Monday Poster Session
Category: Small Intestine
P4038 - Trends and Discrepancies in Mortality Due to Chronic Intestinal Vascular Disorders in the Elderly: A CDC WONDER Analysis (1999–2023)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MK
Musa Khalil, MD (he/him/his)
Howard University Hospital
Washington, DC
Presenting Author(s)
Rizwana Noor, 1, Musa Khalil, MD2, Sadaf Iftikhar, MBBS3, Muhammad Abdullah, MBBS4, Angesom Kibreab, MD2
1Khyber Medical College, Peshawar, North-West Frontier, Pakistan; 2Howard University Hospital, Washington, DC; 3Akhtar Saeed Medical and dental college, Lahore, Punjab, Pakistan; 4Shalamar Institute of Health Sciences, Lahore, Punjab, Pakistan
Introduction: Chronic intestinal vascular disorders are underdiagnosed, progressive disorders, often resulting from long-standing arterial insufficiency and leading to intestinal hypoperfusion and ischemic injury. This study utilizes nationwide data across two decades to observe mortality trends among adults aged 65 and above.
Methods: Data was extracted from CDC WONDER focusing on ICD-10 code K55.1 for chronic intestinal vascular disorders. Age-adjusted mortality rates (AAMRs) were calculated per 1,000,000 population. Annual percent change (APC), and average annual precent change (AAPC) with 95% Confidence Interval (CI) were evaluated using Joinpoint software.
Results: Chronic intestinal vascular disorders accounted for 8,703 deaths. The overall AAMR rose from 8.59 in 1999 to 11.26 in 2023, (AAPC of 1.10 (95% CI: 0.22 to 2.09). The AAMR significantly decreased till 2007 (APC -6.50, 95% CI: -14.36 to -2.57), preceding a sharp rise till 2023 (APC: 5.13, 95% CI: 3.94 to 7.14). Females consistently exhibited higher mortality rates than males and steeper trends (AAPC: 1.28, 95% CI: 0.13 to 2.81) compared to males (AAPC: 0.82, 95% CI: -0.25 to 1.98). Racially, Hispanics experienced the sharpest rise (AAPC: 9.50, 95% CI: 3.33 to 17.84), followed by the NH Blacks (AAPC: 1.95, 95% CI: -4.14 to 10.49) and NH Whites (AAPC: 1.29, 95% CI: 0.42 to 2.27).
The Northeast region saw the most pronounced increase (AAPC: 2.34, 95% CI: 1.13 to 3.86), followed by the West (AAPC: 1.26, 95% CI: -0.11 to 2.82). Non-metropolitan areas exhibited higher AAMRs than metropolitan areas, with larger AAPCs (1.28, 95% CI: -0.68 to 3.51). Age-stratification revealed that individuals aged 75-84 years bore the highest mortality burden, with an AAPC of 1.27 (95% CI: 0.01 to 2.81), followed by the 65-74 years age group (AAPC: 1.21, 95% CI: 0.16 to 2.53).
Discussion: The rising mortality from Chronic intestinal vascular disorders in the elderly highlights underdiagnosis and delayed interventions over the years. Higher female mortality rates could stem from physiological differences or disparities in care. Hispanics and the rural populations showed a pronounced rise, suggesting structural inequities in healthcare delivery. Similarly, regional variations, as seen in the West and Northeast, reflect differences in healthcare availability or environmental risk factors. These findings underscore the need for targeted interventions and strategies in high risk groups.
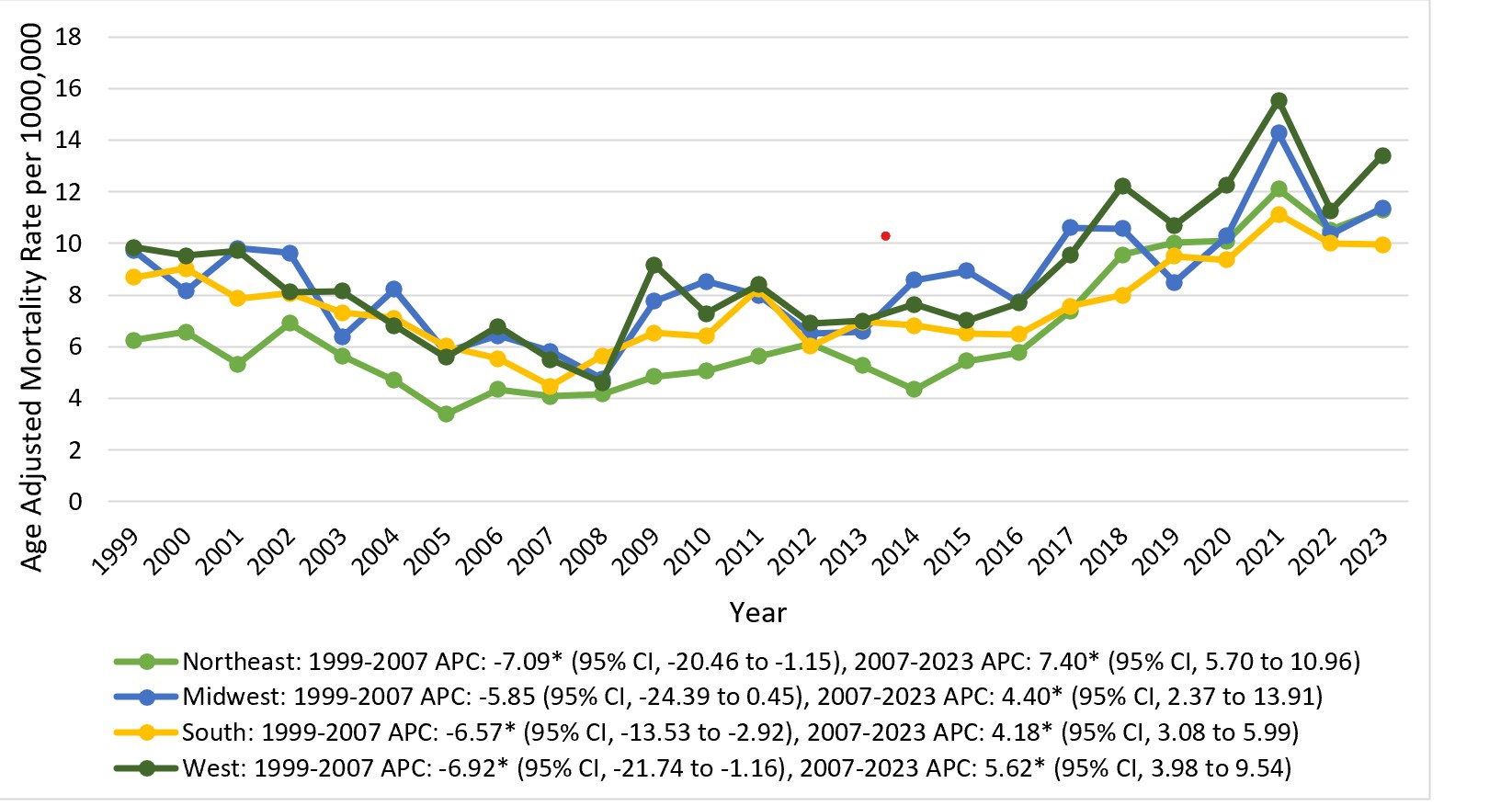
Figure: Figure 1. Trends in chronic intestinal vascular disorder-related mortality stratified by the sex in the United States from 1999 to 2023.
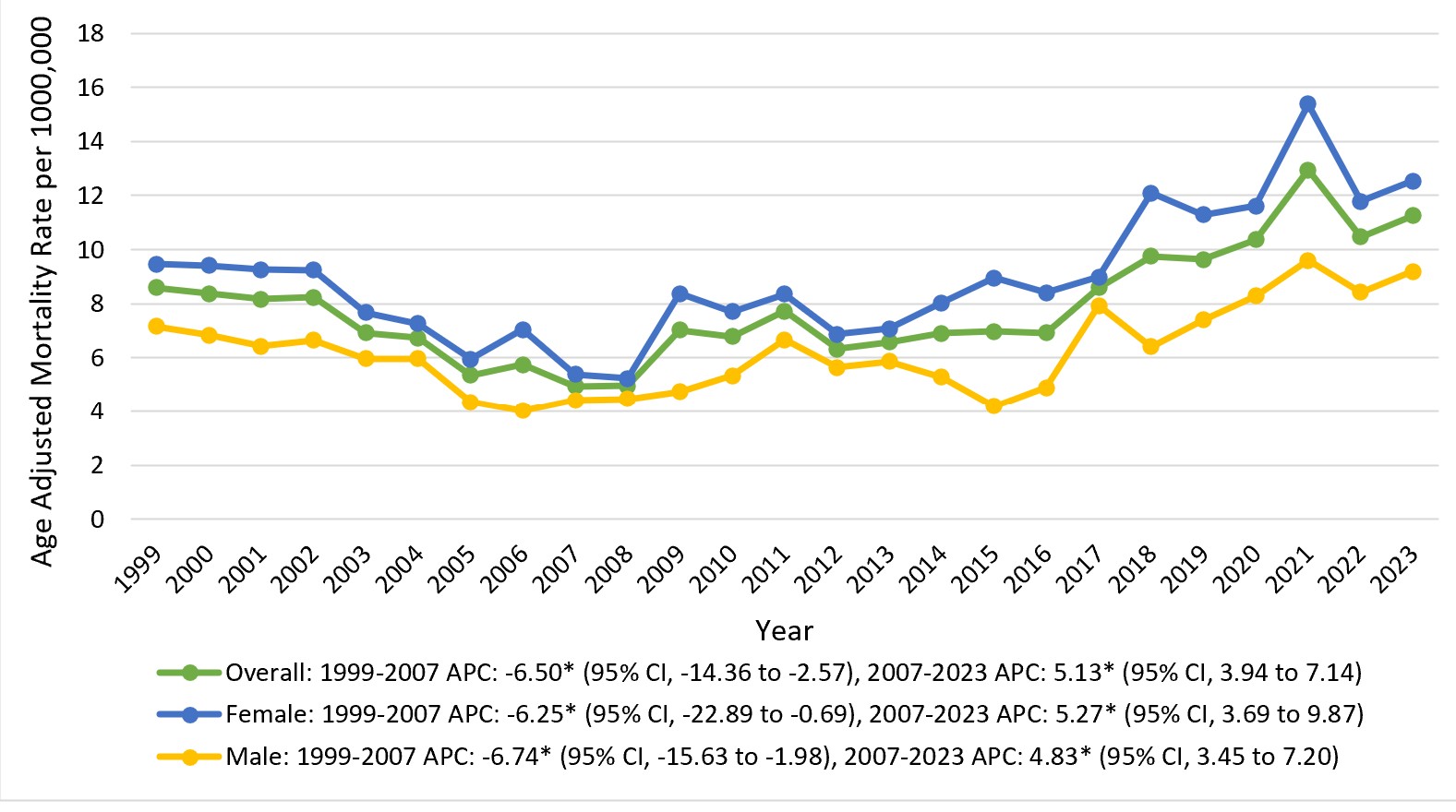
Figure: Figure 2. Trends in chronic intestinal vascular disorder-related mortality stratified by the census region in the United States from 1999 to 2023.
Disclosures:
Rizwana Noor indicated no relevant financial relationships.
Musa Khalil indicated no relevant financial relationships.
Sadaf Iftikhar indicated no relevant financial relationships.
Muhammad Abdullah indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Rizwana Noor, 1, Musa Khalil, MD2, Sadaf Iftikhar, MBBS3, Muhammad Abdullah, MBBS4, Angesom Kibreab, MD2. P4038 - Trends and Discrepancies in Mortality Due to Chronic Intestinal Vascular Disorders in the Elderly: A CDC WONDER Analysis (1999–2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Khyber Medical College, Peshawar, North-West Frontier, Pakistan; 2Howard University Hospital, Washington, DC; 3Akhtar Saeed Medical and dental college, Lahore, Punjab, Pakistan; 4Shalamar Institute of Health Sciences, Lahore, Punjab, Pakistan
Introduction: Chronic intestinal vascular disorders are underdiagnosed, progressive disorders, often resulting from long-standing arterial insufficiency and leading to intestinal hypoperfusion and ischemic injury. This study utilizes nationwide data across two decades to observe mortality trends among adults aged 65 and above.
Methods: Data was extracted from CDC WONDER focusing on ICD-10 code K55.1 for chronic intestinal vascular disorders. Age-adjusted mortality rates (AAMRs) were calculated per 1,000,000 population. Annual percent change (APC), and average annual precent change (AAPC) with 95% Confidence Interval (CI) were evaluated using Joinpoint software.
Results: Chronic intestinal vascular disorders accounted for 8,703 deaths. The overall AAMR rose from 8.59 in 1999 to 11.26 in 2023, (AAPC of 1.10 (95% CI: 0.22 to 2.09). The AAMR significantly decreased till 2007 (APC -6.50, 95% CI: -14.36 to -2.57), preceding a sharp rise till 2023 (APC: 5.13, 95% CI: 3.94 to 7.14). Females consistently exhibited higher mortality rates than males and steeper trends (AAPC: 1.28, 95% CI: 0.13 to 2.81) compared to males (AAPC: 0.82, 95% CI: -0.25 to 1.98). Racially, Hispanics experienced the sharpest rise (AAPC: 9.50, 95% CI: 3.33 to 17.84), followed by the NH Blacks (AAPC: 1.95, 95% CI: -4.14 to 10.49) and NH Whites (AAPC: 1.29, 95% CI: 0.42 to 2.27).
The Northeast region saw the most pronounced increase (AAPC: 2.34, 95% CI: 1.13 to 3.86), followed by the West (AAPC: 1.26, 95% CI: -0.11 to 2.82). Non-metropolitan areas exhibited higher AAMRs than metropolitan areas, with larger AAPCs (1.28, 95% CI: -0.68 to 3.51). Age-stratification revealed that individuals aged 75-84 years bore the highest mortality burden, with an AAPC of 1.27 (95% CI: 0.01 to 2.81), followed by the 65-74 years age group (AAPC: 1.21, 95% CI: 0.16 to 2.53).
Discussion: The rising mortality from Chronic intestinal vascular disorders in the elderly highlights underdiagnosis and delayed interventions over the years. Higher female mortality rates could stem from physiological differences or disparities in care. Hispanics and the rural populations showed a pronounced rise, suggesting structural inequities in healthcare delivery. Similarly, regional variations, as seen in the West and Northeast, reflect differences in healthcare availability or environmental risk factors. These findings underscore the need for targeted interventions and strategies in high risk groups.
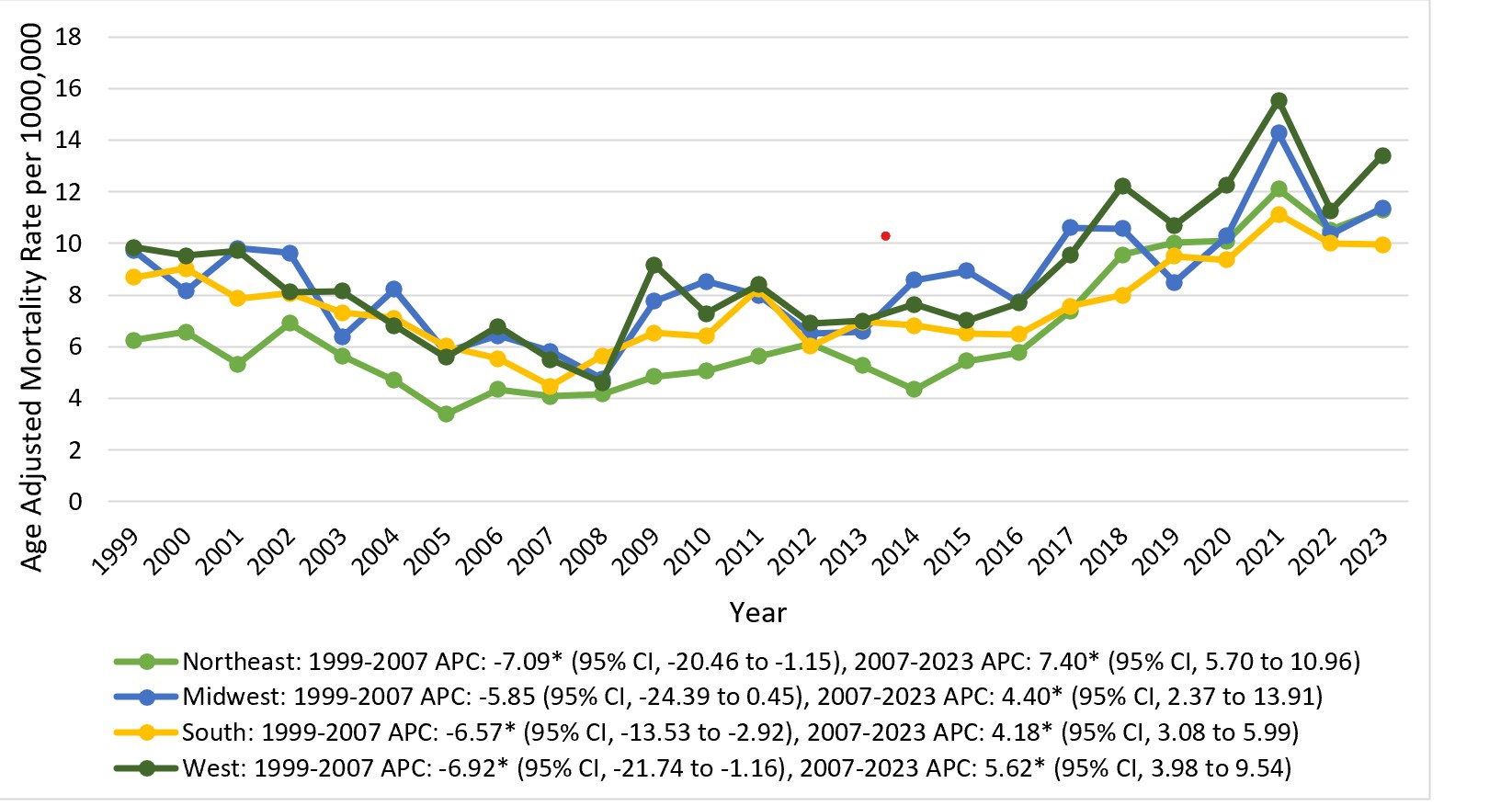
Figure: Figure 1. Trends in chronic intestinal vascular disorder-related mortality stratified by the sex in the United States from 1999 to 2023.
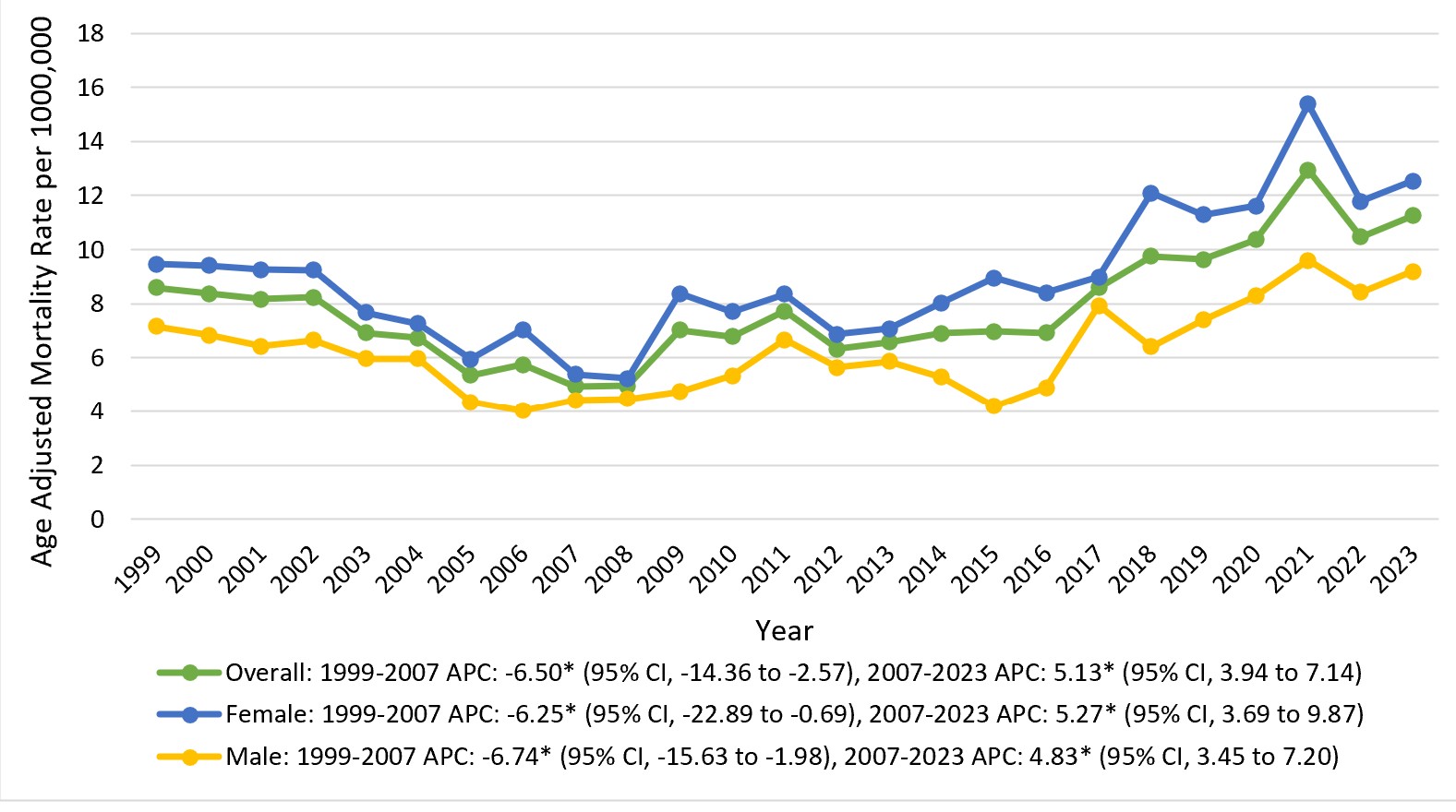
Figure: Figure 2. Trends in chronic intestinal vascular disorder-related mortality stratified by the census region in the United States from 1999 to 2023.
Disclosures:
Rizwana Noor indicated no relevant financial relationships.
Musa Khalil indicated no relevant financial relationships.
Sadaf Iftikhar indicated no relevant financial relationships.
Muhammad Abdullah indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Rizwana Noor, 1, Musa Khalil, MD2, Sadaf Iftikhar, MBBS3, Muhammad Abdullah, MBBS4, Angesom Kibreab, MD2. P4038 - Trends and Discrepancies in Mortality Due to Chronic Intestinal Vascular Disorders in the Elderly: A CDC WONDER Analysis (1999–2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
