Monday Poster Session
Category: Liver
P3912 - Rapidly Progressive Splanchnic Thrombosis in Essential Thrombocytosis: When Anticoagulation Isn’t Enough
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AY
Aneeq Muhammad Yousuf, MD
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Aneeq Muhammad Yousuf, MD1, Christopher G. Moody, DO2, Namrata Paladugu, MD1, Joydeep Chakraborty, MD1
1University of Mississippi Medical Center, Jackson, MS; 2University of Mississippi Medical Center - - Jackson, MS, Brandon, MS
Introduction: Splanchnic venous thrombosis (SVT) includes thrombosis of splenic, mesenteric, portal, and hepatic veins. Portal (PV) and mesenteric veins are most commonly affected, whereas hepatic vein involvement, known as Budd-Chiari syndrome (BCS), is less common. We present a complex case of extensive SVT requiring peritoneovenous (Denver) shunt placement in the setting of essential thrombocytosis (ET).
Case Description/
Methods: A 38-year-old female with ET (JAK2 V617F mutation) presented to an outside hospital with acute onset abdominal distension occurring overnight. She denied fever, confusion, or yellowing of eyes. Examination showed a tense, distended abdomen with positive fluid wave, without scleral icterus or asterixis. Laboratory studies revealed ALT 675 U/L, AST 287 U/L, total bilirubin 0.5 mg/dL, albumin 3.1 g/dL, serum ascites albumin gradient >1.1, ascitic fluid protein < 2.5 g/dl and INR 1.3. Initial Computed Tomography (CT) indicated a non-cirrhotic liver with heterogeneous enhancement, marked ascites, and caudate lobe prominence, without clear evaluation of vascular patency. Viral, autoimmune, and cholestatic serologies were negative. Liver biopsy indicated severe hepatic congestion without fibrosis. Subsequent Magnetic Resonance Imaging showed extensive thrombosis involving hepatic veins, main and right PV, superior mesenteric vein, and proximal splenic vein occlusion. The patient began heparin anticoagulation therapy and was transferred to our center for PV recanalization.
Interventional radiology (IR) attempted direct intrahepatic portocaval shunt placement, which failed due to extensive clot burden. The patient developed acute abdominal pain with worsening liver and renal function. Triple-phase CT demonstrated clot extension into the infrarenal inferior vena cava (IVC) and new left PV thrombosis. An emergent IVC thrombectomy was successful, with subsequent improvement of liver enzymes and renal function. Because of refractory ascites, PV recanalization was reattempted via transplenic and transhepatic access but was unsuccessful due to complete SVT. Due to persistent refractory ascites, a Denver shunt was placed by Hepatobiliary surgeon, leading to substantial improvement of ascites.
Discussion: Extensive SVT combined with BCS is rare but can occur in hypercoagulable states, posing significant therapeutic challenges. While anticoagulation remains first-line treatment, rapid clot progression as seen in this patient highlights the importance of prompt multi-disciplinary interventions.
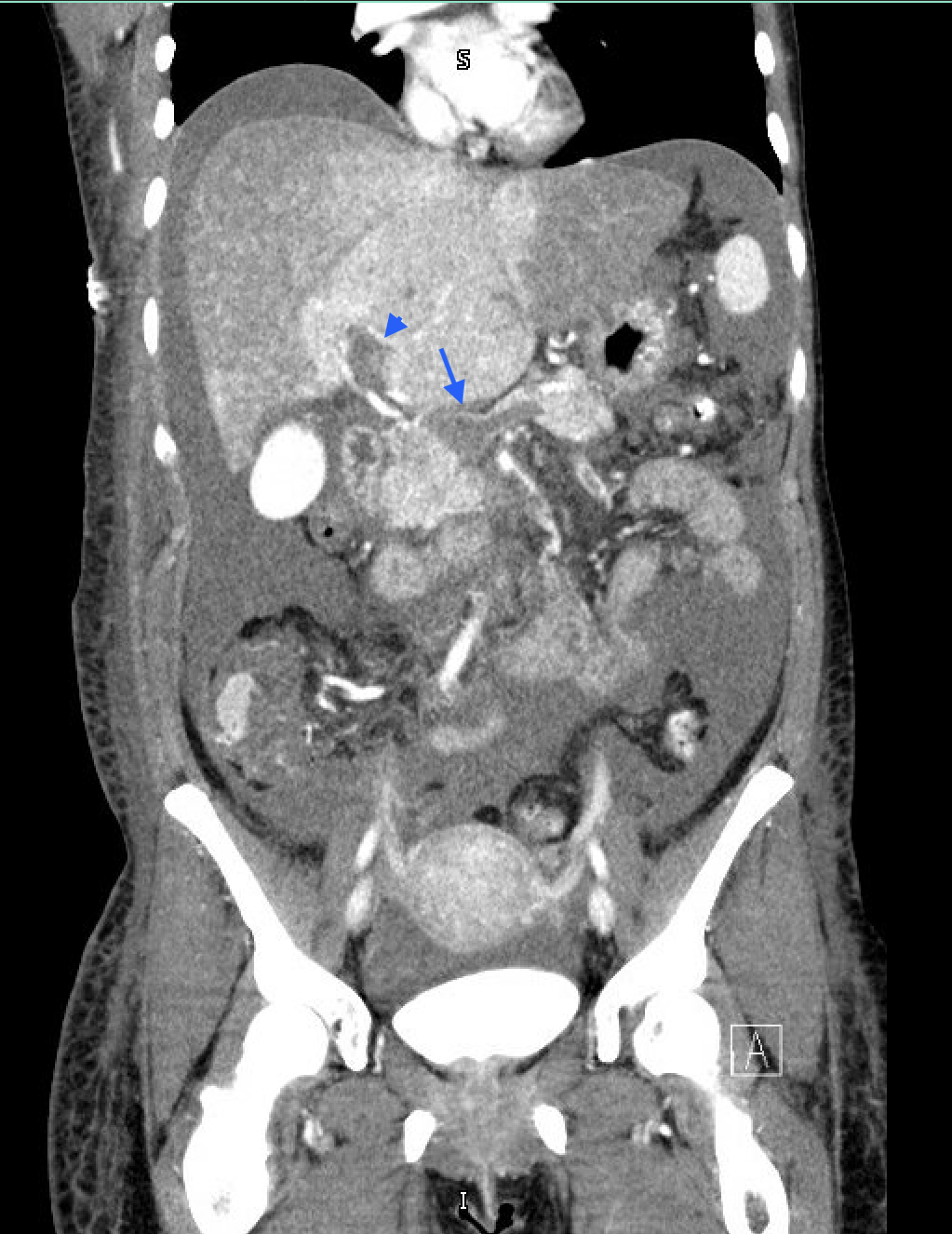
Figure: Figure 1: CT Triple Phase (Coronal View); Arrowhead: Main Portal Vein thrombosis; Arrow: Thrombosis at the confluence of Splenic, Superior Mesenteric Vein and Portal Vein

Figure: Figure 2: CT Triple phase (Coronal view); Arrowhead: Right Portal Vein thrombosis; Arrow: Suprahepatic IVC thrombosis extending to middle hepatic vein
Disclosures:
Aneeq Muhammad Yousuf indicated no relevant financial relationships.
Christopher Moody indicated no relevant financial relationships.
Namrata Paladugu indicated no relevant financial relationships.
Joydeep Chakraborty indicated no relevant financial relationships.
Aneeq Muhammad Yousuf, MD1, Christopher G. Moody, DO2, Namrata Paladugu, MD1, Joydeep Chakraborty, MD1. P3912 - Rapidly Progressive Splanchnic Thrombosis in Essential Thrombocytosis: When Anticoagulation Isn’t Enough, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Mississippi Medical Center, Jackson, MS; 2University of Mississippi Medical Center - - Jackson, MS, Brandon, MS
Introduction: Splanchnic venous thrombosis (SVT) includes thrombosis of splenic, mesenteric, portal, and hepatic veins. Portal (PV) and mesenteric veins are most commonly affected, whereas hepatic vein involvement, known as Budd-Chiari syndrome (BCS), is less common. We present a complex case of extensive SVT requiring peritoneovenous (Denver) shunt placement in the setting of essential thrombocytosis (ET).
Case Description/
Methods: A 38-year-old female with ET (JAK2 V617F mutation) presented to an outside hospital with acute onset abdominal distension occurring overnight. She denied fever, confusion, or yellowing of eyes. Examination showed a tense, distended abdomen with positive fluid wave, without scleral icterus or asterixis. Laboratory studies revealed ALT 675 U/L, AST 287 U/L, total bilirubin 0.5 mg/dL, albumin 3.1 g/dL, serum ascites albumin gradient >1.1, ascitic fluid protein < 2.5 g/dl and INR 1.3. Initial Computed Tomography (CT) indicated a non-cirrhotic liver with heterogeneous enhancement, marked ascites, and caudate lobe prominence, without clear evaluation of vascular patency. Viral, autoimmune, and cholestatic serologies were negative. Liver biopsy indicated severe hepatic congestion without fibrosis. Subsequent Magnetic Resonance Imaging showed extensive thrombosis involving hepatic veins, main and right PV, superior mesenteric vein, and proximal splenic vein occlusion. The patient began heparin anticoagulation therapy and was transferred to our center for PV recanalization.
Interventional radiology (IR) attempted direct intrahepatic portocaval shunt placement, which failed due to extensive clot burden. The patient developed acute abdominal pain with worsening liver and renal function. Triple-phase CT demonstrated clot extension into the infrarenal inferior vena cava (IVC) and new left PV thrombosis. An emergent IVC thrombectomy was successful, with subsequent improvement of liver enzymes and renal function. Because of refractory ascites, PV recanalization was reattempted via transplenic and transhepatic access but was unsuccessful due to complete SVT. Due to persistent refractory ascites, a Denver shunt was placed by Hepatobiliary surgeon, leading to substantial improvement of ascites.
Discussion: Extensive SVT combined with BCS is rare but can occur in hypercoagulable states, posing significant therapeutic challenges. While anticoagulation remains first-line treatment, rapid clot progression as seen in this patient highlights the importance of prompt multi-disciplinary interventions.
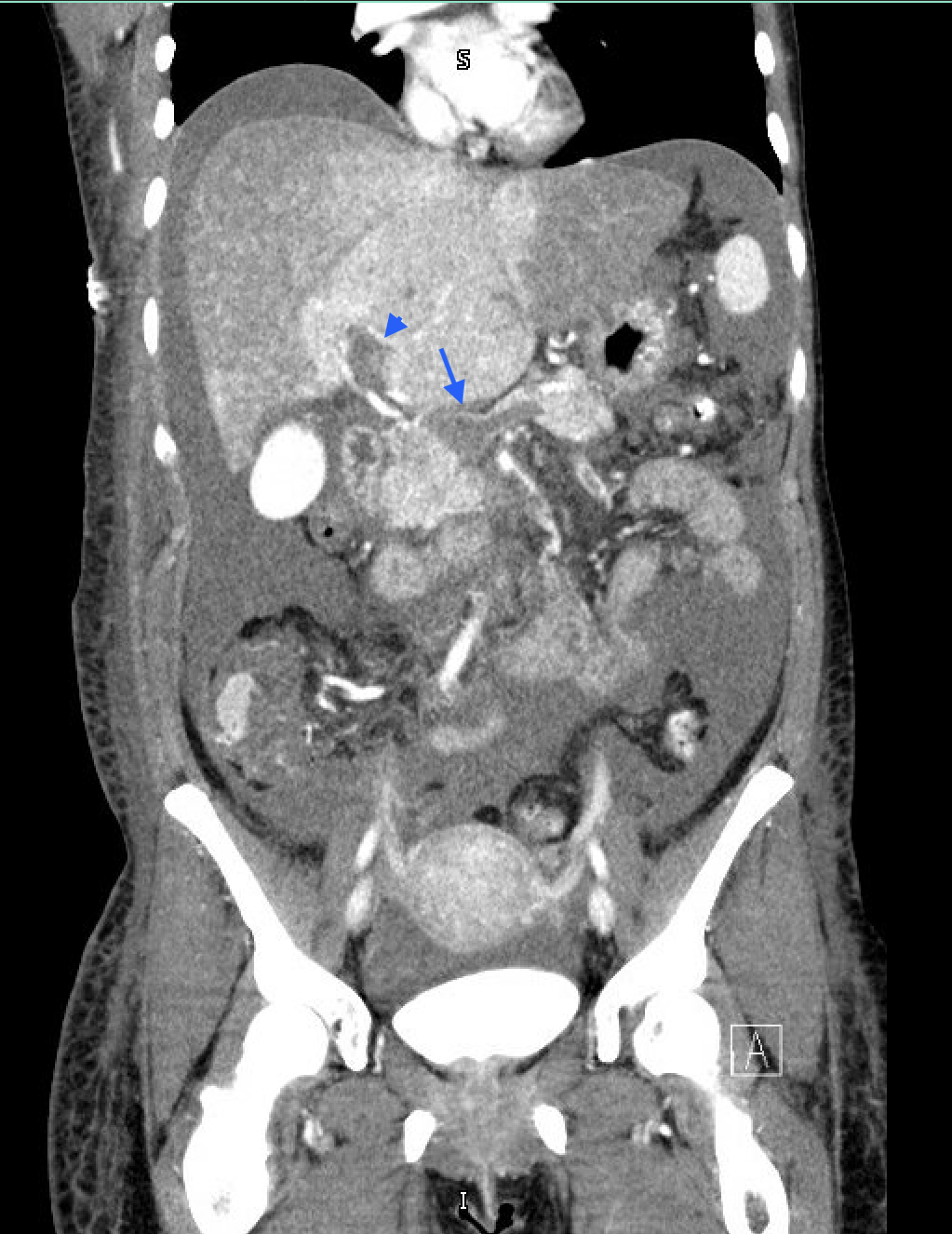
Figure: Figure 1: CT Triple Phase (Coronal View); Arrowhead: Main Portal Vein thrombosis; Arrow: Thrombosis at the confluence of Splenic, Superior Mesenteric Vein and Portal Vein

Figure: Figure 2: CT Triple phase (Coronal view); Arrowhead: Right Portal Vein thrombosis; Arrow: Suprahepatic IVC thrombosis extending to middle hepatic vein
Disclosures:
Aneeq Muhammad Yousuf indicated no relevant financial relationships.
Christopher Moody indicated no relevant financial relationships.
Namrata Paladugu indicated no relevant financial relationships.
Joydeep Chakraborty indicated no relevant financial relationships.
Aneeq Muhammad Yousuf, MD1, Christopher G. Moody, DO2, Namrata Paladugu, MD1, Joydeep Chakraborty, MD1. P3912 - Rapidly Progressive Splanchnic Thrombosis in Essential Thrombocytosis: When Anticoagulation Isn’t Enough, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
