Monday Poster Session
Category: Liver
P3982 - Collateral Damage: Recurrent Splenorenal Shunt Leading to Hepatic Encephalopathy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Thomas G. Wichman, MD (he/him/his)
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Thomas G. Wichman, MD, Ismail Ganim, MD, Laura Smart, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Spontaneous portosystemic shunts (SPSS) may develop in cirrhotic patients due to longstanding portal hypertension, and they are associated with more severe liver dysfunction and decompensating events. Reversal of blood flow away from the liver can result in hyperammonemia and contribute to the development of hepatic encephalopathy, even in a non-diseased liver. It has been shown that up to 57.6% of patients with cirrhosis can have SPSS, small or large, with splenorenal shunts being the most common at roughly 27%. If the SPSS is large enough, patients may get relief from embolization. This case report encourages providers to consider the presence of SPSS in liver transplant patients who present with refractory hepatic encephalopathy (HE) despite both adequate medical management and prior shunt embolization.
Case Description/
Methods: We present the case of a 58-year-old female with history of alcoholic cirrhosis, for which she had an orthotopic liver transplant in 2019, and which was complicated by a large splenorenal shunt that was embolized in 2022. She presented with 5 days of altered mental status and constipation. Exam was significant for disorientation and asterixis. Labs showed mildly elevated AST/ALT at 58/31, respectively, phosphatidylethanol level of 11 ng/mL, and therapeutic levels of tacrolimus and everolimus. Right upper quadrant ultrasound with dopplers showed reversal of flow through the main portal vein, and triple-phase computed tomography (CT) of the abdomen showed interval development of multiple small-caliber splenorenal and gastrorenal collateral vessels. Following evaluation by interventional radiology, it was determined these collaterals would be too small for embolization, so she was managed medically with rifaximin and lactulose.
Discussion: A decompensating event like HE in a patient with history of cirrhosis who is status-post orthotopic liver transplant can be particularly worrisome for the patient and provider. Of note, due to a similar presentation in 2024, our patient underwent liver biopsy which ruled o ut rejection and fibrosis. While providers must rule out transplant rejection or interval development of cirrhosis or damage to a transplanted liver, it is important to consider vascular anomalies that could contribute to the patient’s presentation, and to obtain imaging as seen fit. In this case, though the patient had known SPSS, she previously was able to wean off lactulose but required it again in her outpatient course.
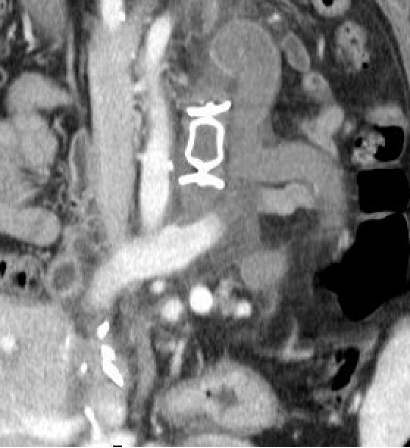
Figure: Successful thrombosis of the left large splenorenal shunt following embolization, as demonstrated on CT of the abdomen and pelvis in 2022.

Figure: Interval development of several small splenorenal collaterals at the time of patient’s presentation in 2025.
Disclosures:
Thomas Wichman indicated no relevant financial relationships.
Ismail Ganim indicated no relevant financial relationships.
Laura Smart indicated no relevant financial relationships.
Thomas G. Wichman, MD, Ismail Ganim, MD, Laura Smart, MD. P3982 - Collateral Damage: Recurrent Splenorenal Shunt Leading to Hepatic Encephalopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Spontaneous portosystemic shunts (SPSS) may develop in cirrhotic patients due to longstanding portal hypertension, and they are associated with more severe liver dysfunction and decompensating events. Reversal of blood flow away from the liver can result in hyperammonemia and contribute to the development of hepatic encephalopathy, even in a non-diseased liver. It has been shown that up to 57.6% of patients with cirrhosis can have SPSS, small or large, with splenorenal shunts being the most common at roughly 27%. If the SPSS is large enough, patients may get relief from embolization. This case report encourages providers to consider the presence of SPSS in liver transplant patients who present with refractory hepatic encephalopathy (HE) despite both adequate medical management and prior shunt embolization.
Case Description/
Methods: We present the case of a 58-year-old female with history of alcoholic cirrhosis, for which she had an orthotopic liver transplant in 2019, and which was complicated by a large splenorenal shunt that was embolized in 2022. She presented with 5 days of altered mental status and constipation. Exam was significant for disorientation and asterixis. Labs showed mildly elevated AST/ALT at 58/31, respectively, phosphatidylethanol level of 11 ng/mL, and therapeutic levels of tacrolimus and everolimus. Right upper quadrant ultrasound with dopplers showed reversal of flow through the main portal vein, and triple-phase computed tomography (CT) of the abdomen showed interval development of multiple small-caliber splenorenal and gastrorenal collateral vessels. Following evaluation by interventional radiology, it was determined these collaterals would be too small for embolization, so she was managed medically with rifaximin and lactulose.
Discussion: A decompensating event like HE in a patient with history of cirrhosis who is status-post orthotopic liver transplant can be particularly worrisome for the patient and provider. Of note, due to a similar presentation in 2024, our patient underwent liver biopsy which ruled o ut rejection and fibrosis. While providers must rule out transplant rejection or interval development of cirrhosis or damage to a transplanted liver, it is important to consider vascular anomalies that could contribute to the patient’s presentation, and to obtain imaging as seen fit. In this case, though the patient had known SPSS, she previously was able to wean off lactulose but required it again in her outpatient course.
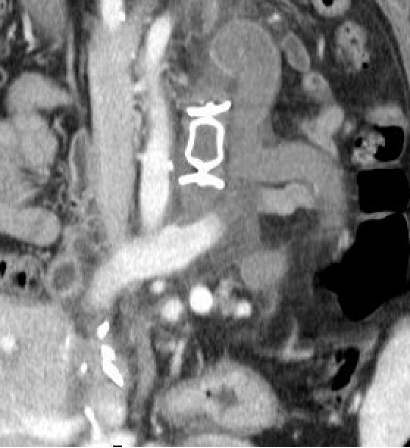
Figure: Successful thrombosis of the left large splenorenal shunt following embolization, as demonstrated on CT of the abdomen and pelvis in 2022.

Figure: Interval development of several small splenorenal collaterals at the time of patient’s presentation in 2025.
Disclosures:
Thomas Wichman indicated no relevant financial relationships.
Ismail Ganim indicated no relevant financial relationships.
Laura Smart indicated no relevant financial relationships.
Thomas G. Wichman, MD, Ismail Ganim, MD, Laura Smart, MD. P3982 - Collateral Damage: Recurrent Splenorenal Shunt Leading to Hepatic Encephalopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
