Monday Poster Session
Category: Liver
P3964 - BRIC or DILI: A Diagnostic Challenge
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TK
Taofeek Kolade, MD, MBA, MPH (he/him/his)
Bayonne Medical Center
Bayonne, NJ
Presenting Author(s)
Taofeek Kolade, MD, MBA, MPH1, Philip Hall, MD, MPH2, Adwait Patel, MD1, Ricardo Binsol, MD3, Meron Debesai, MD4
1Bayonne Medical Center, Bayonne, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ; 3Bayonne Medical Center, Byaonne, NJ; 4Carepoint Health/ Christ Hospital, Jersey City, NJ
Introduction: Benign recurrent intrahepatic cholestasis (BRIC) is a rare autosomal recessive disorder marked by episodic jaundice and pruritus without progression to liver failure. It is associated with mutations in ATP8B1 (BRIC1) or ABCB11 (BRIC2), with triggers including infections, medications, or hormonal changes. Fewer than 50 cases have been reported in the U.S. Diagnostic overlap with other cholestatic liver diseases, particularly drug-induced liver injury (DILI), complicates recognition. The Luketic and Shiffman criteria offer a clinical framework, though not formally validated. We present a case of suspected BRIC with possible DILI, highlighting diagnostic challenges.
Case Description/
Methods: A 26-year-old male presented with one month of jaundice, dark urine, pale stools, nausea, and right upper quadrant pain. He had a flu-like illness two weeks prior and began pantoprazole one month before symptoms. He was unsure of any past jaundice. Family history included jaundice in his grandfather and unspecified cancer. Exam showed scleral icterus without hepatosplenomegaly. Labs revealed total bilirubin 10 mg/dL (peaking at 30.8), mildly elevated ALP, AST, ALT, normal GGT, hemoglobin 12.2 g/dL, and elevated ferritin. Workup for hereditary hemochromatosis, autoimmune, infectious, metabolic, and toxic causes was negative. Imaging (ultrasound, CT, MRCP) showed no obstruction or structural abnormalities. Cholestyramine provided partial symptom relief. He returned 2.5 weeks later with recurrent symptoms and weight loss. Ursodiol was started, with subsequent improvement. Liver biopsy showed lobular cholestasis, mild periportal inflammation, and focal bile duct proliferation; findings consistent with BRIC but not excluding DILI. Genetic testing was recommended.
Discussion: This case met clinical, biochemical, and histologic features of BRIC, likely triggered by a viral illness. However, pantoprazole use raised concern for DILI or a mixed etiology. Although BRIC typically presents with recurrent episodes, this may represent an initial manifestation, further complicating differentiation from idiopathic or drug-related cholestasis. Liver biopsy supported BRIC but was not definitive. Genetic testing for ATP8B1 and ABCB11 may confirm diagnosis, though not timely for acute decisions. This case highlights the importance of considering BRIC in patients with unexplained cholestasis, especially when drug exposure and viral illness are present. Early recognition can help avoid unnecessary interventions and guide management.
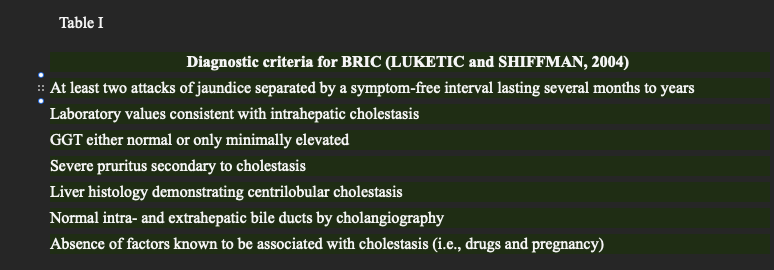
Figure: Figure 1. top ; periportal inflamation. Bottom: centrilobular cholestasis
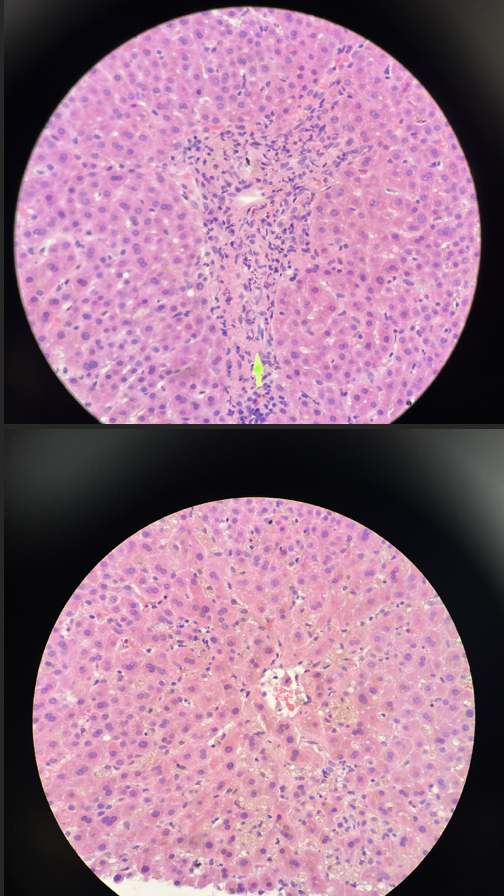
Figure: Table I. Diagnostic Criteria for Benign Reccurrent Cholestasis proprosed by Luketic and Shiffman. Obtained from Luketic VA, Shiffman ML. Benign recurrent intrahepatic cholestasis. Clinics in Liver Disease. 2003;7(1):153–164
Disclosures:
Taofeek Kolade indicated no relevant financial relationships.
Philip Hall indicated no relevant financial relationships.
Adwait Patel indicated no relevant financial relationships.
Ricardo Binsol indicated no relevant financial relationships.
Meron Debesai indicated no relevant financial relationships.
Taofeek Kolade, MD, MBA, MPH1, Philip Hall, MD, MPH2, Adwait Patel, MD1, Ricardo Binsol, MD3, Meron Debesai, MD4. P3964 - BRIC or DILI: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Bayonne Medical Center, Bayonne, NJ; 2CarePoint Health - Bayonne Medical Center, Bayonne, NJ; 3Bayonne Medical Center, Byaonne, NJ; 4Carepoint Health/ Christ Hospital, Jersey City, NJ
Introduction: Benign recurrent intrahepatic cholestasis (BRIC) is a rare autosomal recessive disorder marked by episodic jaundice and pruritus without progression to liver failure. It is associated with mutations in ATP8B1 (BRIC1) or ABCB11 (BRIC2), with triggers including infections, medications, or hormonal changes. Fewer than 50 cases have been reported in the U.S. Diagnostic overlap with other cholestatic liver diseases, particularly drug-induced liver injury (DILI), complicates recognition. The Luketic and Shiffman criteria offer a clinical framework, though not formally validated. We present a case of suspected BRIC with possible DILI, highlighting diagnostic challenges.
Case Description/
Methods: A 26-year-old male presented with one month of jaundice, dark urine, pale stools, nausea, and right upper quadrant pain. He had a flu-like illness two weeks prior and began pantoprazole one month before symptoms. He was unsure of any past jaundice. Family history included jaundice in his grandfather and unspecified cancer. Exam showed scleral icterus without hepatosplenomegaly. Labs revealed total bilirubin 10 mg/dL (peaking at 30.8), mildly elevated ALP, AST, ALT, normal GGT, hemoglobin 12.2 g/dL, and elevated ferritin. Workup for hereditary hemochromatosis, autoimmune, infectious, metabolic, and toxic causes was negative. Imaging (ultrasound, CT, MRCP) showed no obstruction or structural abnormalities. Cholestyramine provided partial symptom relief. He returned 2.5 weeks later with recurrent symptoms and weight loss. Ursodiol was started, with subsequent improvement. Liver biopsy showed lobular cholestasis, mild periportal inflammation, and focal bile duct proliferation; findings consistent with BRIC but not excluding DILI. Genetic testing was recommended.
Discussion: This case met clinical, biochemical, and histologic features of BRIC, likely triggered by a viral illness. However, pantoprazole use raised concern for DILI or a mixed etiology. Although BRIC typically presents with recurrent episodes, this may represent an initial manifestation, further complicating differentiation from idiopathic or drug-related cholestasis. Liver biopsy supported BRIC but was not definitive. Genetic testing for ATP8B1 and ABCB11 may confirm diagnosis, though not timely for acute decisions. This case highlights the importance of considering BRIC in patients with unexplained cholestasis, especially when drug exposure and viral illness are present. Early recognition can help avoid unnecessary interventions and guide management.
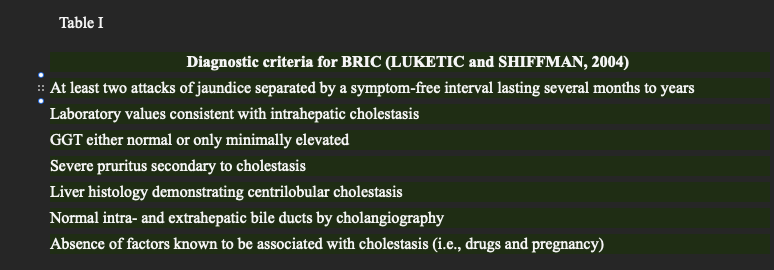
Figure: Figure 1. top ; periportal inflamation. Bottom: centrilobular cholestasis
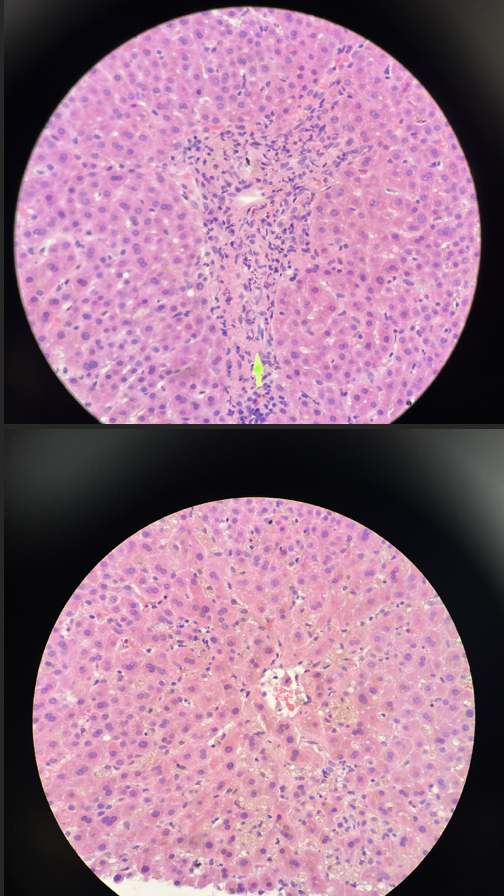
Figure: Table I. Diagnostic Criteria for Benign Reccurrent Cholestasis proprosed by Luketic and Shiffman. Obtained from Luketic VA, Shiffman ML. Benign recurrent intrahepatic cholestasis. Clinics in Liver Disease. 2003;7(1):153–164
Disclosures:
Taofeek Kolade indicated no relevant financial relationships.
Philip Hall indicated no relevant financial relationships.
Adwait Patel indicated no relevant financial relationships.
Ricardo Binsol indicated no relevant financial relationships.
Meron Debesai indicated no relevant financial relationships.
Taofeek Kolade, MD, MBA, MPH1, Philip Hall, MD, MPH2, Adwait Patel, MD1, Ricardo Binsol, MD3, Meron Debesai, MD4. P3964 - BRIC or DILI: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
