Monday Poster Session
Category: Small Intestine
P4039 - Microscopic Colitis in Celiac Patients: A Hidden Driver of Malnutrition and Healthcare Utilization
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad Adam, MD, MSc
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Mohammad Adam, MD, MSc1, Ali Osman, MD2, Fatima Elmustafa, MBBS3, Ayman Elawad, MD4, Hazem Abosheaishaa, MD5, Mohamed Eldesouki, MD6, Mohamed A. Ebrahim, MD7, Miqdad Dafaallah, MD8, Samiksha Pandey, MD9, Muhammad Ibrahim Majeed, MD9, Monzer Abdalla, MD10, Mohamed Abdallah, MD11, Mohammad Bilal, MD, FACG12, Hassan Ghoz, MD13
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Washington University, Saint Louis, MO; 3Henry Ford Warren, Warren, MI; 4Massachusetts General Hospital, Harvard Medical School, Boston, MA; 5Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 6Saint Michael's Medical Center, New York Medical College, Newark, NJ; 7Ascension Saint Joseph Hospital, Chicago, IL; 8Mercyone Des Moines Medical Center, Iowa, IA; 9Corewell Health William Beaumont University Hospital, Royal Oak, MI; 10Rosalind Franklin University of Medicine and Science, Evanston, IL; 11Corewell Health, Royal Oak, MI; 12University of Colorado Anschutz Medical Campus, Denver, CO; 13University of Missouri Kansas City School of Medicine, Kansas City, MO
Introduction: Microscopic colitis (MC) is increasingly recognized as a comorbidity in patients with celiac disease (CD), particularly among those with persistent symptoms despite a gluten-free diet. However, the impact of coexisting MC on CD clinical outcomes remains underexplored. We aimed to evaluate the burden of malnutrition, healthcare utilization, and malignancy in patients with CD and concurrent MC (CD+MC) compared to those with isolated CD.
Methods: Using the TriNetX Global Research Network, we identified adult patients with CD only and matched them 1:1 with patients with CD+MC (n = 2,833 per group) based on age, sex, and comorbidities. We evaluated the incidence of malnutrition, emergency department (ED) visits, hospitalizations, and all-cause mortality. Hazard ratios (HRs) with 95% confidence intervals (CIs) and p-values were used to compare outcomes.
Results: Patients with CD+MC had a significantly higher risk of malnutrition compared to those with isolated CD (HR 0.71, 95% CI: 0.58–0.86; p = 0.001), as illustrated in Figure 1. ED visits and hospitalizations were modestly reduced in the CD+MC group (HR 0.88, 95% CI: 0.80–0.96; p = 0.006), as shown in Figure 2. A summary of outcome comparisons is provided in Table 2.
Discussion: Compared to patients with isolated CD, those with coexisting MC have a significantly greater risk of malnutrition, likely driven by chronic diarrhea, accelerated intestinal transit, and compounded nutrient loss, despite the colon not being a primary site for nutrient absorption. Healthcare utilization was comparable or modestly lower, and mortality risk was not significantly different. Clinicians should maintain a high index of suspicion for MC in CD patients with persistent symptoms and proactively assess for nutritional deficiencies.
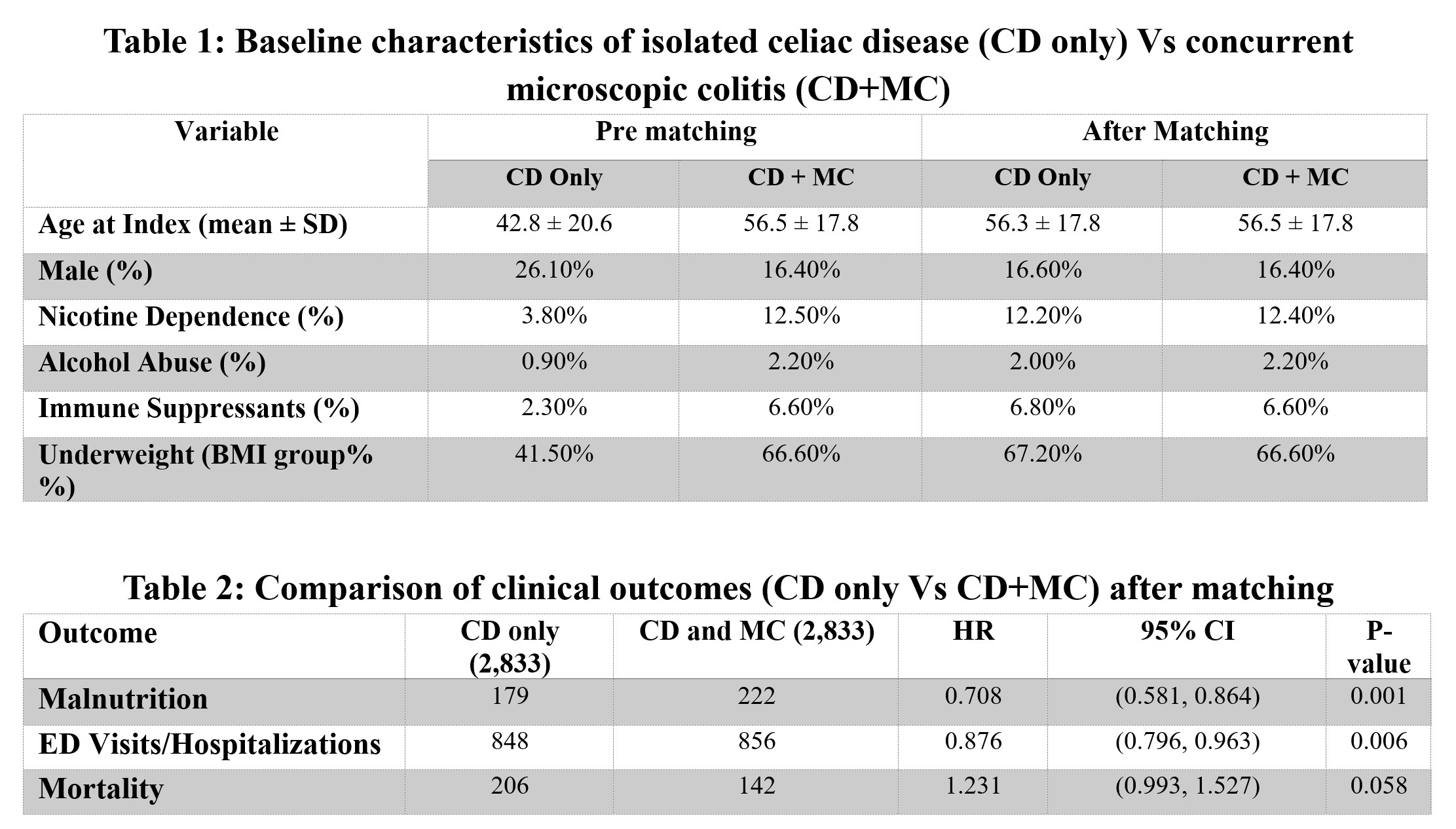
Figure: Table 1. Baseline characteristics of patients with isolated celiac disease (CD only) and those with concurrent microscopic colitis (CD+MC) before and after 1:1 propensity score matching based on age, sex, and comorbidities.
Table 2. Comparison of clinical outcomes between CD only and CD+MC groups after matching, including hazard ratios (HR), 95% confidence intervals (CI), and p-values for malnutrition, emergency department visits or hospitalizations, and all-cause mortality.
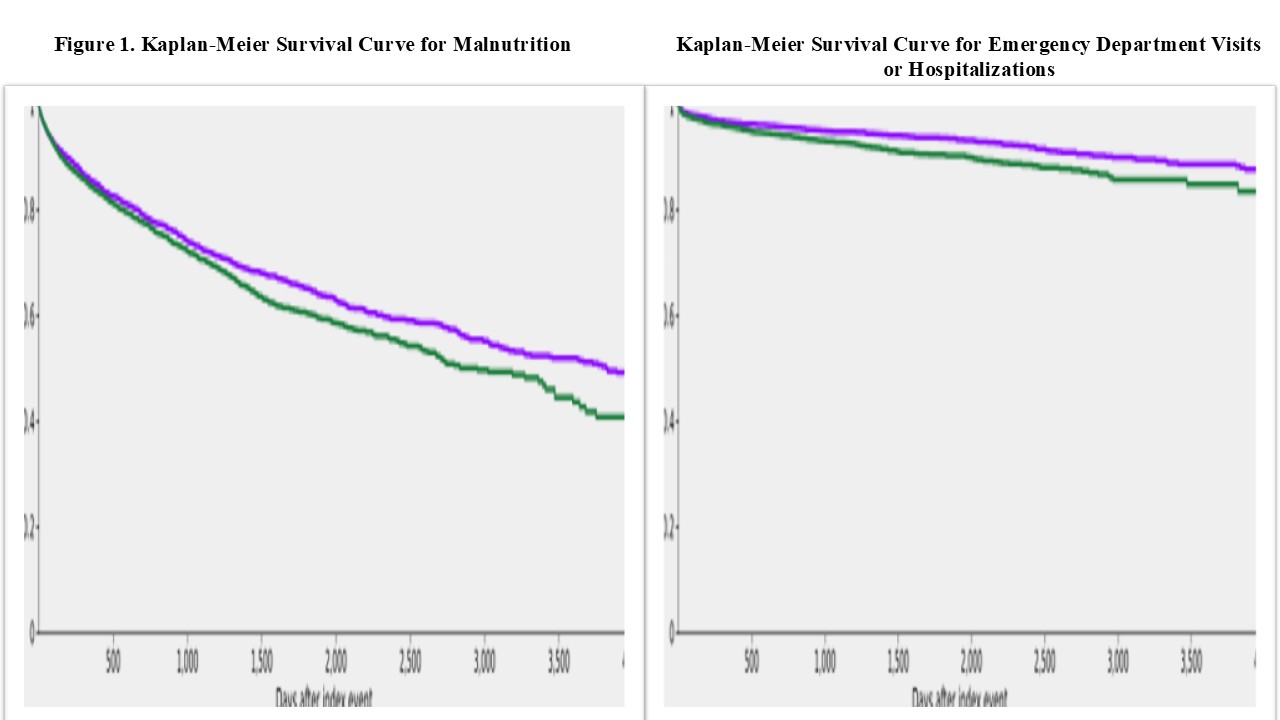
Figure: Figure 1. Kaplan-Meier Survival Curve for Malnutrition (Comparison of malnutrition risk over time between CD only and CD+MC groups).
Figure 2. Kaplan-Meier Survival Curve for Emergency Department Visits or Hospitalizations (Comparison of ED visit or hospitalization rates over time between CD only and CD+MC groups).
Disclosures:
Mohammad Adam indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Fatima Elmustafa indicated no relevant financial relationships.
Ayman Elawad indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Mohamed Ebrahim indicated no relevant financial relationships.
Miqdad Dafaallah indicated no relevant financial relationships.
Samiksha Pandey indicated no relevant financial relationships.
Muhammad Ibrahim Majeed indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Hassan Ghoz indicated no relevant financial relationships.
Mohammad Adam, MD, MSc1, Ali Osman, MD2, Fatima Elmustafa, MBBS3, Ayman Elawad, MD4, Hazem Abosheaishaa, MD5, Mohamed Eldesouki, MD6, Mohamed A. Ebrahim, MD7, Miqdad Dafaallah, MD8, Samiksha Pandey, MD9, Muhammad Ibrahim Majeed, MD9, Monzer Abdalla, MD10, Mohamed Abdallah, MD11, Mohammad Bilal, MD, FACG12, Hassan Ghoz, MD13. P4039 - Microscopic Colitis in Celiac Patients: A Hidden Driver of Malnutrition and Healthcare Utilization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Washington University, Saint Louis, MO; 3Henry Ford Warren, Warren, MI; 4Massachusetts General Hospital, Harvard Medical School, Boston, MA; 5Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 6Saint Michael's Medical Center, New York Medical College, Newark, NJ; 7Ascension Saint Joseph Hospital, Chicago, IL; 8Mercyone Des Moines Medical Center, Iowa, IA; 9Corewell Health William Beaumont University Hospital, Royal Oak, MI; 10Rosalind Franklin University of Medicine and Science, Evanston, IL; 11Corewell Health, Royal Oak, MI; 12University of Colorado Anschutz Medical Campus, Denver, CO; 13University of Missouri Kansas City School of Medicine, Kansas City, MO
Introduction: Microscopic colitis (MC) is increasingly recognized as a comorbidity in patients with celiac disease (CD), particularly among those with persistent symptoms despite a gluten-free diet. However, the impact of coexisting MC on CD clinical outcomes remains underexplored. We aimed to evaluate the burden of malnutrition, healthcare utilization, and malignancy in patients with CD and concurrent MC (CD+MC) compared to those with isolated CD.
Methods: Using the TriNetX Global Research Network, we identified adult patients with CD only and matched them 1:1 with patients with CD+MC (n = 2,833 per group) based on age, sex, and comorbidities. We evaluated the incidence of malnutrition, emergency department (ED) visits, hospitalizations, and all-cause mortality. Hazard ratios (HRs) with 95% confidence intervals (CIs) and p-values were used to compare outcomes.
Results: Patients with CD+MC had a significantly higher risk of malnutrition compared to those with isolated CD (HR 0.71, 95% CI: 0.58–0.86; p = 0.001), as illustrated in Figure 1. ED visits and hospitalizations were modestly reduced in the CD+MC group (HR 0.88, 95% CI: 0.80–0.96; p = 0.006), as shown in Figure 2. A summary of outcome comparisons is provided in Table 2.
Discussion: Compared to patients with isolated CD, those with coexisting MC have a significantly greater risk of malnutrition, likely driven by chronic diarrhea, accelerated intestinal transit, and compounded nutrient loss, despite the colon not being a primary site for nutrient absorption. Healthcare utilization was comparable or modestly lower, and mortality risk was not significantly different. Clinicians should maintain a high index of suspicion for MC in CD patients with persistent symptoms and proactively assess for nutritional deficiencies.
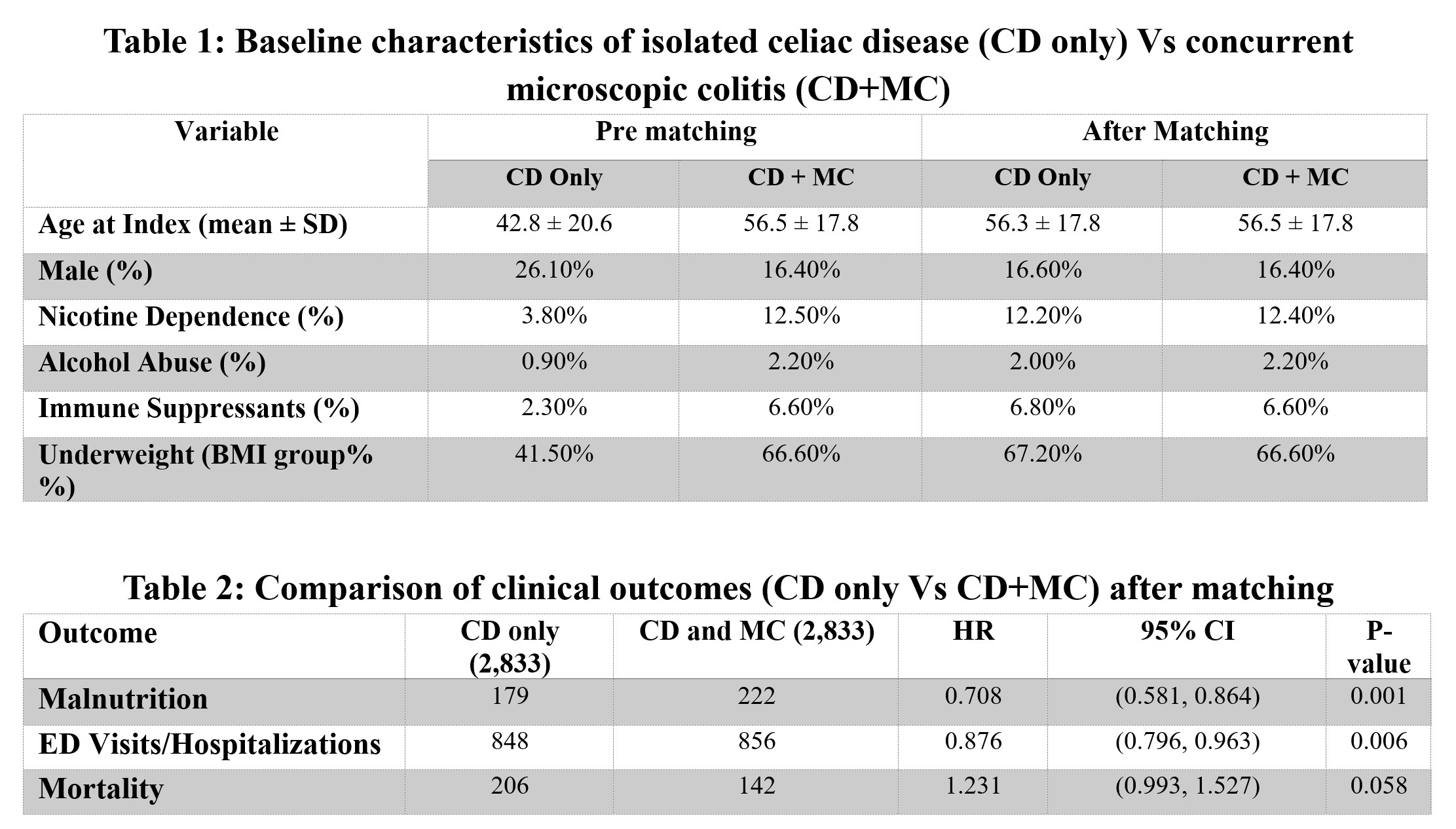
Figure: Table 1. Baseline characteristics of patients with isolated celiac disease (CD only) and those with concurrent microscopic colitis (CD+MC) before and after 1:1 propensity score matching based on age, sex, and comorbidities.
Table 2. Comparison of clinical outcomes between CD only and CD+MC groups after matching, including hazard ratios (HR), 95% confidence intervals (CI), and p-values for malnutrition, emergency department visits or hospitalizations, and all-cause mortality.
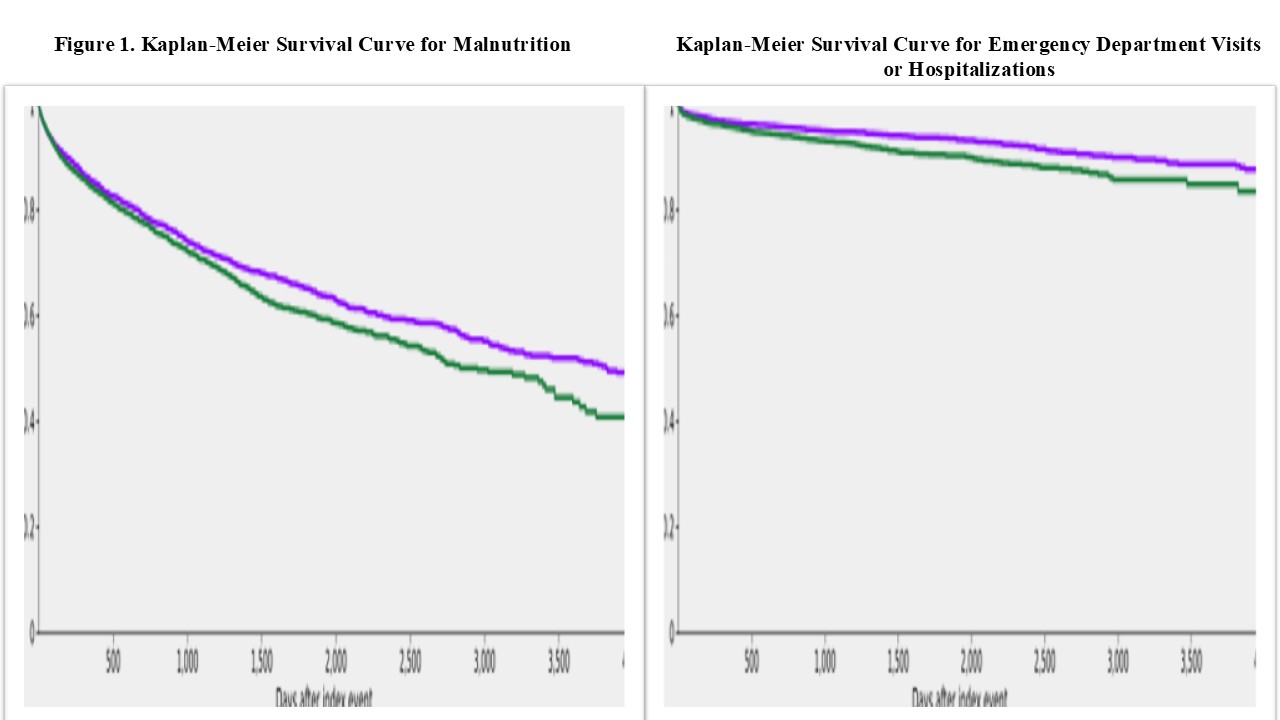
Figure: Figure 1. Kaplan-Meier Survival Curve for Malnutrition (Comparison of malnutrition risk over time between CD only and CD+MC groups).
Figure 2. Kaplan-Meier Survival Curve for Emergency Department Visits or Hospitalizations (Comparison of ED visit or hospitalization rates over time between CD only and CD+MC groups).
Disclosures:
Mohammad Adam indicated no relevant financial relationships.
Ali Osman indicated no relevant financial relationships.
Fatima Elmustafa indicated no relevant financial relationships.
Ayman Elawad indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Mohamed Ebrahim indicated no relevant financial relationships.
Miqdad Dafaallah indicated no relevant financial relationships.
Samiksha Pandey indicated no relevant financial relationships.
Muhammad Ibrahim Majeed indicated no relevant financial relationships.
Monzer Abdalla indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Hassan Ghoz indicated no relevant financial relationships.
Mohammad Adam, MD, MSc1, Ali Osman, MD2, Fatima Elmustafa, MBBS3, Ayman Elawad, MD4, Hazem Abosheaishaa, MD5, Mohamed Eldesouki, MD6, Mohamed A. Ebrahim, MD7, Miqdad Dafaallah, MD8, Samiksha Pandey, MD9, Muhammad Ibrahim Majeed, MD9, Monzer Abdalla, MD10, Mohamed Abdallah, MD11, Mohammad Bilal, MD, FACG12, Hassan Ghoz, MD13. P4039 - Microscopic Colitis in Celiac Patients: A Hidden Driver of Malnutrition and Healthcare Utilization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
