Monday Poster Session
Category: Liver
P3941 - A Case of Biopsy Proven Relapsing Hepatitis A Infection
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah O'Neill, MD (she/her/hers)
Houston Methodist-Weill Cornell Graduate School of Medical Sciences
Houston, TX
Presenting Author(s)
Hannah O'Neill, MD1, Shayan Amini, MD2, Tamneet Basra, MD3
1Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX; 2Houston Methodist Hospital, Houston, TX; 3Houston Methodist, Houston, TX
Introduction: Hepatitis A virus (HAV) is one of the most common causes of hepatitis in the world. It is highly endemic in developing areas with contaminated water implicated in outbreaks4. Common presentation in the US follows travel to an endemic area. Clinical presentation includes symptoms of acute hepatitis. Course is typically self-limited with clinical / biochemical resolution by six months. Fulminant liver failure is very rare (< 1% of cases) and associated with pre-existing liver disease / advanced age3. Relapsing HAV is atypical (10% of cases1,5). We present a biopsy-proven case of relapsing HAV.
Case Description/
Methods: 52-year-old male presented with abdominal discomfort following a recent trip to Mexico. Exam was unremarkable. Workup included aminotransferase elevation (2000s-3000s), hyperbilirubinemia (3.5) and marked hepatomegaly. HAV IgM was positive. MRCP for concurrent obstruction was negative. Autoimmune workup (antinuclear antibody & anti-smooth muscle) was negative. Patient endorsed alcohol consumption (10 drinks per week) & otherwise had no liver disease risk factors. Symptoms / liver tests improved. He did not go into acute liver failure & was discharged for outpatient monitoring.
Elevated liver tests continued to resolve at one month with aminotransferase improvement (100s-200s) and hyperbilirubinemia resolved. In spite of avoidance of alcohol / supplements, levels worsened at the two month mark, prompting further evaluation. Liver biopsy noted moderate lobular hepatitis, suspected secondary to relapsing HAV. Patient remained clinically asymptomatic, and he had remission six months out from his initial diagnosis.
Discussion: Although severity of HAV relapse is low, it is an important differential to consider for a patient with persistent / recurrent elevated liver tests. Relapse timeline is 2-3 months from initial presentation. Clinical course is typically mild and may be isolated to biochemical relapse. Multiple relapses are exceedingly rare2. Persistent viremia / HAV shedding are detectable during recurrence. If severe relapse is present (hyperbilirubinemia / pruritis), a short course of corticosteroids may be considered.
In our case, asymptomatic relapse occurred two months after initial. Recurrent aminotransferase elevation was milder. Case was managed conservatively. Our case highlights the importance of including relapsing HAV in a differential and utilizing biopsy as a diagnostic tool. It also highlights the importance of continued monitoring until full resolution is reached.
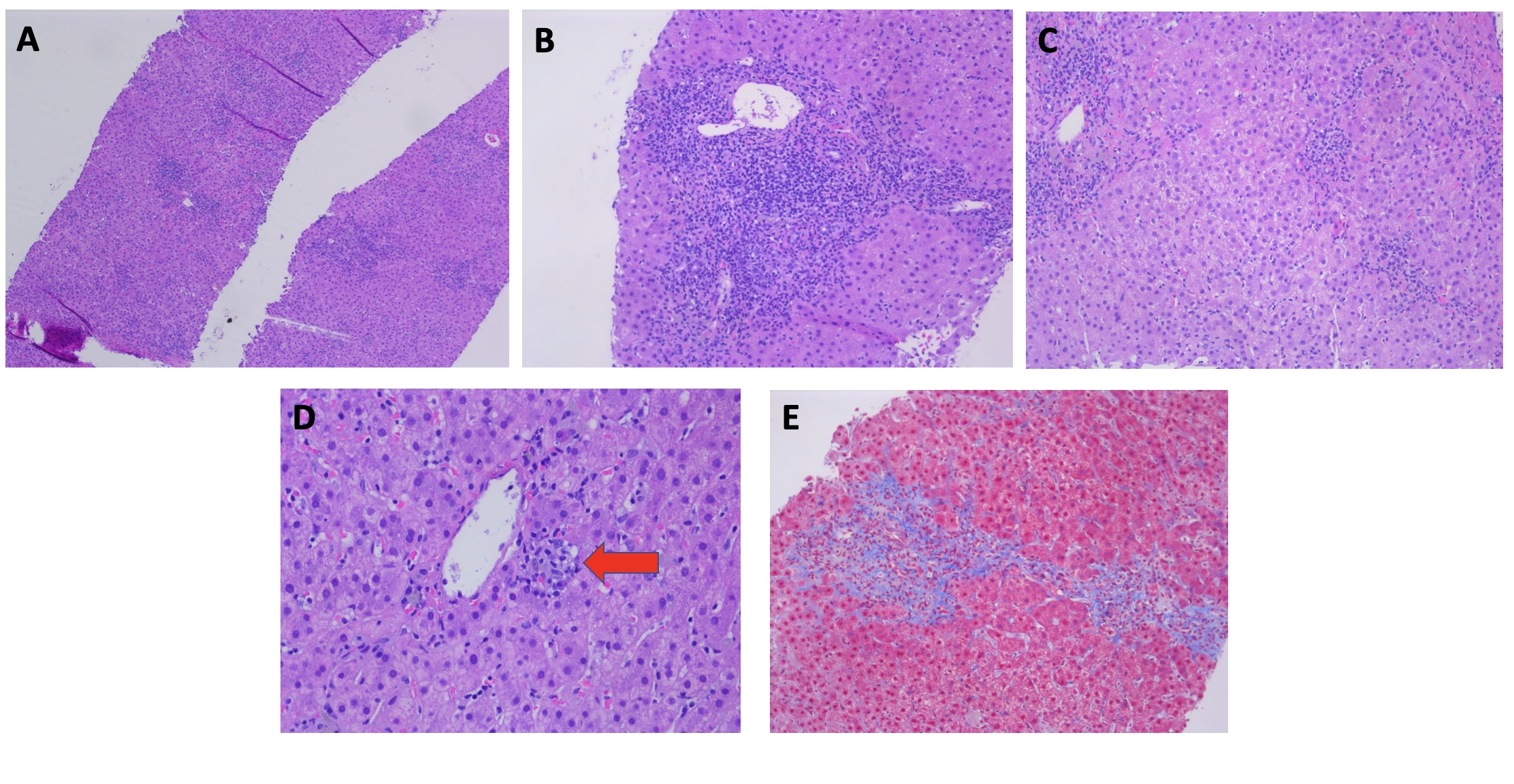
Figure: Figure 1: Liver Biopsy
A) Low-power view of liver biopsy demonstrating moderate active hepatitis with a chronic inflammatory infiltrate (H and E, x40)
B) Chronic portal lymphoplasmacytic inflammation with circumferential interface hepatitis (H and E, x100)
C) Moderate active portal and lobular hepatitis with ceroid laden-macrophages in the portal tract on the upper left (H and E, x100)
D) Small centrizonal lobular non-necrotizing granuloma (H and E x 200)
E) Masson trichrome staining demonstrating a single focus of bridging fibrosis (x 100)
Disclosures:
Hannah O'Neill indicated no relevant financial relationships.
Shayan Amini indicated no relevant financial relationships.
Tamneet Basra indicated no relevant financial relationships.
Hannah O'Neill, MD1, Shayan Amini, MD2, Tamneet Basra, MD3. P3941 - A Case of Biopsy Proven Relapsing Hepatitis A Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Houston Methodist-Weill Cornell Graduate School of Medical Sciences, Houston, TX; 2Houston Methodist Hospital, Houston, TX; 3Houston Methodist, Houston, TX
Introduction: Hepatitis A virus (HAV) is one of the most common causes of hepatitis in the world. It is highly endemic in developing areas with contaminated water implicated in outbreaks4. Common presentation in the US follows travel to an endemic area. Clinical presentation includes symptoms of acute hepatitis. Course is typically self-limited with clinical / biochemical resolution by six months. Fulminant liver failure is very rare (< 1% of cases) and associated with pre-existing liver disease / advanced age3. Relapsing HAV is atypical (10% of cases1,5). We present a biopsy-proven case of relapsing HAV.
Case Description/
Methods: 52-year-old male presented with abdominal discomfort following a recent trip to Mexico. Exam was unremarkable. Workup included aminotransferase elevation (2000s-3000s), hyperbilirubinemia (3.5) and marked hepatomegaly. HAV IgM was positive. MRCP for concurrent obstruction was negative. Autoimmune workup (antinuclear antibody & anti-smooth muscle) was negative. Patient endorsed alcohol consumption (10 drinks per week) & otherwise had no liver disease risk factors. Symptoms / liver tests improved. He did not go into acute liver failure & was discharged for outpatient monitoring.
Elevated liver tests continued to resolve at one month with aminotransferase improvement (100s-200s) and hyperbilirubinemia resolved. In spite of avoidance of alcohol / supplements, levels worsened at the two month mark, prompting further evaluation. Liver biopsy noted moderate lobular hepatitis, suspected secondary to relapsing HAV. Patient remained clinically asymptomatic, and he had remission six months out from his initial diagnosis.
Discussion: Although severity of HAV relapse is low, it is an important differential to consider for a patient with persistent / recurrent elevated liver tests. Relapse timeline is 2-3 months from initial presentation. Clinical course is typically mild and may be isolated to biochemical relapse. Multiple relapses are exceedingly rare2. Persistent viremia / HAV shedding are detectable during recurrence. If severe relapse is present (hyperbilirubinemia / pruritis), a short course of corticosteroids may be considered.
In our case, asymptomatic relapse occurred two months after initial. Recurrent aminotransferase elevation was milder. Case was managed conservatively. Our case highlights the importance of including relapsing HAV in a differential and utilizing biopsy as a diagnostic tool. It also highlights the importance of continued monitoring until full resolution is reached.
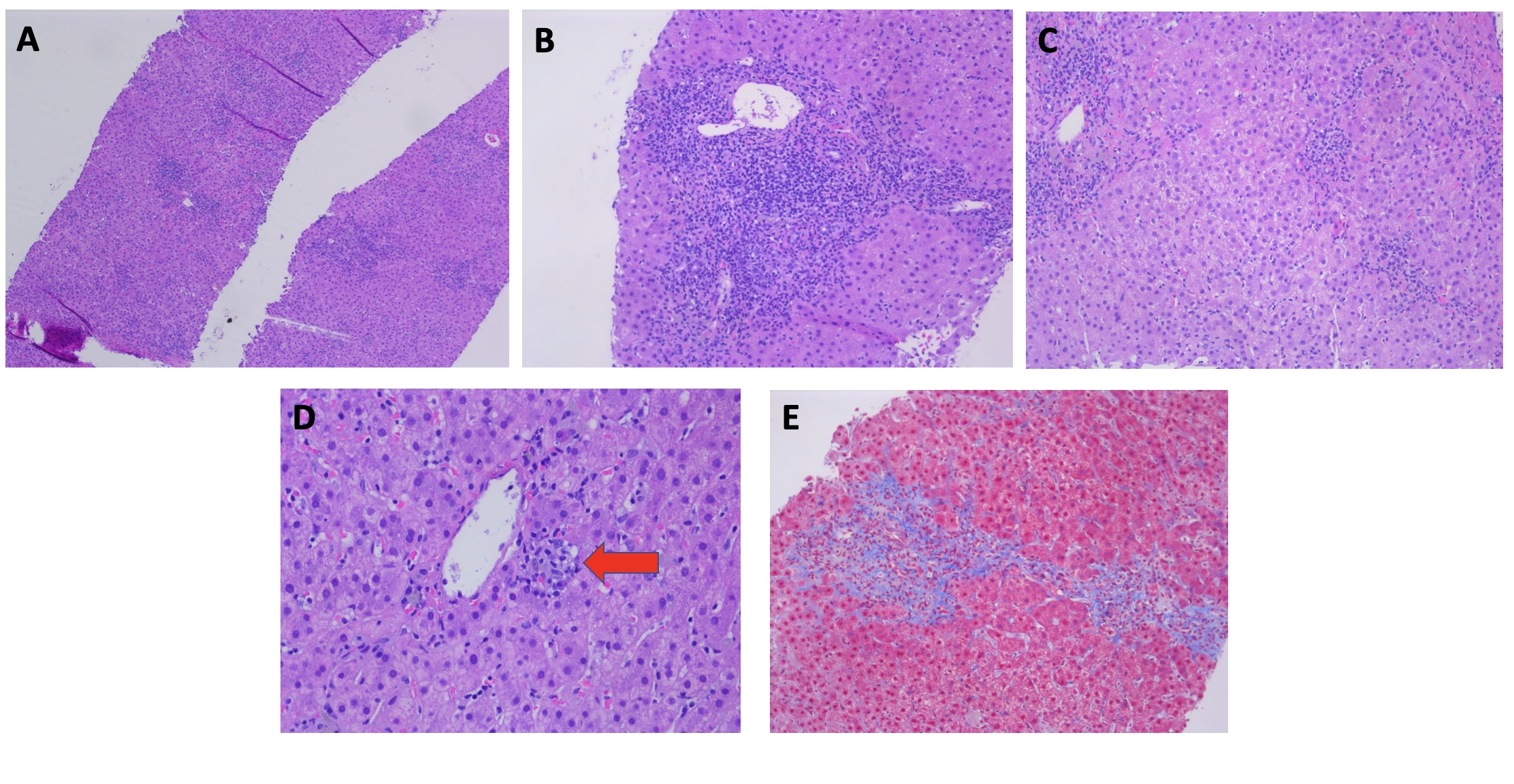
Figure: Figure 1: Liver Biopsy
A) Low-power view of liver biopsy demonstrating moderate active hepatitis with a chronic inflammatory infiltrate (H and E, x40)
B) Chronic portal lymphoplasmacytic inflammation with circumferential interface hepatitis (H and E, x100)
C) Moderate active portal and lobular hepatitis with ceroid laden-macrophages in the portal tract on the upper left (H and E, x100)
D) Small centrizonal lobular non-necrotizing granuloma (H and E x 200)
E) Masson trichrome staining demonstrating a single focus of bridging fibrosis (x 100)
Disclosures:
Hannah O'Neill indicated no relevant financial relationships.
Shayan Amini indicated no relevant financial relationships.
Tamneet Basra indicated no relevant financial relationships.
Hannah O'Neill, MD1, Shayan Amini, MD2, Tamneet Basra, MD3. P3941 - A Case of Biopsy Proven Relapsing Hepatitis A Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
