Monday Poster Session
Category: Liver
P4006 - Severe Portal Hypertension From Late-Diagnosed JAK2-Associated PVT: Time for a Paradigm Shift in Earlier Assessment
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Justin Lin, MD (he/him/his)
Northwell Health
New Hyde Park, NY
Presenting Author(s)
Justin Lin, MD1, Michelle Shi, MD2, Jang Kim, MD2, Harmit Singh. Kalia, DO2
1Northwell Health, New Hyde Park, NY; 2Northwell Health, Manhasset, NY
Introduction: Portal vein thrombosis (PVT) driven by JAK2 V617F is a significant cause of non-cirrhotic portal hypertension. Delayed diagnosis is common leading to irreversible complications like life-threatening variceal bleeding. When patients present with massive hematemesis from chronic PVT with cavernous transformation, emergent interventions are severely limited and high-risk. These cases illustrate how diagnostic delays restrict therapeutic options, underscoring the urgent need for earlier identification of hypercoagulable states before catastrophic presentations.
Case Description/
Methods: A 23-year-old woman with alpha-thalassemia intermedia presented with hematemesis. EGD showed large esophageal and Type 2 gastroesophageal varices. CT showed extensive chronic PVT with complete portal vein and portosplenic confluence occlusion with cavernous transformation. Workup was positive for JAK2 V617F, though not meeting full overt myeloproliferative neoplasm criteria. Anticoagulation was deferred due to high bleeding risk. Recanalization (TIPS, thrombectomy) was infeasible due to chronicity. Management involved supportive care and repeat endoscopic band ligation. She faces ongoing risks from severe portal hypertension.
A 38-year-old man presented with hematemesis. Seven years prior, an admission for bloody diarrhea revealed splenomegaly, esophageal varices, and thrombocytosis with a patent portal vein, but no definitive etiology was established, and he was lost to follow-up. Current imaging confirmed extensive chronic PVT with cavernous transformation and complete splenic vein occlusion. EGD showed esophageal/gastric varices with an ulcer. Workup revealed extreme thrombocytosis from an underlying myeloproliferative neoplasm confirmed by bone marrow biopsy, with JAK2 V617F mutation. Similarly, chronicity precluded recanalization and anticoagulation was withheld due to bleeding risk. He continues to have severe portal hypertension.
Discussion: These cases of severe JAK2 V617F-associated PVT, diagnosed after massive hematemesis, faced severely limited therapies and profound complications. They underscore the critical need for earlier recognition and comprehensive hypercoagulability investigation in patients with unexplained early signs of portal hypertension, varices, splenomegaly, or hematologic abnormalities. Prompt identification of underlying prothrombotic states is paramount, allowing intervention before irreversible thrombosis and life-threatening hemorrhage develop, improving patient outcomes.

Figure: Case 1 CT of PVT, EGD image of EV
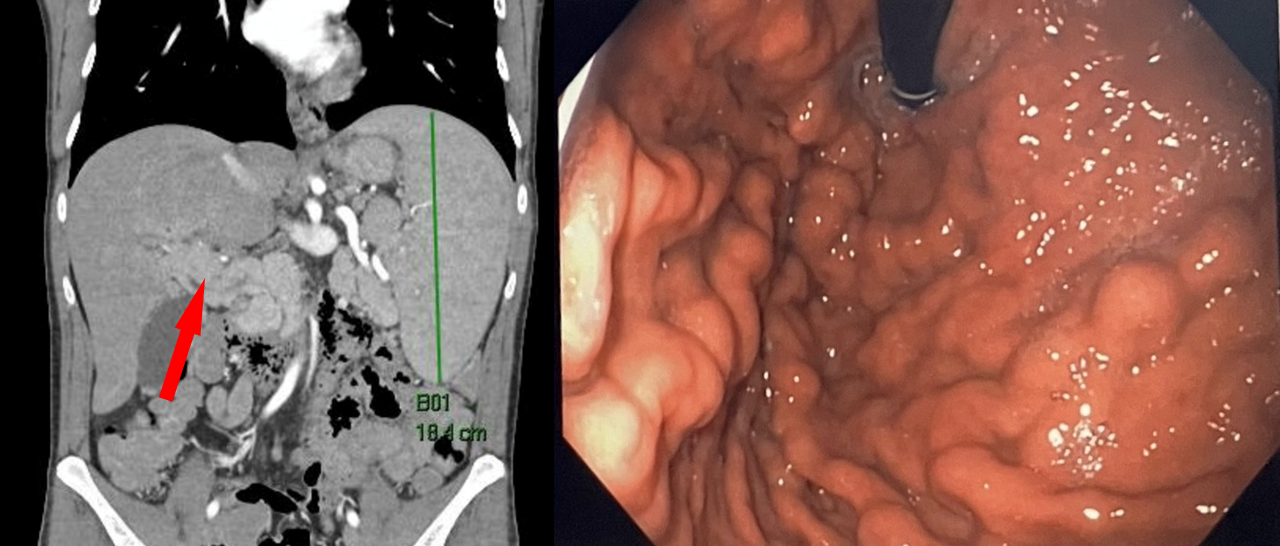
Figure: Case 2 CT of PVT, EGD image of Gastric Varices
Disclosures:
Justin Lin indicated no relevant financial relationships.
Michelle Shi indicated no relevant financial relationships.
Jang Kim indicated no relevant financial relationships.
Harmit Kalia indicated no relevant financial relationships.
Justin Lin, MD1, Michelle Shi, MD2, Jang Kim, MD2, Harmit Singh. Kalia, DO2. P4006 - Severe Portal Hypertension From Late-Diagnosed JAK2-Associated PVT: Time for a Paradigm Shift in Earlier Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, New Hyde Park, NY; 2Northwell Health, Manhasset, NY
Introduction: Portal vein thrombosis (PVT) driven by JAK2 V617F is a significant cause of non-cirrhotic portal hypertension. Delayed diagnosis is common leading to irreversible complications like life-threatening variceal bleeding. When patients present with massive hematemesis from chronic PVT with cavernous transformation, emergent interventions are severely limited and high-risk. These cases illustrate how diagnostic delays restrict therapeutic options, underscoring the urgent need for earlier identification of hypercoagulable states before catastrophic presentations.
Case Description/
Methods: A 23-year-old woman with alpha-thalassemia intermedia presented with hematemesis. EGD showed large esophageal and Type 2 gastroesophageal varices. CT showed extensive chronic PVT with complete portal vein and portosplenic confluence occlusion with cavernous transformation. Workup was positive for JAK2 V617F, though not meeting full overt myeloproliferative neoplasm criteria. Anticoagulation was deferred due to high bleeding risk. Recanalization (TIPS, thrombectomy) was infeasible due to chronicity. Management involved supportive care and repeat endoscopic band ligation. She faces ongoing risks from severe portal hypertension.
A 38-year-old man presented with hematemesis. Seven years prior, an admission for bloody diarrhea revealed splenomegaly, esophageal varices, and thrombocytosis with a patent portal vein, but no definitive etiology was established, and he was lost to follow-up. Current imaging confirmed extensive chronic PVT with cavernous transformation and complete splenic vein occlusion. EGD showed esophageal/gastric varices with an ulcer. Workup revealed extreme thrombocytosis from an underlying myeloproliferative neoplasm confirmed by bone marrow biopsy, with JAK2 V617F mutation. Similarly, chronicity precluded recanalization and anticoagulation was withheld due to bleeding risk. He continues to have severe portal hypertension.
Discussion: These cases of severe JAK2 V617F-associated PVT, diagnosed after massive hematemesis, faced severely limited therapies and profound complications. They underscore the critical need for earlier recognition and comprehensive hypercoagulability investigation in patients with unexplained early signs of portal hypertension, varices, splenomegaly, or hematologic abnormalities. Prompt identification of underlying prothrombotic states is paramount, allowing intervention before irreversible thrombosis and life-threatening hemorrhage develop, improving patient outcomes.

Figure: Case 1 CT of PVT, EGD image of EV
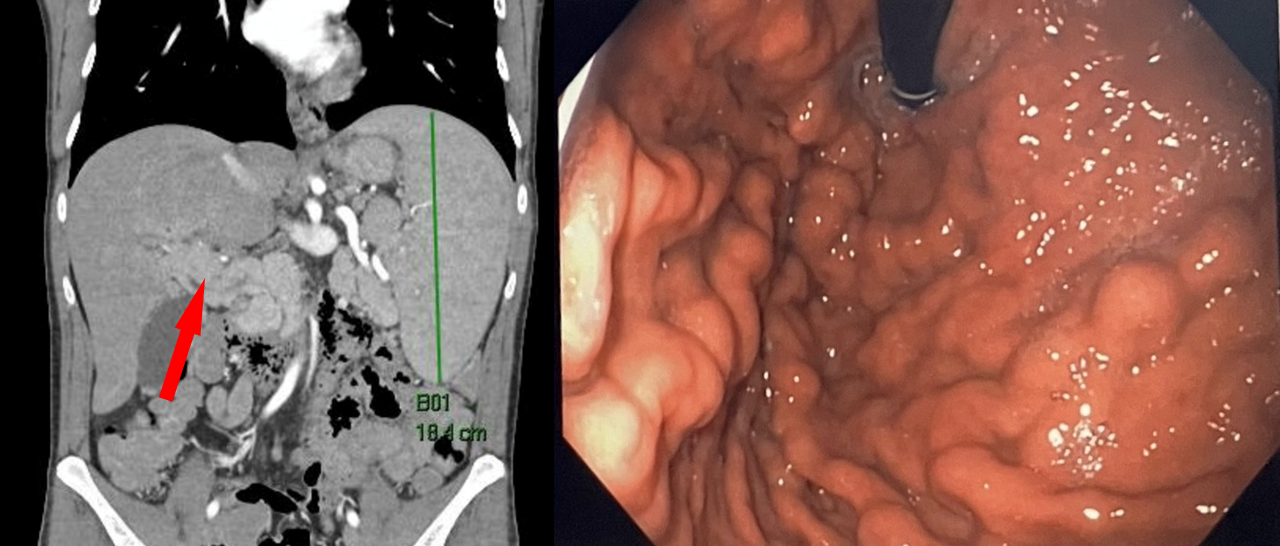
Figure: Case 2 CT of PVT, EGD image of Gastric Varices
Disclosures:
Justin Lin indicated no relevant financial relationships.
Michelle Shi indicated no relevant financial relationships.
Jang Kim indicated no relevant financial relationships.
Harmit Kalia indicated no relevant financial relationships.
Justin Lin, MD1, Michelle Shi, MD2, Jang Kim, MD2, Harmit Singh. Kalia, DO2. P4006 - Severe Portal Hypertension From Late-Diagnosed JAK2-Associated PVT: Time for a Paradigm Shift in Earlier Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
