Monday Poster Session
Category: Liver
P3936 - Hepatic Hydrothorax in Dyskeratosis Congenita: A Rare Complication of Telomere Biology Disorder-Associated Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nouman Shafique, MD (he/him/his)
AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Nouman Shafique, MD1, Anurag Karki, MD2, Amna Malik, MD2, Sobaan Taj, MD2, Aimen Farooq, MD3, George Everett, MD2
1AdventHealth Orlando, Orlando, FL; 2AdventHealth, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Dyskeratosis congenita (DC) is a rare telomere biology disorder (TBD) characterized by mucocutaneous features, bone marrow (BM) failure, and multisystem organ involvement. Liver disease in DC, typically manifests as fibrosis, cirrhosis, or portal hypertension (PH). Hepatic hydrothorax (HH)—defined as transudative pleural effusion secondary to PH—is a rare decompensating event in cirrhotic patients and even more unusual in those with DC. We present a case of HH in a young adult with DC and decompensated cirrhosis.
Case Description/
Methods: A 21-year-old male with a history of DC (confirmed by telomere length testing), and liver cirrhosis secondary to telomere-related hepatic fibrosis presented with two weeks of progressive dyspnea and chest tightness. Imaging revealed a moderate right-sided pleural effusion (Figure 1). Given his underlying liver disease and PH, HH was suspected.
Thoracentesis yielded 1.5 L of straw-colored fluid, which was transudative by Light’s criteria (protein 0.7 g/dL, LDH 32 IU/L, glucose 105 mg/dL). Cultures and cytology were negative. Pulmonary evaluation ruled out primary parenchymal disease. The patient’s symptoms improved following drainage. He was managed with diuretics and sodium restriction.
His liver disease had previously been confirmed via imaging (Figure 2) and endoscopy, including small esophageal varices and portal hypertensive gastropathy. Transplant evaluation for simultaneous BM and liver transplant was ongoing. He remained stable at discharge.
Discussion: This case highlights HH as an under recognized complication of DC-related cirrhosis. TBD like DC are increasingly implicated in early-onset liver disease, particularly in patients with DKC1 and TINF2 mutations. Studies suggest liver involvement occurs in up to 40% of patients with telomere syndromes, with progression to PH and decompensation in about 17%. However, HH remains exceedingly rare.
Pathogenesis in DC is linked to impaired hepatocyte regeneration and vascular remodeling due to telomere dysfunction. As demonstrated in this patient, cirrhosis can develop in young adulthood with rapid decompensation. Recognition of HH is critical, as misdiagnosis may lead to inappropriate interventions. In patients with DC, early hepatology referral, routine screening for liver disease, and consideration for liver or dual-organ transplantation are essential. Outcomes following transplant, though limited, appear favorable
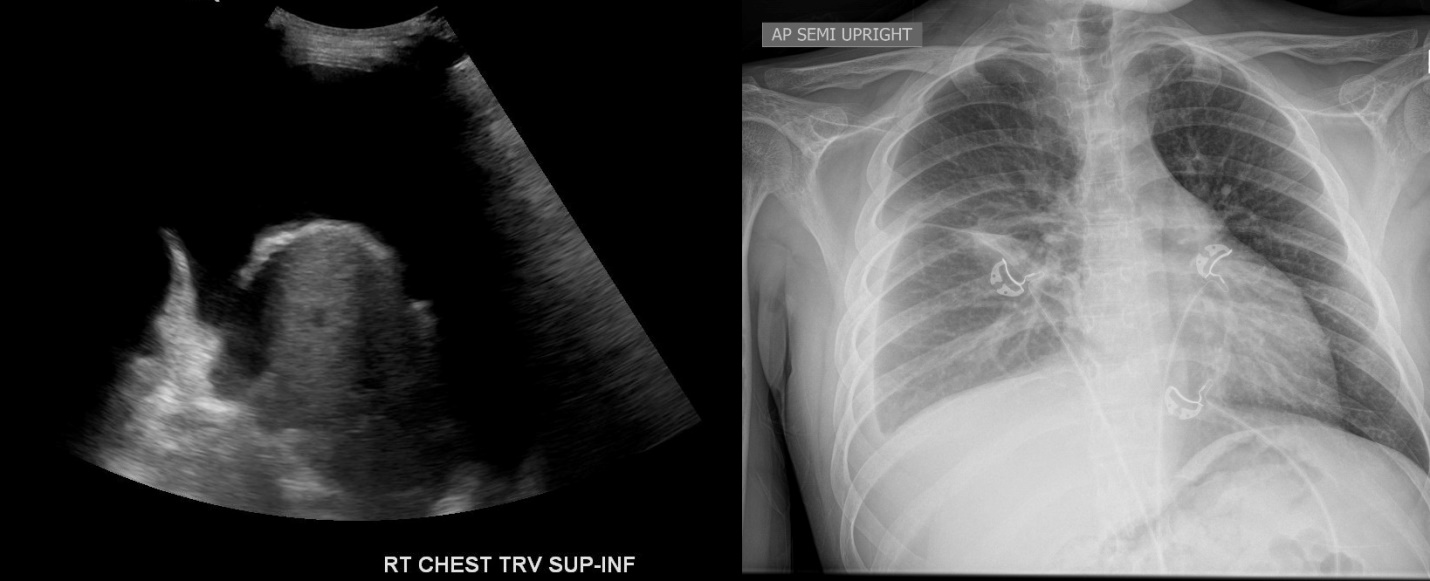
Figure: Figure 1: CXR and Ultrasound chest showing moderate right sided pleural effusion
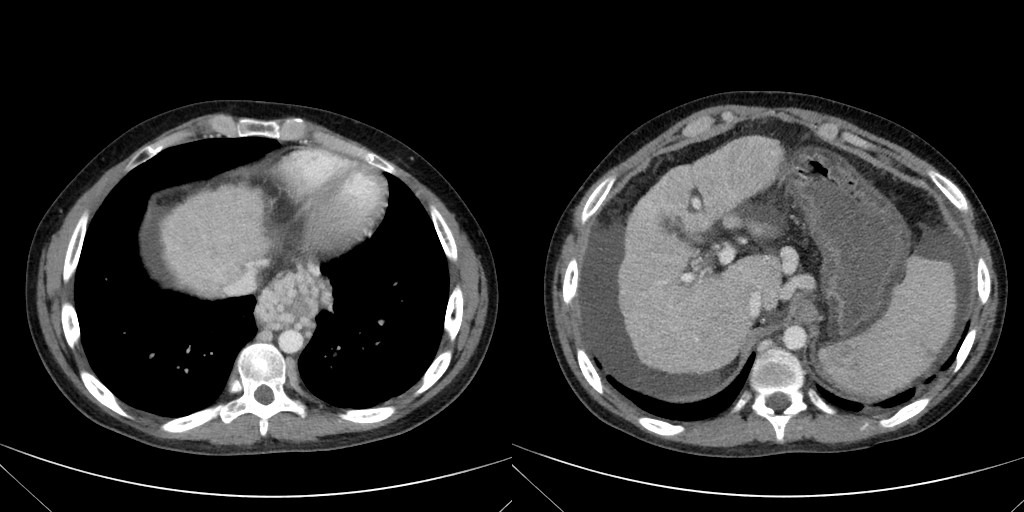
Figure: Figure 2: CT Abdomen and Pelvis showing cirrhotic liver morphology with numerous para-esophageal and gastric varices re-canalized umbilical vein
Disclosures:
Nouman Shafique indicated no relevant financial relationships.
Anurag Karki indicated no relevant financial relationships.
Amna Malik indicated no relevant financial relationships.
Sobaan Taj indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
George Everett indicated no relevant financial relationships.
Nouman Shafique, MD1, Anurag Karki, MD2, Amna Malik, MD2, Sobaan Taj, MD2, Aimen Farooq, MD3, George Everett, MD2. P3936 - Hepatic Hydrothorax in Dyskeratosis Congenita: A Rare Complication of Telomere Biology Disorder-Associated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1AdventHealth Orlando, Orlando, FL; 2AdventHealth, Orlando, FL; 3Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Dyskeratosis congenita (DC) is a rare telomere biology disorder (TBD) characterized by mucocutaneous features, bone marrow (BM) failure, and multisystem organ involvement. Liver disease in DC, typically manifests as fibrosis, cirrhosis, or portal hypertension (PH). Hepatic hydrothorax (HH)—defined as transudative pleural effusion secondary to PH—is a rare decompensating event in cirrhotic patients and even more unusual in those with DC. We present a case of HH in a young adult with DC and decompensated cirrhosis.
Case Description/
Methods: A 21-year-old male with a history of DC (confirmed by telomere length testing), and liver cirrhosis secondary to telomere-related hepatic fibrosis presented with two weeks of progressive dyspnea and chest tightness. Imaging revealed a moderate right-sided pleural effusion (Figure 1). Given his underlying liver disease and PH, HH was suspected.
Thoracentesis yielded 1.5 L of straw-colored fluid, which was transudative by Light’s criteria (protein 0.7 g/dL, LDH 32 IU/L, glucose 105 mg/dL). Cultures and cytology were negative. Pulmonary evaluation ruled out primary parenchymal disease. The patient’s symptoms improved following drainage. He was managed with diuretics and sodium restriction.
His liver disease had previously been confirmed via imaging (Figure 2) and endoscopy, including small esophageal varices and portal hypertensive gastropathy. Transplant evaluation for simultaneous BM and liver transplant was ongoing. He remained stable at discharge.
Discussion: This case highlights HH as an under recognized complication of DC-related cirrhosis. TBD like DC are increasingly implicated in early-onset liver disease, particularly in patients with DKC1 and TINF2 mutations. Studies suggest liver involvement occurs in up to 40% of patients with telomere syndromes, with progression to PH and decompensation in about 17%. However, HH remains exceedingly rare.
Pathogenesis in DC is linked to impaired hepatocyte regeneration and vascular remodeling due to telomere dysfunction. As demonstrated in this patient, cirrhosis can develop in young adulthood with rapid decompensation. Recognition of HH is critical, as misdiagnosis may lead to inappropriate interventions. In patients with DC, early hepatology referral, routine screening for liver disease, and consideration for liver or dual-organ transplantation are essential. Outcomes following transplant, though limited, appear favorable
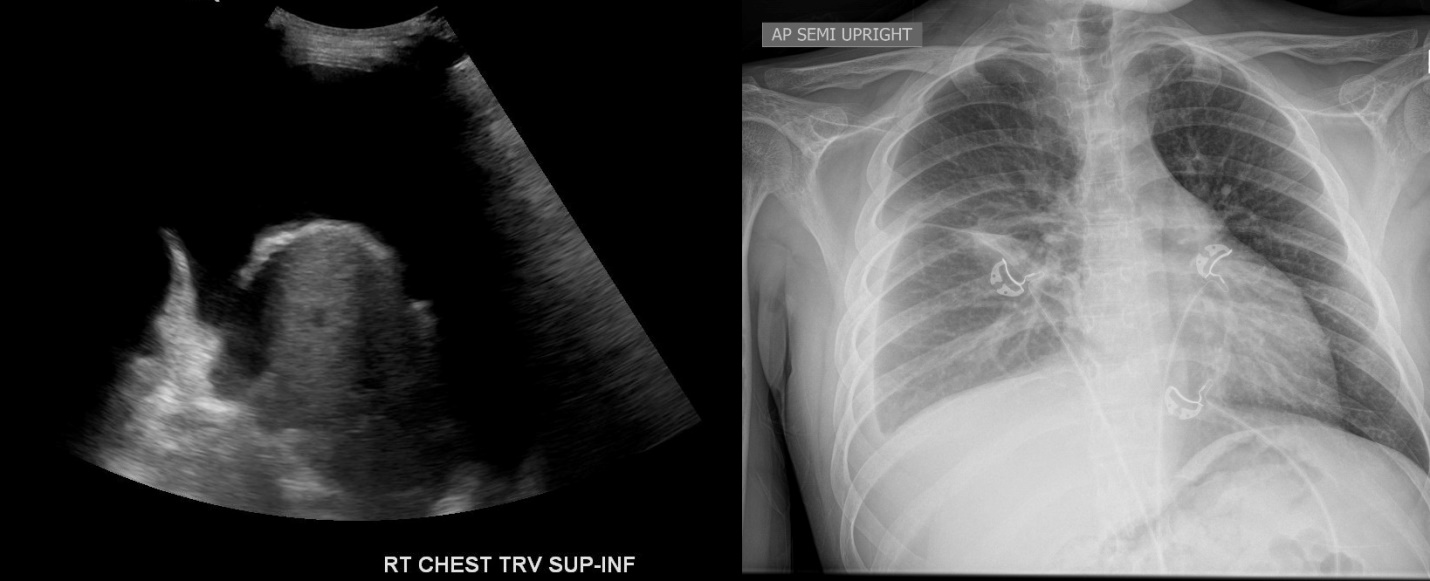
Figure: Figure 1: CXR and Ultrasound chest showing moderate right sided pleural effusion
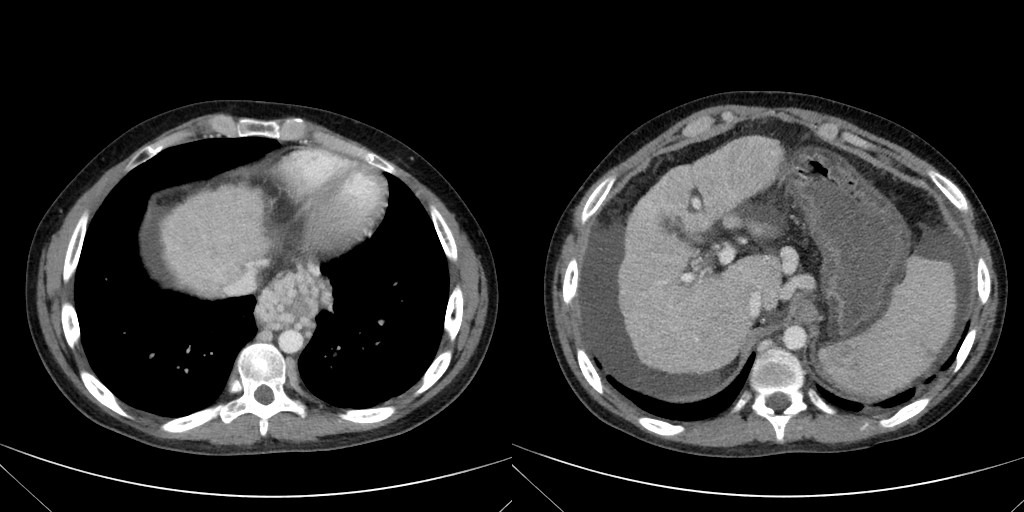
Figure: Figure 2: CT Abdomen and Pelvis showing cirrhotic liver morphology with numerous para-esophageal and gastric varices re-canalized umbilical vein
Disclosures:
Nouman Shafique indicated no relevant financial relationships.
Anurag Karki indicated no relevant financial relationships.
Amna Malik indicated no relevant financial relationships.
Sobaan Taj indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
George Everett indicated no relevant financial relationships.
Nouman Shafique, MD1, Anurag Karki, MD2, Amna Malik, MD2, Sobaan Taj, MD2, Aimen Farooq, MD3, George Everett, MD2. P3936 - Hepatic Hydrothorax in Dyskeratosis Congenita: A Rare Complication of Telomere Biology Disorder-Associated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
