Monday Poster Session
Category: Liver
P3975 - When Newly Diagnosed Cirrhosis Conceals Cancer: Diagnosing CLL in a Patient With Alcohol Use Disorder, Lymphocytic Ascites, and Exudative Pleural Effusions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LC
Lixamar Colon Vicenti, MD, MSNS (she/her/hers)
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Lixamar Colon Vicenti, MD, MSNS1, Krystal Cruz Escobar, DO2, Leyla Bojanini, MD3
1University of Texas Health Science Center, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3University of North Texas Health Science Center, San Antonio, TX
Introduction: In cirrhosis, ascitic fluid is usually transudative and sterile, with low PMN counts. Spontaneous bacterial peritonitis (SBP) is defined by PMN >250 cells/mm³, while lymphocyte-predominant ascites is rare and suggests alternative diagnoses. We present a case of decompensated presumed alcoholic cirrhosis with lymphocyte-rich ascites and pleural effusion, ultimately attributed to chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
Case Description/
Methods: A 64-year-old man with newly diagnosed cirrhosis, likely alcohol-related, presented with progressive leg swelling and abdominal pain. He reported prior paracentesis in Mexico and had no outpatient follow-up.
During admission, he developed worsening ascites and a right pleural effusion, requiring serial drainage. Both fluids revealed 98% lymphocytes, prompting further evaluation.
CT imaging showed diffuse lymphadenopathy and splenomegaly (14 cm). Peripheral smear revealed reactive lymphocytes, and lymph node biopsy confirmed Rai stage IV CLL/SLL.
Given his decompensated cirrhosis, which precluded standard CLL induction regimens, and concurrent AKI with hyperuricemia concerning for spontaneous tumor lysis, he was started on weekly rituximab monotherapy for disease debulking, along with allopurinol and rasburicase. His course was complicated by pancytopenia, AKI, and metabolic acidosis, all managed appropriately. He improved and was discharged with hematology and hepatology follow-up.
Discussion: SBP typically presents with neutrophilic ascites. Lymphocyte-predominant fluid should raise concern for malignancy or tuberculosis. This case highlights the importance of fluid differential counts in diagnosis.
Cirrhosis can obscure conditions like CLL/SLL due to overlapping features—ascites, splenomegaly, and cytopenias—delaying diagnosis and complicating management. Hepatic dysfunction increases infection risk, limits treatment options, and is associated with poorer outcomes in hematologic malignancies.
Given the poor prognosis of decompensated cirrhosis—especially in the presence of ascites or encephalopathy—timely recognition of dual pathology is essential. When ascitic fluid profiles deviate from expected norms, clinicians should broaden their diagnostic approach to include flow cytometry, immunophenotyping, and advanced imaging to guide appropriate therapy.
Portions of this case report were edited with the assistance of AI-based language tools.
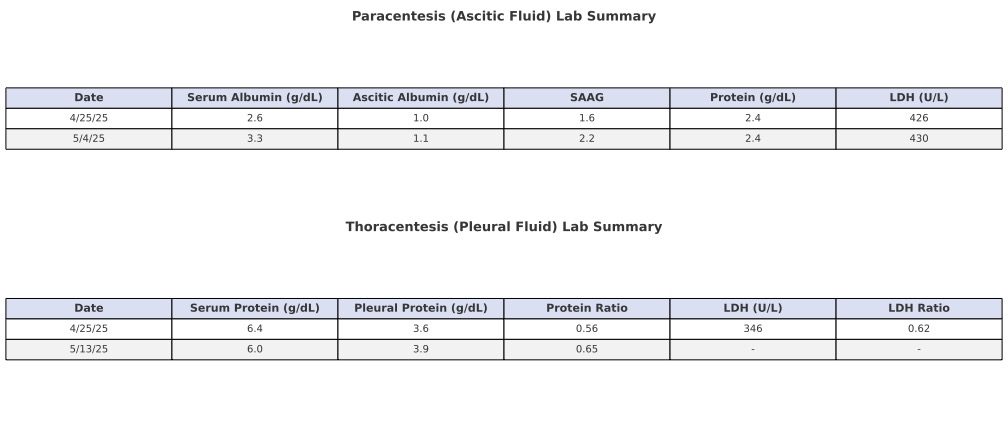
Figure: Table 1. Summary of paracentesis and thoracentesis laboratory findings.
Paracentesis demonstrated serum-ascites albumin gradient (SAAG) values >1.1 on both dates, consistent with portal hypertension. Ascitic protein levels were low, supporting a transudative process.
Thoracentesis on 4/25 met all of Light’s criteria for an exudative effusion, with pleural/serum protein and LDH ratios >0.5 and >0.6, respectively, and elevated pleural LDH. Findings are consistent with malignant pleural involvement in the setting of CLL/SLL.
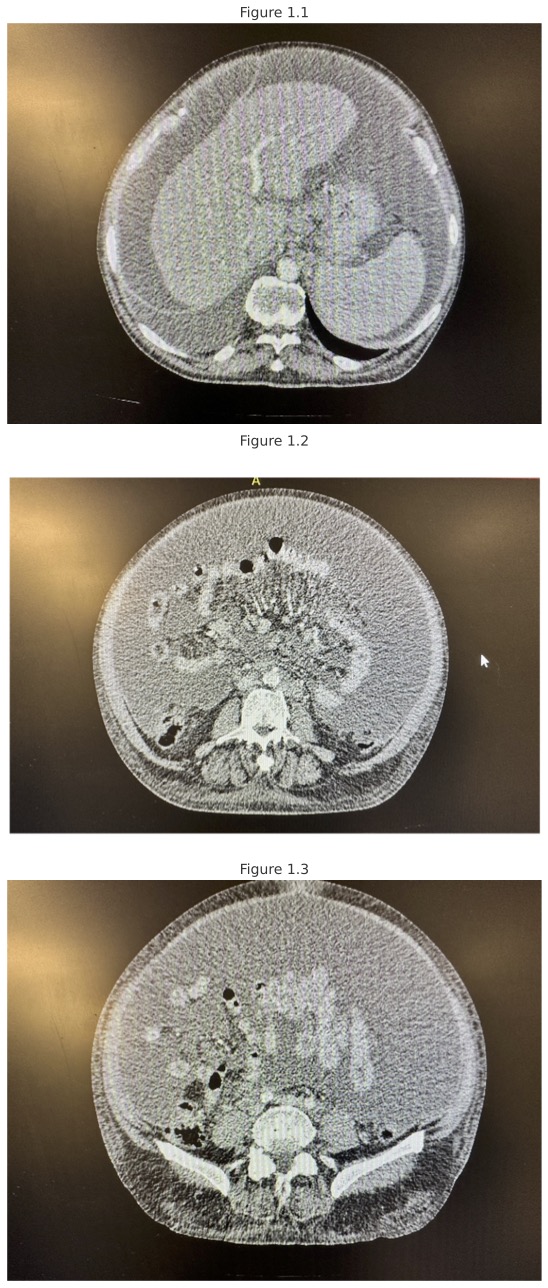
Figure: Figure 1.1–1.3.
CT Abdomen and Pelvis with IV contrast demonstrating cirrhosis with sequelae of portal hypertension, including splenomegaly and marked ascites. Mild diffuse peritoneal enhancement raises concern for spontaneous bacterial peritonitis.
Prominent paraesophageal, mesenteric, retroperitoneal, bilateral pelvic sidewall, and inguinal lymphadenopathy. Additional findings include mild omental stranding concerning for a neoplastic process, diffuse soft tissue anasarca, and a moderate right-sided pleural effusion with associated passive lung collapse.
Disclosures:
Lixamar Colon Vicenti indicated no relevant financial relationships.
Krystal Cruz Escobar indicated no relevant financial relationships.
Leyla Bojanini indicated no relevant financial relationships.
Lixamar Colon Vicenti, MD, MSNS1, Krystal Cruz Escobar, DO2, Leyla Bojanini, MD3. P3975 - When Newly Diagnosed Cirrhosis Conceals Cancer: Diagnosing CLL in a Patient With Alcohol Use Disorder, Lymphocytic Ascites, and Exudative Pleural Effusions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health Science Center, San Antonio, TX; 2University of Texas Health San Antonio, San Antonio, TX; 3University of North Texas Health Science Center, San Antonio, TX
Introduction: In cirrhosis, ascitic fluid is usually transudative and sterile, with low PMN counts. Spontaneous bacterial peritonitis (SBP) is defined by PMN >250 cells/mm³, while lymphocyte-predominant ascites is rare and suggests alternative diagnoses. We present a case of decompensated presumed alcoholic cirrhosis with lymphocyte-rich ascites and pleural effusion, ultimately attributed to chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL).
Case Description/
Methods: A 64-year-old man with newly diagnosed cirrhosis, likely alcohol-related, presented with progressive leg swelling and abdominal pain. He reported prior paracentesis in Mexico and had no outpatient follow-up.
During admission, he developed worsening ascites and a right pleural effusion, requiring serial drainage. Both fluids revealed 98% lymphocytes, prompting further evaluation.
CT imaging showed diffuse lymphadenopathy and splenomegaly (14 cm). Peripheral smear revealed reactive lymphocytes, and lymph node biopsy confirmed Rai stage IV CLL/SLL.
Given his decompensated cirrhosis, which precluded standard CLL induction regimens, and concurrent AKI with hyperuricemia concerning for spontaneous tumor lysis, he was started on weekly rituximab monotherapy for disease debulking, along with allopurinol and rasburicase. His course was complicated by pancytopenia, AKI, and metabolic acidosis, all managed appropriately. He improved and was discharged with hematology and hepatology follow-up.
Discussion: SBP typically presents with neutrophilic ascites. Lymphocyte-predominant fluid should raise concern for malignancy or tuberculosis. This case highlights the importance of fluid differential counts in diagnosis.
Cirrhosis can obscure conditions like CLL/SLL due to overlapping features—ascites, splenomegaly, and cytopenias—delaying diagnosis and complicating management. Hepatic dysfunction increases infection risk, limits treatment options, and is associated with poorer outcomes in hematologic malignancies.
Given the poor prognosis of decompensated cirrhosis—especially in the presence of ascites or encephalopathy—timely recognition of dual pathology is essential. When ascitic fluid profiles deviate from expected norms, clinicians should broaden their diagnostic approach to include flow cytometry, immunophenotyping, and advanced imaging to guide appropriate therapy.
Portions of this case report were edited with the assistance of AI-based language tools.
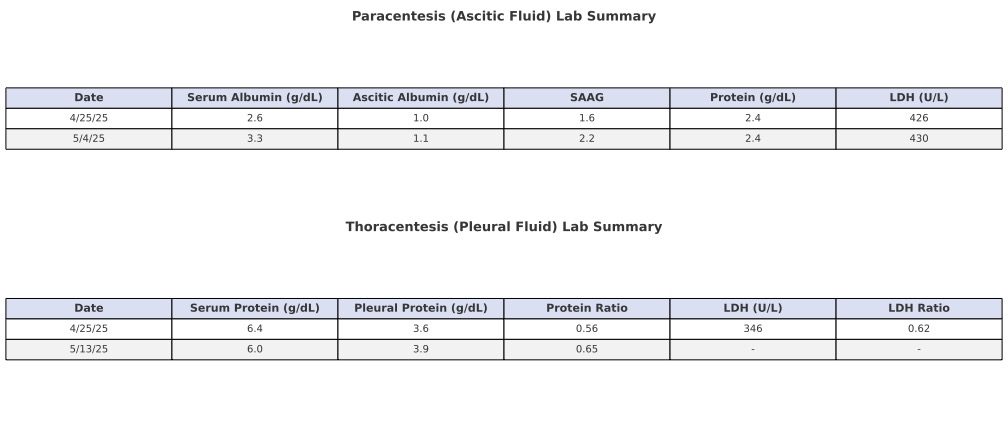
Figure: Table 1. Summary of paracentesis and thoracentesis laboratory findings.
Paracentesis demonstrated serum-ascites albumin gradient (SAAG) values >1.1 on both dates, consistent with portal hypertension. Ascitic protein levels were low, supporting a transudative process.
Thoracentesis on 4/25 met all of Light’s criteria for an exudative effusion, with pleural/serum protein and LDH ratios >0.5 and >0.6, respectively, and elevated pleural LDH. Findings are consistent with malignant pleural involvement in the setting of CLL/SLL.
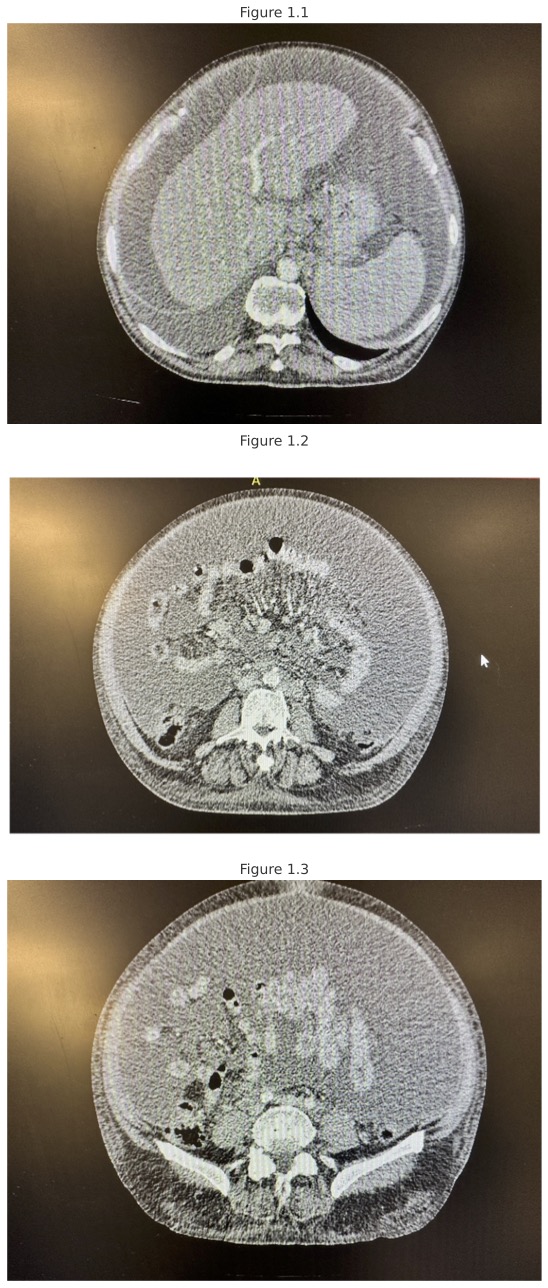
Figure: Figure 1.1–1.3.
CT Abdomen and Pelvis with IV contrast demonstrating cirrhosis with sequelae of portal hypertension, including splenomegaly and marked ascites. Mild diffuse peritoneal enhancement raises concern for spontaneous bacterial peritonitis.
Prominent paraesophageal, mesenteric, retroperitoneal, bilateral pelvic sidewall, and inguinal lymphadenopathy. Additional findings include mild omental stranding concerning for a neoplastic process, diffuse soft tissue anasarca, and a moderate right-sided pleural effusion with associated passive lung collapse.
Disclosures:
Lixamar Colon Vicenti indicated no relevant financial relationships.
Krystal Cruz Escobar indicated no relevant financial relationships.
Leyla Bojanini indicated no relevant financial relationships.
Lixamar Colon Vicenti, MD, MSNS1, Krystal Cruz Escobar, DO2, Leyla Bojanini, MD3. P3975 - When Newly Diagnosed Cirrhosis Conceals Cancer: Diagnosing CLL in a Patient With Alcohol Use Disorder, Lymphocytic Ascites, and Exudative Pleural Effusions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
