Monday Poster Session
Category: Liver
P3907 - An Unusual Case of Portal Hypertension
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Winoah A. Henry, MD, FACG (she/her/hers)
Central Maine Medical Center
Lewiston, ME
Presenting Author(s)
Winoah A. Henry, MD, FACG
Central Maine Medical Center, Lewiston, ME
Introduction: In rare cases, portal hypertension (pHTN) is presinusoidal and occurs in the absence of cirrhosis such as portosinusoidal vascular disorder (PSVD). PSVD is a clinicopathologic diagnosis with various histologic findings including hepatoportal sclerosis (HPS). Herein, we describe this rare case of portal hypertension.
Case Description/
Methods: A 35 yr old F with history of untreated PVT presents with two episodes of hematemesis. Other than a palpable spleen the exam was normal. Hgb 5.9 g/dL, Platelet 66 U/L, INR 1.2, TBili 0.4, ALP 63, AST 30 and ALT 30. Hepatitis A/B immune, hepatitis C and HIV negative. Ceruloplasmin, alpha-1 antitrypsin, celiac, ANA, ASMA, AMA negative. Ig A and IgM normal and IgG was 1743 mg/dL (600-1640). Hypercoagulable work up negative. No OCP use. Family history is positive for alcohol-related cirrhosis. Patient drank alcohol on occasion, smoked Cannabis and tobacco, used cocaine, ecstasy and molly but denied IVDU. Abd/Pelvic CT showed a posterior notch sign, cavernous transformation of the portal vein (PV), 18.4 cm spleen, trace ascites, portal colopathy, abdominal varices, and no thrombosis. On EGD, there were F3 esophgeal varices with stigmata s/p EVL. Outpatient elastography was 4.8 kPa with a CAP of 230 dB/m. Due to concern for non-cirrhotic pHTN, a liver biopsy was performed and showed PV herniation beyond the portal tract borders and focal portal vein sclerosis. There was no steatosis, no advanced fibrosis or cirrhosis on trichrome and reticulin stains. A diagnosis of HPS was made.
Discussion: HPS is rare in the Western world, the pathophysiology is unknown, and variceal bleeding in the absence of cirrhosis is the most common presentation. Other less common presentations include ascites, HE and PVT. A high clinical suspicion is important when imaging findings are equivocal for cirrhosis but there are signs of pHTN. In this case of variceal bleed and imaging signs of portal hypertension, normal liver enzymes as well as normal elastography helped support a low suspicion for cirrhosis and need for a diagnostic liver biopsy. While the etiology of HPS has not been elucidated multiple derangements may impact endothelial integrity and vascular remodeling complicated by thrombosis and/or fibroproliferation leading to obstruction (phlebosclerosis) and pHTN. There have been many associations including toxins, medications, and genetic disorders such as short telomeres syndrome. Treatment is focused on managing portal hypertension.
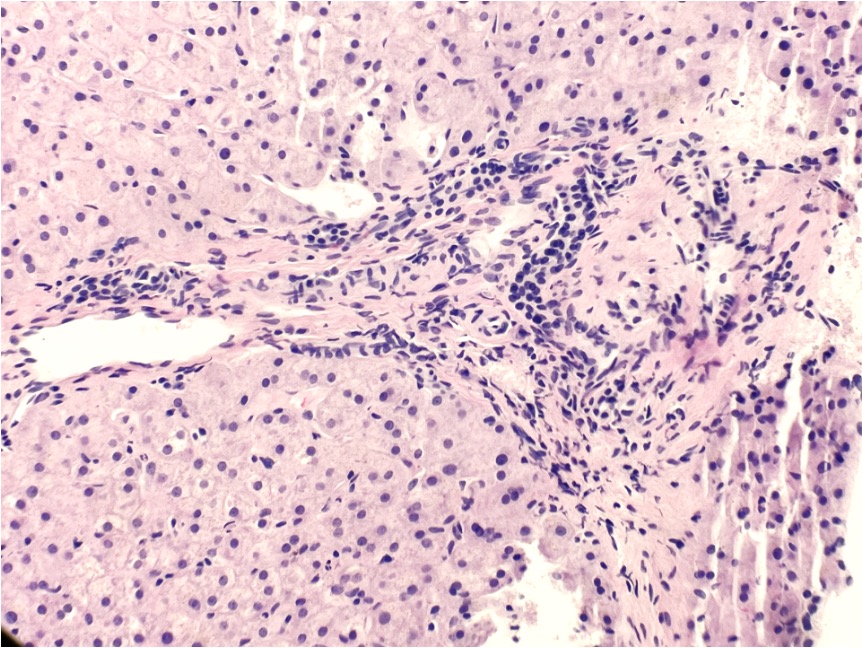
Figure: Portal vein sclerosis and herniated portal vein
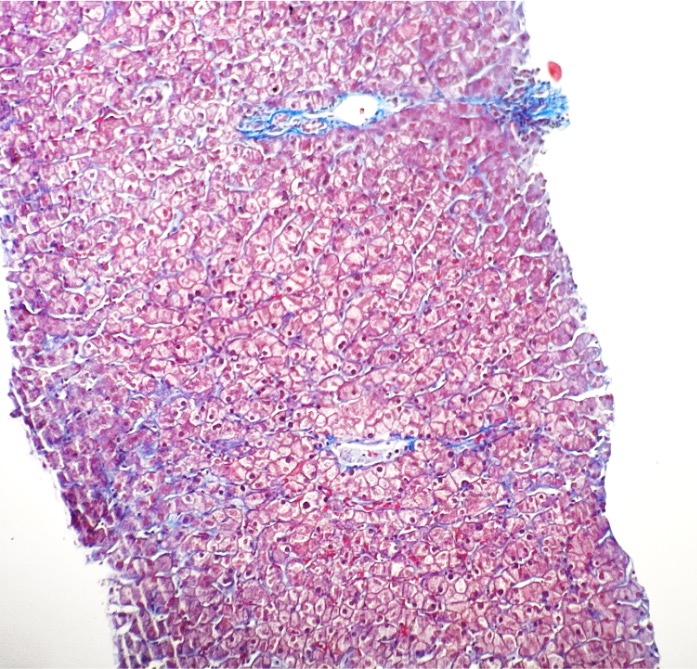
Figure: No fibrosis on trichrome stain
Disclosures:
Winoah Henry indicated no relevant financial relationships.
Winoah A. Henry, MD, FACG. P3907 - An Unusual Case of Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Central Maine Medical Center, Lewiston, ME
Introduction: In rare cases, portal hypertension (pHTN) is presinusoidal and occurs in the absence of cirrhosis such as portosinusoidal vascular disorder (PSVD). PSVD is a clinicopathologic diagnosis with various histologic findings including hepatoportal sclerosis (HPS). Herein, we describe this rare case of portal hypertension.
Case Description/
Methods: A 35 yr old F with history of untreated PVT presents with two episodes of hematemesis. Other than a palpable spleen the exam was normal. Hgb 5.9 g/dL, Platelet 66 U/L, INR 1.2, TBili 0.4, ALP 63, AST 30 and ALT 30. Hepatitis A/B immune, hepatitis C and HIV negative. Ceruloplasmin, alpha-1 antitrypsin, celiac, ANA, ASMA, AMA negative. Ig A and IgM normal and IgG was 1743 mg/dL (600-1640). Hypercoagulable work up negative. No OCP use. Family history is positive for alcohol-related cirrhosis. Patient drank alcohol on occasion, smoked Cannabis and tobacco, used cocaine, ecstasy and molly but denied IVDU. Abd/Pelvic CT showed a posterior notch sign, cavernous transformation of the portal vein (PV), 18.4 cm spleen, trace ascites, portal colopathy, abdominal varices, and no thrombosis. On EGD, there were F3 esophgeal varices with stigmata s/p EVL. Outpatient elastography was 4.8 kPa with a CAP of 230 dB/m. Due to concern for non-cirrhotic pHTN, a liver biopsy was performed and showed PV herniation beyond the portal tract borders and focal portal vein sclerosis. There was no steatosis, no advanced fibrosis or cirrhosis on trichrome and reticulin stains. A diagnosis of HPS was made.
Discussion: HPS is rare in the Western world, the pathophysiology is unknown, and variceal bleeding in the absence of cirrhosis is the most common presentation. Other less common presentations include ascites, HE and PVT. A high clinical suspicion is important when imaging findings are equivocal for cirrhosis but there are signs of pHTN. In this case of variceal bleed and imaging signs of portal hypertension, normal liver enzymes as well as normal elastography helped support a low suspicion for cirrhosis and need for a diagnostic liver biopsy. While the etiology of HPS has not been elucidated multiple derangements may impact endothelial integrity and vascular remodeling complicated by thrombosis and/or fibroproliferation leading to obstruction (phlebosclerosis) and pHTN. There have been many associations including toxins, medications, and genetic disorders such as short telomeres syndrome. Treatment is focused on managing portal hypertension.
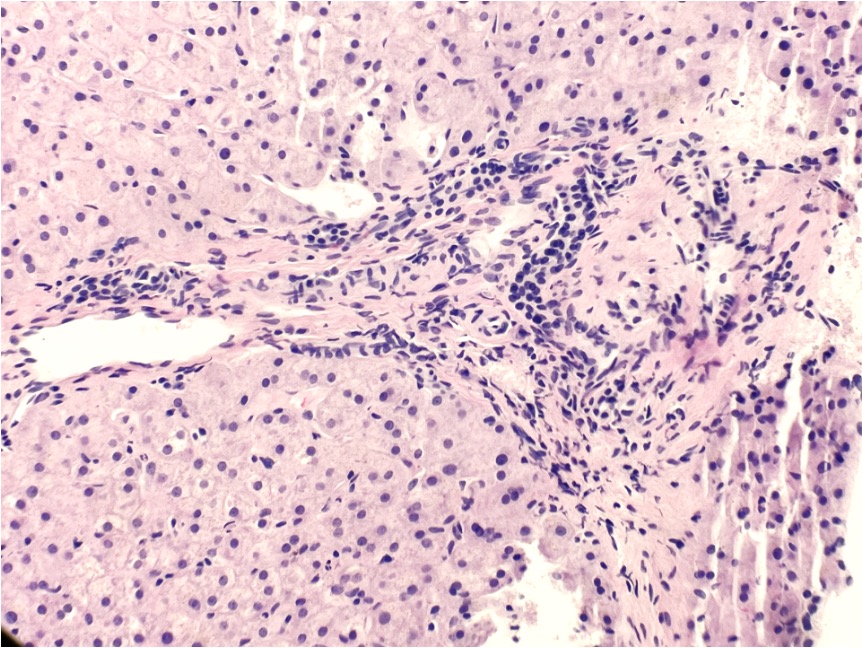
Figure: Portal vein sclerosis and herniated portal vein
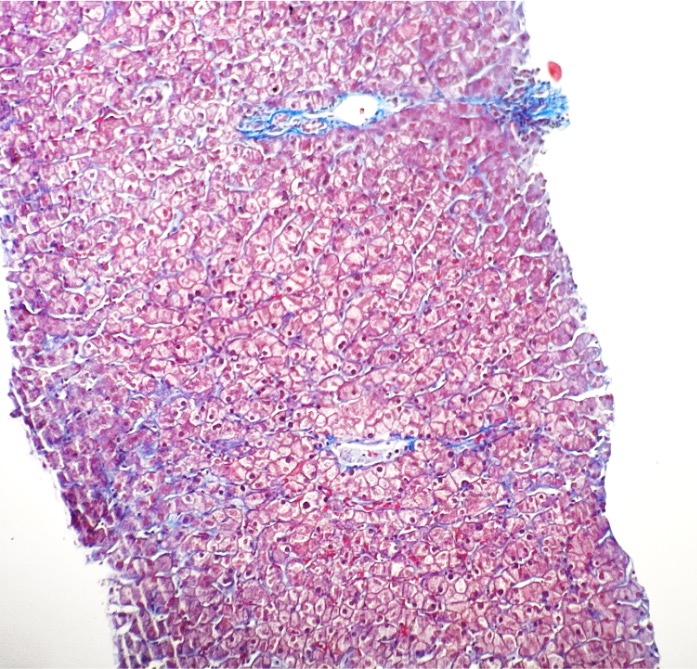
Figure: No fibrosis on trichrome stain
Disclosures:
Winoah Henry indicated no relevant financial relationships.
Winoah A. Henry, MD, FACG. P3907 - An Unusual Case of Portal Hypertension, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
