Monday Poster Session
Category: Liver
P3910 - "Liver Dyspnea:" Unexpected Profound Hypoxia on Newly Diagnosed Liver Cirrhosis - A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cinthia Reyes Cruz, MD
University of Miami Miller School of Medicine at Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Cinthia Reyes Cruz, MD, Shahryar Jafri, MD, Eric Salkey, MD, Melaine Lanza, MD, Nemer Dabage-Forzoli, MD
University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL
Introduction: Hepatopulmonary syndrome (HPS) is a serious pulmonary vascular complication of cirrhosis, characterized by intrapulmonary vascular dilations leading to impaired oxygenation. The prevalence of HPS among patients with cirrhosis in the United States ranges from 4% to 32%. HPS is more common in advanced-stage cirrhosis, particularly in those being evaluated for liver transplantation, whereas it is less frequent in early-stage cirrhosis.
Case Description/
Methods: A 33-year-old male with a history of pituitary adenoma on steroids, presented to the pulmonology clinic with dyspnea and a dry cough for three months. During the visit, oxygen saturation was noted to be 88% on room air, dropping to 75% after minimal exertion. He was placed on supplemental oxygen and referred to the emergency department. On arrival, he remained hypoxic. A computed tomography pulmonary angiogram, was negative for pulmonary embolism but revealed cirrhotic liver morphology. Laboratory evaluation showed aspartate aminotransferase 59 U/L, total bilirubin 1.4 mg/dL, gamma-glutamyl transferase 109 U/L, platelet count 36,000/µL.
A vascular abdominal ultrasound demonstrated hepatic cirrhosis, and patent portal venous system. A nuclear medicine ventilation-perfusion scan revealed a right-to-left shunt. A transesophageal echocardiogram (TEE) was performed, which ruled out a patent foramen ovale (PFO) but confirmed an extracardiac shunt, given the appearance of saline contrast bubbles in the left atrium 5 cardiac cycles after right atrial opacification, suggestive of HPS.
Liver biopsy confirmed cirrhosis, no steatosis.Serologic liver and autoimmune workup was unremarkable (Table 1). The etiology of his cirrhosis was attributed to “burnt-out” nonalcoholic steatohepatitis, secondary to long-term steroid use. The patient then established care with gastroenterology and was discharged on long-term oxygen therapy. He was referred to a transplant hepatology center for evaluation.
Discussion: This case highlights the importance of considering HPS in the evaluation of unexplained hypoxia, even in patients without advanced liver disease or with only mild liver function test abnormalities. While HPS is more common in end-stage cirrhosis, it can present in earlier stages, as seen in this patient with a MELD score of 10. Early recognition is crucial, as liver transplantation remains the only curative option. We emphasize the high value of thoroughly ruling out other potential right-to-left shunts, such as a PFO or pulmonary vascular malformations.
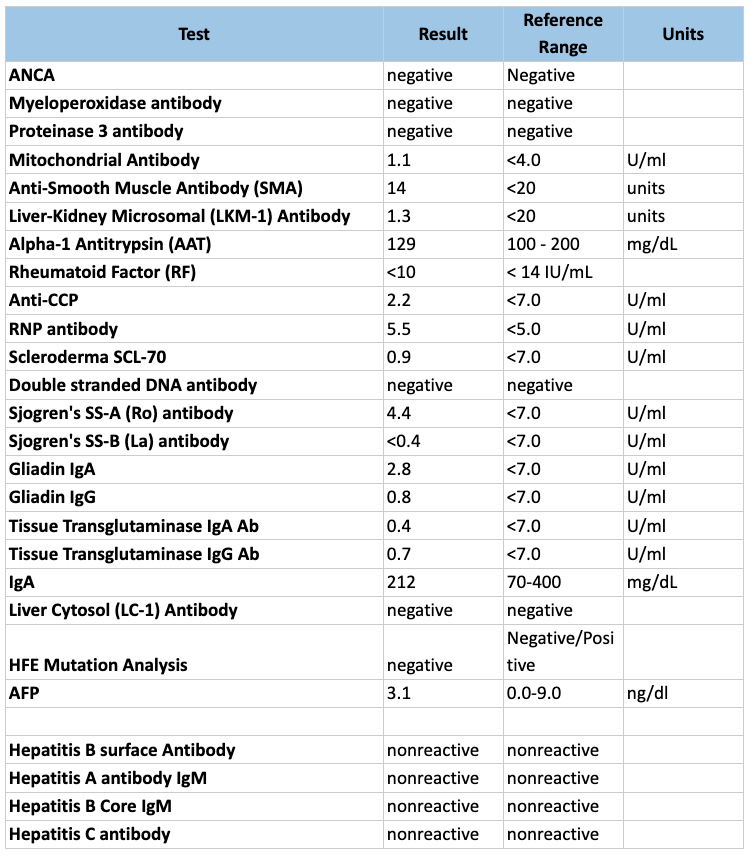
Figure: Table 1. Liver disease and autoimmune panel laboratory results
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Shahryar Jafri indicated no relevant financial relationships.
Eric Salkey indicated no relevant financial relationships.
Melaine Lanza indicated no relevant financial relationships.
Nemer Dabage-Forzoli indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD, Shahryar Jafri, MD, Eric Salkey, MD, Melaine Lanza, MD, Nemer Dabage-Forzoli, MD. P3910 - "Liver Dyspnea:" Unexpected Profound Hypoxia on Newly Diagnosed Liver Cirrhosis - A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Miami Miller School of Medicine at Holy Cross Hospital, Fort Lauderdale, FL
Introduction: Hepatopulmonary syndrome (HPS) is a serious pulmonary vascular complication of cirrhosis, characterized by intrapulmonary vascular dilations leading to impaired oxygenation. The prevalence of HPS among patients with cirrhosis in the United States ranges from 4% to 32%. HPS is more common in advanced-stage cirrhosis, particularly in those being evaluated for liver transplantation, whereas it is less frequent in early-stage cirrhosis.
Case Description/
Methods: A 33-year-old male with a history of pituitary adenoma on steroids, presented to the pulmonology clinic with dyspnea and a dry cough for three months. During the visit, oxygen saturation was noted to be 88% on room air, dropping to 75% after minimal exertion. He was placed on supplemental oxygen and referred to the emergency department. On arrival, he remained hypoxic. A computed tomography pulmonary angiogram, was negative for pulmonary embolism but revealed cirrhotic liver morphology. Laboratory evaluation showed aspartate aminotransferase 59 U/L, total bilirubin 1.4 mg/dL, gamma-glutamyl transferase 109 U/L, platelet count 36,000/µL.
A vascular abdominal ultrasound demonstrated hepatic cirrhosis, and patent portal venous system. A nuclear medicine ventilation-perfusion scan revealed a right-to-left shunt. A transesophageal echocardiogram (TEE) was performed, which ruled out a patent foramen ovale (PFO) but confirmed an extracardiac shunt, given the appearance of saline contrast bubbles in the left atrium 5 cardiac cycles after right atrial opacification, suggestive of HPS.
Liver biopsy confirmed cirrhosis, no steatosis.Serologic liver and autoimmune workup was unremarkable (Table 1). The etiology of his cirrhosis was attributed to “burnt-out” nonalcoholic steatohepatitis, secondary to long-term steroid use. The patient then established care with gastroenterology and was discharged on long-term oxygen therapy. He was referred to a transplant hepatology center for evaluation.
Discussion: This case highlights the importance of considering HPS in the evaluation of unexplained hypoxia, even in patients without advanced liver disease or with only mild liver function test abnormalities. While HPS is more common in end-stage cirrhosis, it can present in earlier stages, as seen in this patient with a MELD score of 10. Early recognition is crucial, as liver transplantation remains the only curative option. We emphasize the high value of thoroughly ruling out other potential right-to-left shunts, such as a PFO or pulmonary vascular malformations.
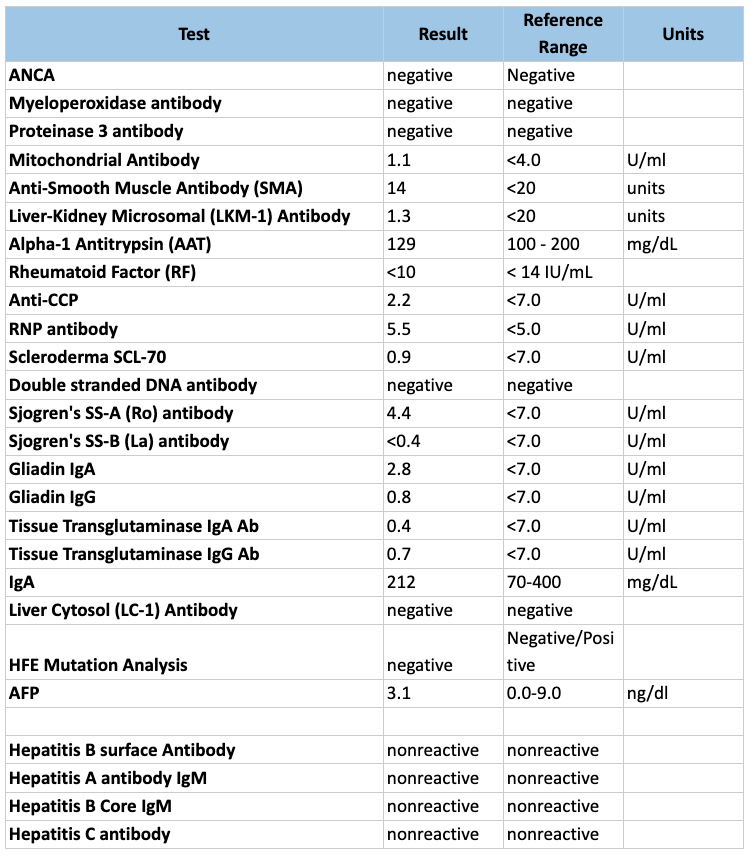
Figure: Table 1. Liver disease and autoimmune panel laboratory results
Disclosures:
Cinthia Reyes Cruz indicated no relevant financial relationships.
Shahryar Jafri indicated no relevant financial relationships.
Eric Salkey indicated no relevant financial relationships.
Melaine Lanza indicated no relevant financial relationships.
Nemer Dabage-Forzoli indicated no relevant financial relationships.
Cinthia Reyes Cruz, MD, Shahryar Jafri, MD, Eric Salkey, MD, Melaine Lanza, MD, Nemer Dabage-Forzoli, MD. P3910 - "Liver Dyspnea:" Unexpected Profound Hypoxia on Newly Diagnosed Liver Cirrhosis - A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
