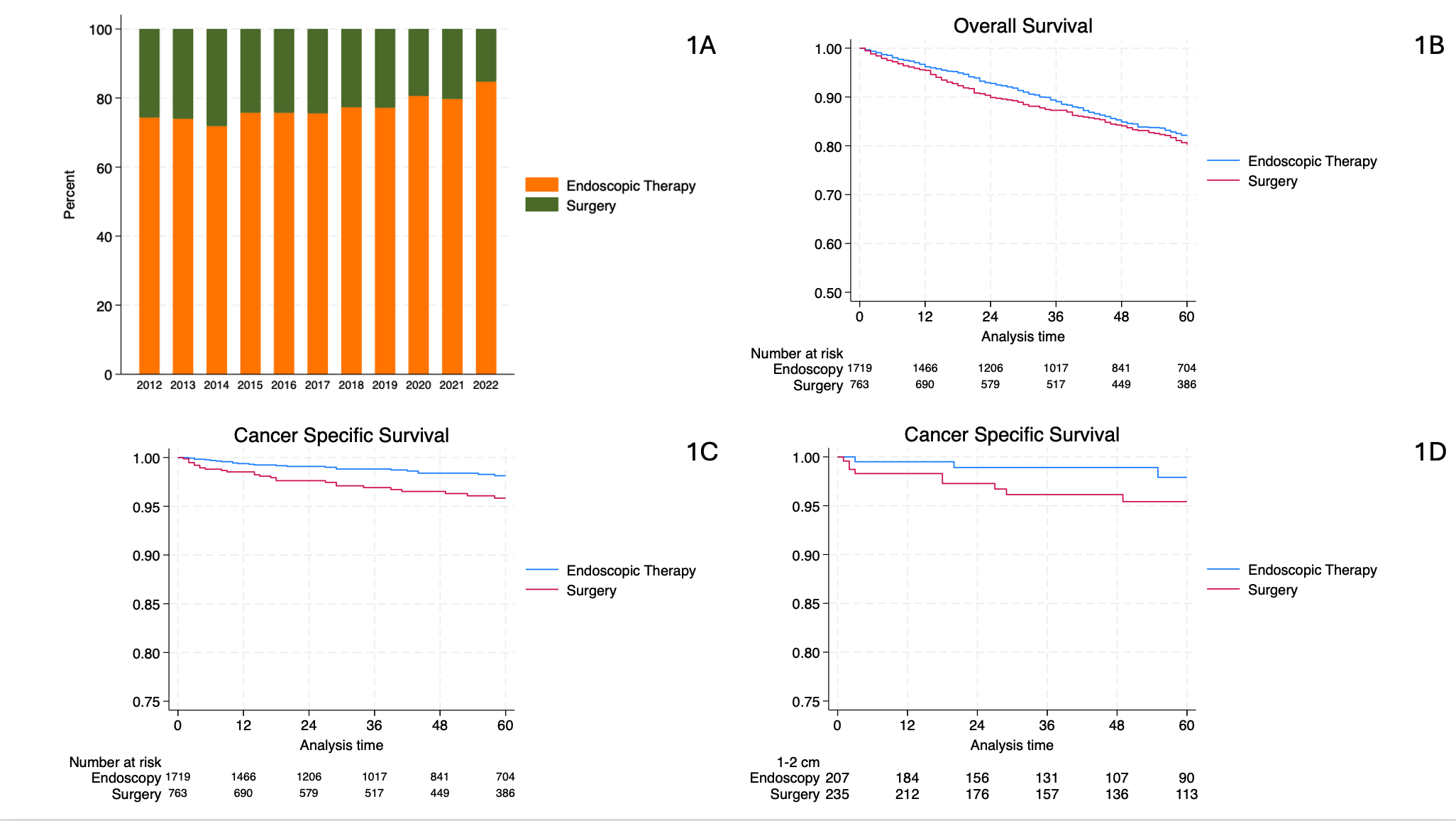
Figure: Figure 1: (A) Trends in treatment of early-stage duodenal neuroendocrine tumor from 2012 to 2022. (B) The 5-year overall survival in endoscopic therapy vs surgery groups. (C) The 5-year cancer-specific survival in endoscopic therapy vs surgery groups. (D) The 5-year cancer-specific survival for tumor size 11-20mm in endoscopic therapy vs surgery groups.
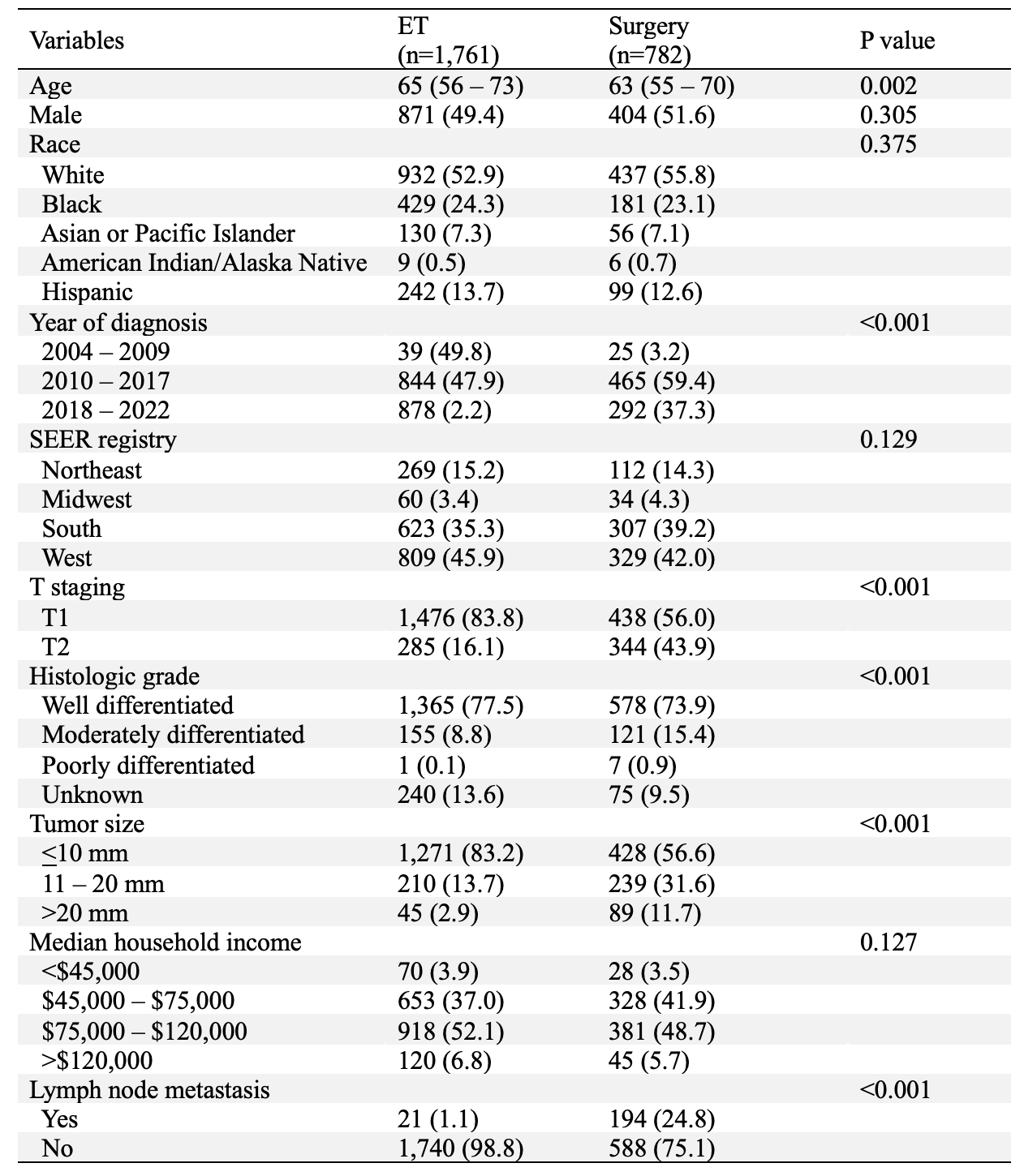
Figure: Table 1: Characteristics of patients with early-stage duodenal neuroendocrine tumors
† Continuous variables presented as median and IQR; categorical variables presented as N (%)
Disclosures:
Chawin Lopimpisuth indicated no relevant financial relationships.
Shyam Vedantam indicated no relevant financial relationships.
Pojsakorn Danpanichkul indicated no relevant financial relationships.
Mahmoud Mahfouz indicated no relevant financial relationships.
Jordan Orr indicated no relevant financial relationships.
Shria Kumar: Phathom Pharmaceuticals – Grant/Research Support, Unrelated to this work. TriMed Americas – Grant/Research Support, Unrelated to this work.
Jodie Barkin: AbbVie – Advisor or Review Panel Member. Aimmune Therapeutics – Advisor or Review Panel Member. Amgen – Consultant. CorEvitas – Consultant. Iterative Health – Consultant. Medtronic – Consultant. MotusGI – Consultant.
Sunil Amin: 3D Matrix – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Sean Bhalla indicated no relevant financial relationships.
Chawin Lopimpisuth, MD1, Shyam Vedantam, DO2, Pojsakorn Danpanichkul, MD3, Mahmoud Mahfouz, MD4, Jordan Orr, MD4, Shria Kumar, MD, MSCE4, Jodie A. Barkin, MD, FACG4, Sunil Amin, MD, MPH5, Sean Bhalla, MD4. P4042 - Trends in Endoscopic Therapy and Survival Outcomes in Patients With Early-stage Duodenal Neuroendocrine Tumors: A Surveillance Epidemiology and End Results (SEER) Analysis From 2004 to 2022, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at Jackson Memorial Hospital, Miami, FL; 2University of Miami, Miami, FL; 3Department of Internal Medicine, Texas Tech University Healt, Lubbock, TX; 4University of Miami Miller School of Medicine, Miami, FL; 5University of Miami Health System, Miami, FL
Introduction: Duodenal neuroendocrine tumors (D-NETs) are rare, yet are the most common type of small bowel neoplasms. Despite growth in endoscopic therapy (ET), current European guidelines recommend surgical resection (SR) over ET for high-risk D-NETs (ie tumor size >10mm or invasion beyond the submucosa) due to risk of lymph node metastasis (LNM). We aim to investigate the trend and survival outcomes of patients with early-stage D-NETs treated with ET vs SR.
Methods: The National Cancer Institute SEER program, the SEER17 registry, was used to extract data on adult patients (age>18yr) with histologically confirmed D-NET with T1-2 staging, diagnosed in 2004-2022. We compared characteristics and trends in use of ET. Multivariate logistic regression was used to identify factors associated with ET. Cancer-specific survival (CSS) and overall survival (OS) were calculated using Kaplan-Meier’s (KM) estimate and the log-rank test. A Cox proportional hazards model was performed after controlling for other covariates.
Results: 3,406 patients with T1-2 D-NET were identified (median age 65; 49.8% male; 53.1% White). Overall, 2,543 patients underwent tumor resection (1,761 ET vs 782 SR). Baseline characteristics were compared and shown in Table 1. There was an increase in ET over time (65.5% in 2012 to 82.0% in 2022) (Fig 1a). In multivariate logistic regression, ET was more likely in female patients (OR 1.22, 95%CI 1.00-1.49, p=0.05), 2018-2022 (OR 2.88, 95%CI 1.39-5.98, p< 0.01), T1 stage (OR 2.38, 95%CI 1.57-3.60, p< 0.01), well-differentiated tumor (OR 1.38, 95%CI 1.00-1.89, p=0.04), and no LNM (OR 21.8, 95%CI 12.80-36.96, p< 0.01). Median follow-up time was 43 months. The 5-year OS in ET was similar to SR (5-yr OS ET 82.0% vs 80.2%, p=0.52, Fig 1b). The 5-year CSS was significantly higher in ET group (5-yr CSS ET 98.1% vs 95.8%, p=0.04, Fig 1c). In subgroup analysis of tumor size 11–20 mm, 5-year CSS was similar in ET and SR (5-yr CSS ET 96.7% vs 95.5%, p=0.57, Fig 1d). In a Cox proportional hazards model, there was no significant difference in either overall mortality (hazard ratio (HR) 1.01, 95%CI 0.82-1.24, p=0.90) or cancer-specific mortality (HR 0.69, 95%CI 0.38-1.25, p=0.23) between ET and SR.
Discussion: We found a rising trend in the use of ET for D-NETs in the past decade. 5-year CSS was higher in the ET group, however, OS remained similar. In larger D-NETs (11-20 mm), patients who received ET and SR exhibited comparable long-term survival outcomes, indicating that ET is a viable treatment option.
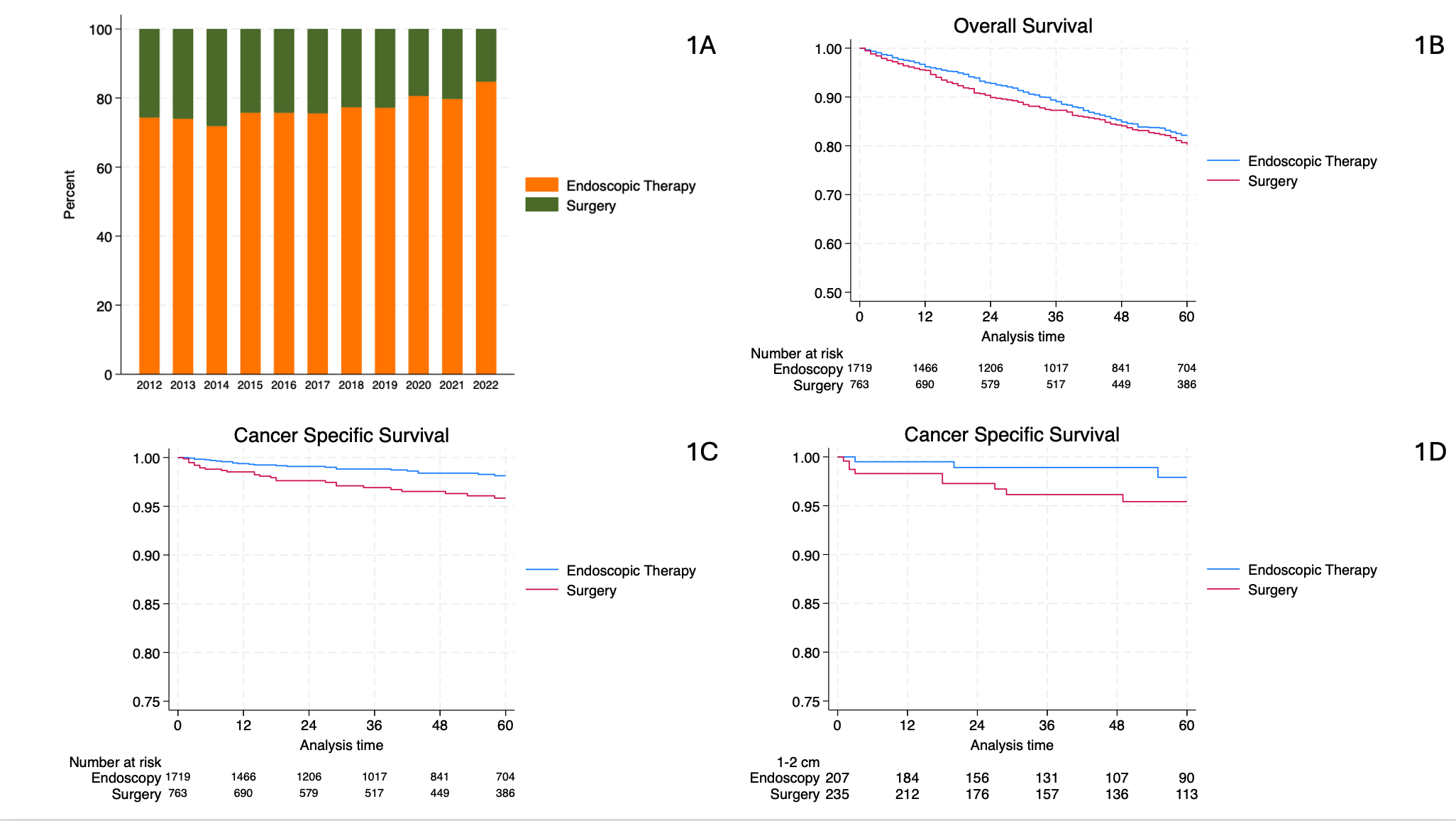
Figure: Figure 1: (A) Trends in treatment of early-stage duodenal neuroendocrine tumor from 2012 to 2022. (B) The 5-year overall survival in endoscopic therapy vs surgery groups. (C) The 5-year cancer-specific survival in endoscopic therapy vs surgery groups. (D) The 5-year cancer-specific survival for tumor size 11-20mm in endoscopic therapy vs surgery groups.
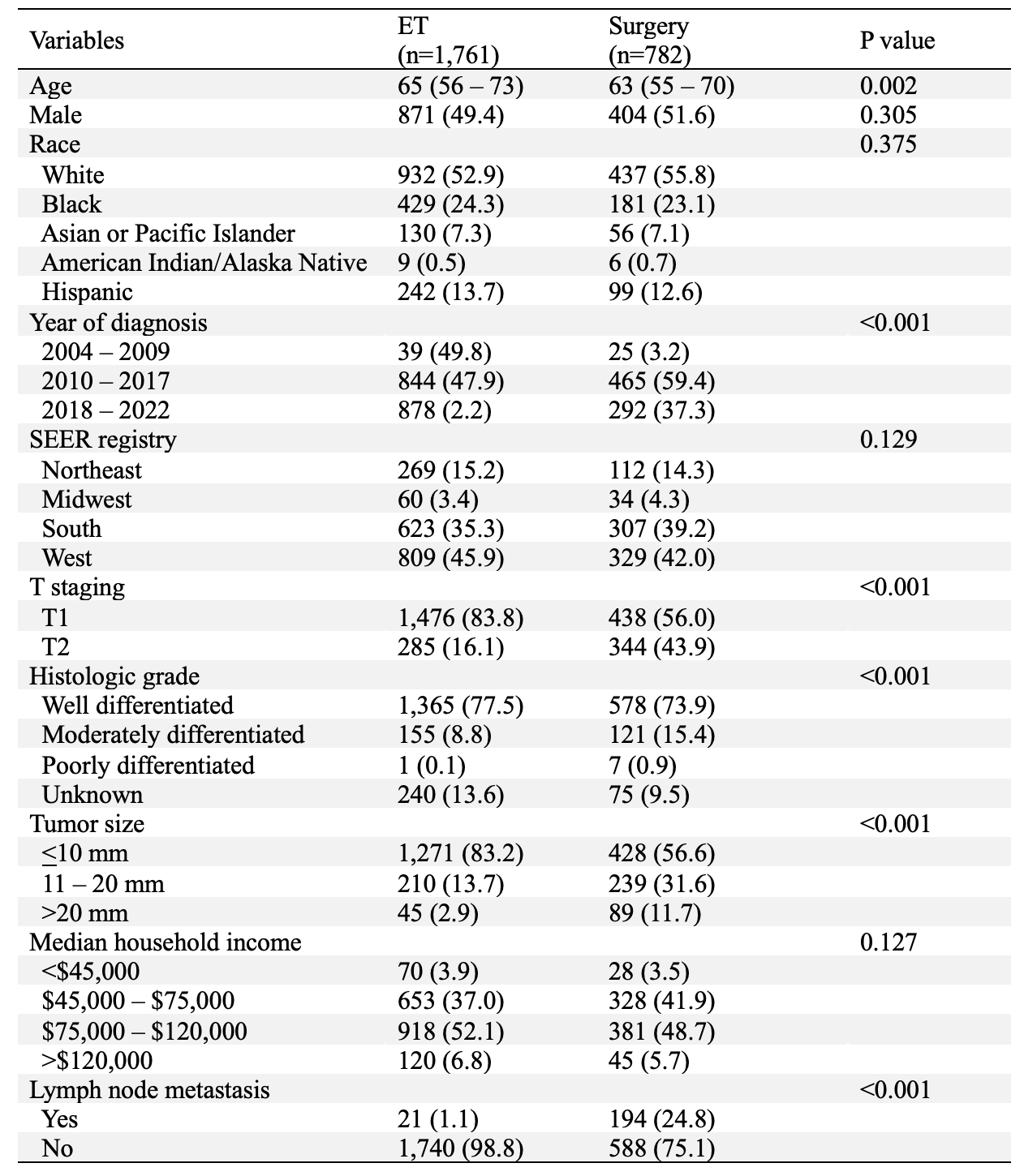
Figure: Table 1: Characteristics of patients with early-stage duodenal neuroendocrine tumors
† Continuous variables presented as median and IQR; categorical variables presented as N (%)
Disclosures:
Chawin Lopimpisuth indicated no relevant financial relationships.
Shyam Vedantam indicated no relevant financial relationships.
Pojsakorn Danpanichkul indicated no relevant financial relationships.
Mahmoud Mahfouz indicated no relevant financial relationships.
Jordan Orr indicated no relevant financial relationships.
Shria Kumar: Phathom Pharmaceuticals – Grant/Research Support, Unrelated to this work. TriMed Americas – Grant/Research Support, Unrelated to this work.
Jodie Barkin: AbbVie – Advisor or Review Panel Member. Aimmune Therapeutics – Advisor or Review Panel Member. Amgen – Consultant. CorEvitas – Consultant. Iterative Health – Consultant. Medtronic – Consultant. MotusGI – Consultant.
Sunil Amin: 3D Matrix – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Sean Bhalla indicated no relevant financial relationships.
Chawin Lopimpisuth, MD1, Shyam Vedantam, DO2, Pojsakorn Danpanichkul, MD3, Mahmoud Mahfouz, MD4, Jordan Orr, MD4, Shria Kumar, MD, MSCE4, Jodie A. Barkin, MD, FACG4, Sunil Amin, MD, MPH5, Sean Bhalla, MD4. P4042 - Trends in Endoscopic Therapy and Survival Outcomes in Patients With Early-stage Duodenal Neuroendocrine Tumors: A Surveillance Epidemiology and End Results (SEER) Analysis From 2004 to 2022, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
