Monday Poster Session
Category: Liver
P3984 - Hepatocellular Carcinoma in Non-Cirrhotic Liver: A Case Series
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LA
Leen Azeez, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Leen Azeez, MD1, Keerthi Thallapureddy, MD1, Katherine S.. Crow, MS, PA-C2, Daniel Wheeler, DO1, Lisa D. Pedicone, PhD3, Jan Petrasek, MD1, Fabian Rodas, MD1, Andres Gomez-Aldana, MD1, Carmen landaverde, MD1, Eric Lawitz, MD1, Fred Poordad, MD1, Eugenia Tsai, MD3
1University of Texas Health San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3Texas Liver Institute, Austin, TX
Introduction: Hepatocellular carcinoma (HCC) is the 6th leading cancer worldwide. Although cirrhosis is the most common risk factor for the development of HCC, up to 20% of HCC occurs in non-cirrhotic liver. Non-cirrhotic HCC has a bimodal age distribution with peaks in the 2nd and 7th decades of life and is often diagnosed at more advanced stages due to the lack of surveillance and absence of symptoms. In this subgroup, HCC is associated with non-alcoholic fatty liver disease (NAFLD). We present characteristics associated with non-cirrhotic HCC in this case series.
Case Description/
Methods: We retrospectively analyzed patients referred to a multidisciplinary liver tumor center between January 2020 and December 2023. Patients with biochemical or radiographic evidence of, or biopsy-confirmed cirrhosis were excluded. All patients underwent a detailed serologic workup to evaluate for liver disease etiology including autoimmune, viral, genetic and metabolic causes. Magnetic resonance imaging (MRI) was utilized to characterize liver masses and liver biopsy was performed to confirm HCC.
A total of 6 patients (60% male) had noncirrhotic HCC. The median age at diagnosis was 72.5 [52-83] years and median body mass index (BMI) was 27 [24-32] kg/m2. Median AST and ALT were 55 [18-91] U/L and 45 [29-244] U/L, respectively. Etiologies of liver disease were metabolic dysfunction associated steatohepatitis (MASLD; formerly NAFLD) (n=1), hepatitis C virus infection (n=1), alcohol (n=1) and cryptogenic (n=3). Median tumor size measured on MRI and alpha-fetoprotein (AFP) levels were 10.4 [6.1-13] cm and 9.5 [3-189] ng/mL, respectively. Liver biopsy confirmed non-cirrhotic liver (n=5) and HCC. Figure 1 demonstrates liver mass on MRI with biopsy-confirmed HCC. All patients had advanced stage HCC (outside of Milan criteria) and were treated with liver resection (n=3), stereotactic body radiotherapy (n=1) or immunotherapy (n=2). Demographics and key characteristics are listed in table 1.
Discussion: This case series confirms the older age distribution and male sex association with HCC in non-cirrhotic liver. Risk factors such as smoking, diabetes mellitus and alcohol use were not ubiquitous amongst our cohort, highlighting the complex nature of non-cirrhotic HCC. Unfortunately, non-cirrhotic HCC lacks clear risk factors and screening biomarkers to identify subgroups that would benefit from screening. Interestingly, most patients had active liver injury which warrants further study into the role of inflammation in tumorigenesis.
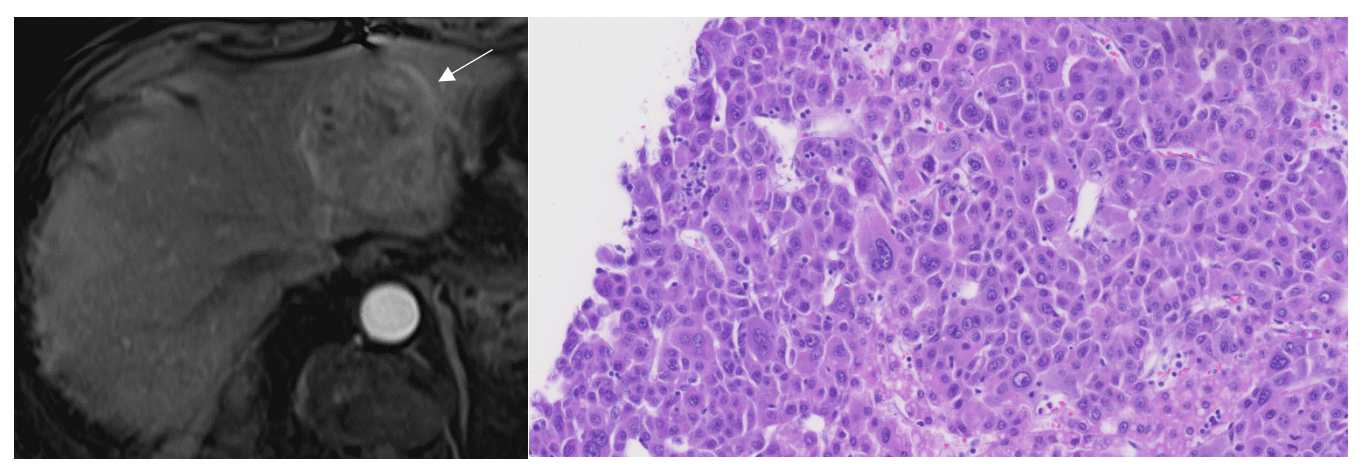
Figure: Liver mass of Patient 2 (a) MRI on T1 early arterial phase demonstrates a well-circumscribed 7 cm left hepatic lobe mass (white arrow) concerning for HCC subsequently biopsied and (b) histology demonstrates poorly differentiated HCC with marked nuclear pleimorphism and giant cells (H&E stain, 20x).
Disclosures:
Leen Azeez indicated no relevant financial relationships.
Keerthi Thallapureddy indicated no relevant financial relationships.
Katherine Crow: Circulogene Theranostics – Consultant, Speakers Bureau.
Daniel Wheeler indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Carmen landaverde indicated no relevant financial relationships.
Eric Lawitz indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Leen Azeez, MD1, Keerthi Thallapureddy, MD1, Katherine S.. Crow, MS, PA-C2, Daniel Wheeler, DO1, Lisa D. Pedicone, PhD3, Jan Petrasek, MD1, Fabian Rodas, MD1, Andres Gomez-Aldana, MD1, Carmen landaverde, MD1, Eric Lawitz, MD1, Fred Poordad, MD1, Eugenia Tsai, MD3. P3984 - Hepatocellular Carcinoma in Non-Cirrhotic Liver: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3Texas Liver Institute, Austin, TX
Introduction: Hepatocellular carcinoma (HCC) is the 6th leading cancer worldwide. Although cirrhosis is the most common risk factor for the development of HCC, up to 20% of HCC occurs in non-cirrhotic liver. Non-cirrhotic HCC has a bimodal age distribution with peaks in the 2nd and 7th decades of life and is often diagnosed at more advanced stages due to the lack of surveillance and absence of symptoms. In this subgroup, HCC is associated with non-alcoholic fatty liver disease (NAFLD). We present characteristics associated with non-cirrhotic HCC in this case series.
Case Description/
Methods: We retrospectively analyzed patients referred to a multidisciplinary liver tumor center between January 2020 and December 2023. Patients with biochemical or radiographic evidence of, or biopsy-confirmed cirrhosis were excluded. All patients underwent a detailed serologic workup to evaluate for liver disease etiology including autoimmune, viral, genetic and metabolic causes. Magnetic resonance imaging (MRI) was utilized to characterize liver masses and liver biopsy was performed to confirm HCC.
A total of 6 patients (60% male) had noncirrhotic HCC. The median age at diagnosis was 72.5 [52-83] years and median body mass index (BMI) was 27 [24-32] kg/m2. Median AST and ALT were 55 [18-91] U/L and 45 [29-244] U/L, respectively. Etiologies of liver disease were metabolic dysfunction associated steatohepatitis (MASLD; formerly NAFLD) (n=1), hepatitis C virus infection (n=1), alcohol (n=1) and cryptogenic (n=3). Median tumor size measured on MRI and alpha-fetoprotein (AFP) levels were 10.4 [6.1-13] cm and 9.5 [3-189] ng/mL, respectively. Liver biopsy confirmed non-cirrhotic liver (n=5) and HCC. Figure 1 demonstrates liver mass on MRI with biopsy-confirmed HCC. All patients had advanced stage HCC (outside of Milan criteria) and were treated with liver resection (n=3), stereotactic body radiotherapy (n=1) or immunotherapy (n=2). Demographics and key characteristics are listed in table 1.
Discussion: This case series confirms the older age distribution and male sex association with HCC in non-cirrhotic liver. Risk factors such as smoking, diabetes mellitus and alcohol use were not ubiquitous amongst our cohort, highlighting the complex nature of non-cirrhotic HCC. Unfortunately, non-cirrhotic HCC lacks clear risk factors and screening biomarkers to identify subgroups that would benefit from screening. Interestingly, most patients had active liver injury which warrants further study into the role of inflammation in tumorigenesis.
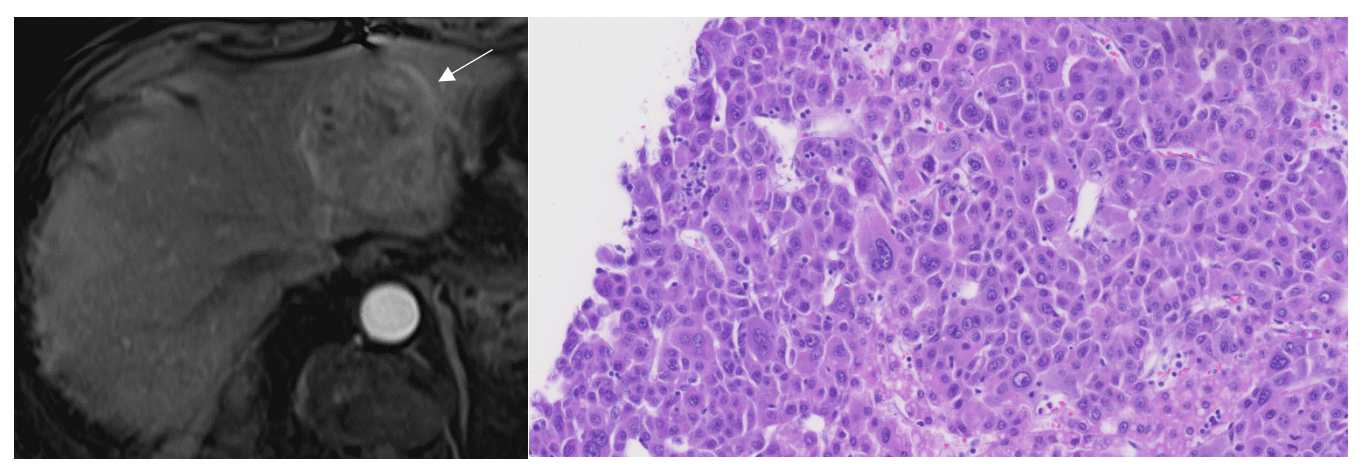
Figure: Liver mass of Patient 2 (a) MRI on T1 early arterial phase demonstrates a well-circumscribed 7 cm left hepatic lobe mass (white arrow) concerning for HCC subsequently biopsied and (b) histology demonstrates poorly differentiated HCC with marked nuclear pleimorphism and giant cells (H&E stain, 20x).
Disclosures:
Leen Azeez indicated no relevant financial relationships.
Keerthi Thallapureddy indicated no relevant financial relationships.
Katherine Crow: Circulogene Theranostics – Consultant, Speakers Bureau.
Daniel Wheeler indicated no relevant financial relationships.
Lisa D. Pedicone indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Andres Gomez-Aldana indicated no relevant financial relationships.
Carmen landaverde indicated no relevant financial relationships.
Eric Lawitz indicated no relevant financial relationships.
Fred Poordad indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Leen Azeez, MD1, Keerthi Thallapureddy, MD1, Katherine S.. Crow, MS, PA-C2, Daniel Wheeler, DO1, Lisa D. Pedicone, PhD3, Jan Petrasek, MD1, Fabian Rodas, MD1, Andres Gomez-Aldana, MD1, Carmen landaverde, MD1, Eric Lawitz, MD1, Fred Poordad, MD1, Eugenia Tsai, MD3. P3984 - Hepatocellular Carcinoma in Non-Cirrhotic Liver: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
