Monday Poster Session
Category: Liver
P3906 - From Psoas Abscess to Hemobilia: Unveiling a Case of Portal Biliopathy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Enoch Joseph Abbey, MD, MPH
NYC Health + Hospitals/Harlem
New York, NY
Presenting Author(s)
Enoch Joseph. Abbey, MD, MPH1, Daniyal Abbas, MD1, Joan A.. Culpepper-Morgan, MD, FACG2
1NYC Health + Hospitals/Harlem, New York, NY; 2NYC Health + Hospitals, New York, NY
Introduction: Extrahepatic portal vein obstruction (EHPVO) is a rare but serious consequence of deep-seated abdominal infections, often progressing silently to portal cavernoma and biliary complications. While osteomyelitis and psoas abscesses are typically localized infections, they may under certain conditions initiate septic thrombotic events involving the portal system. We describe a case of portal biliopathy with hemobilia, evolving from vertebral osteomyelitis and psoas abscess in the absence of known prothrombotic risk factors.
Case Description/
Methods: A 60-year-old black man with a history of T2DM presented with one day of epigastric abdominal pain, nausea, and vomiting. He denied jaundice or history of hepatitis. The patient had treatment 2 months ago for T12/L1 osteomyelitis with left psoas muscle MRSA abscess. On admission initial vital signs were stable. The patient was notably cachectic (BMI 15.7) but otherwise not in distress with a benign abdomen. Over the next week he had progressive worsening of liver enzymes with evidence of gall bladder distention without wall thickening or stones but dilated intrahepatic ducts (DAY: 5- Total Bili 1.1/ DB 0.5/ ALK 511/ ALT 424/ AST 184). There was no evidence of mass (fig). Although the patient had pain and rising liver enzymes, he remained afebrile and his white count was normal (WBC 6.7). He was given broad-spectrum antibiotics out of an abundance of caution. On hospital day 7 patient had an abrupt increase in WBC to 18.1. He had a seizure and was transferred to an OSH for emergent ERCP. There he was found to have hemobilia and was treated with a fully covered metal stent. Post procedure his Hb dropped to 5.7g/dL. CT abdomen revealed the stent in the CBD with pneumobilia, gallbladder containing intraluminal contrast, non-visualized portal vein, and superior mesenteric vein with cavernous transformation in the porta hepatis with numerous peripancreatic collaterals.
Discussion: While portal vein thrombosis is most often attributed to cirrhosis, malignancy, or thrombophilia, this case underscores the potential for deep tissue infection to precipitate septic thrombosis of the portal system. The development of cavernous transformation within weeks leads to biliary compression, portal ductopathy, and complications like choledocholithiasis and hemobilia, particularly during endoscopic manipulation. Recognizing these complications early is critical, especially when infection and thrombosis intersect.
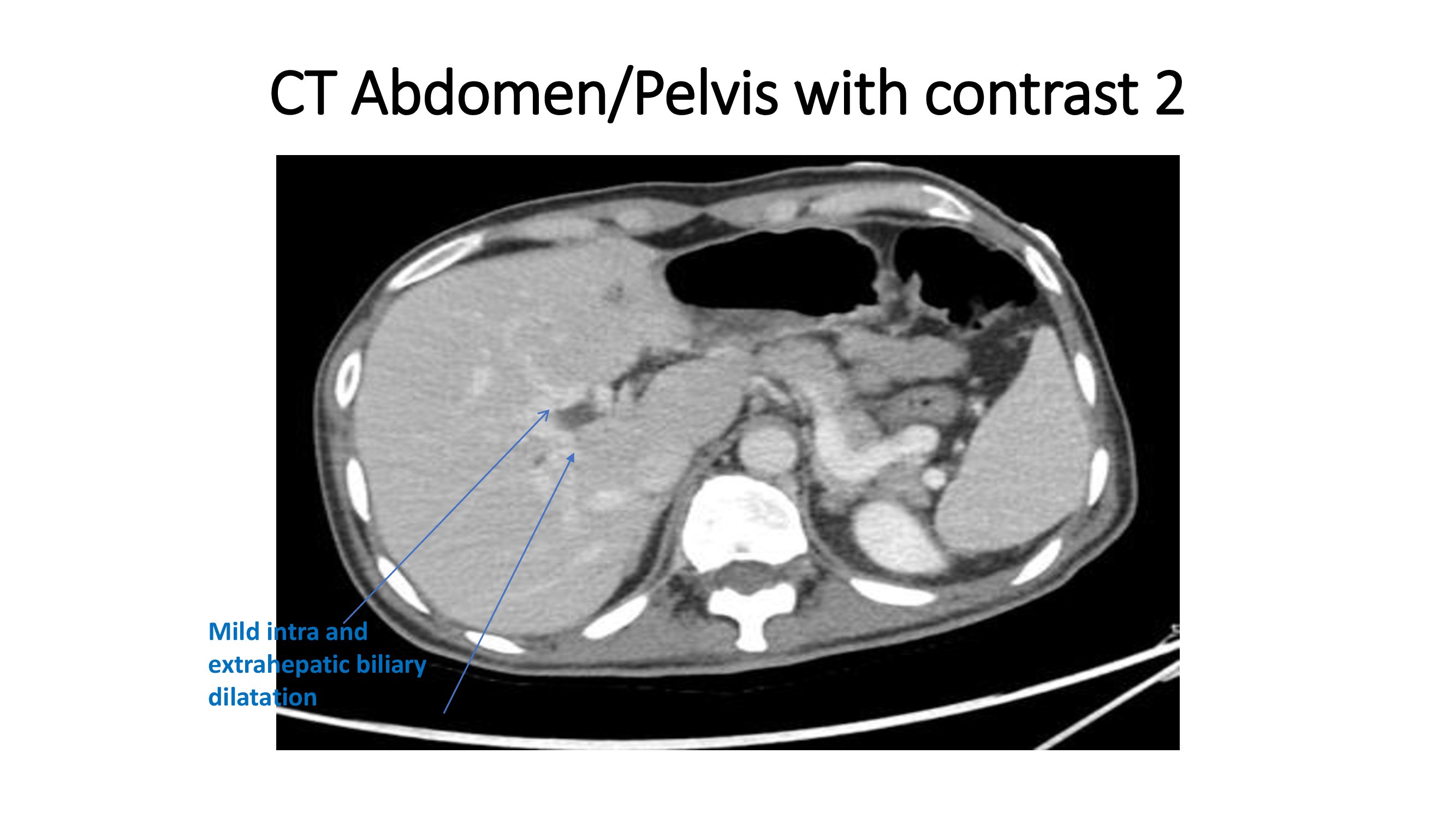
Figure: CT scan of abdomen and pelvis with contrast
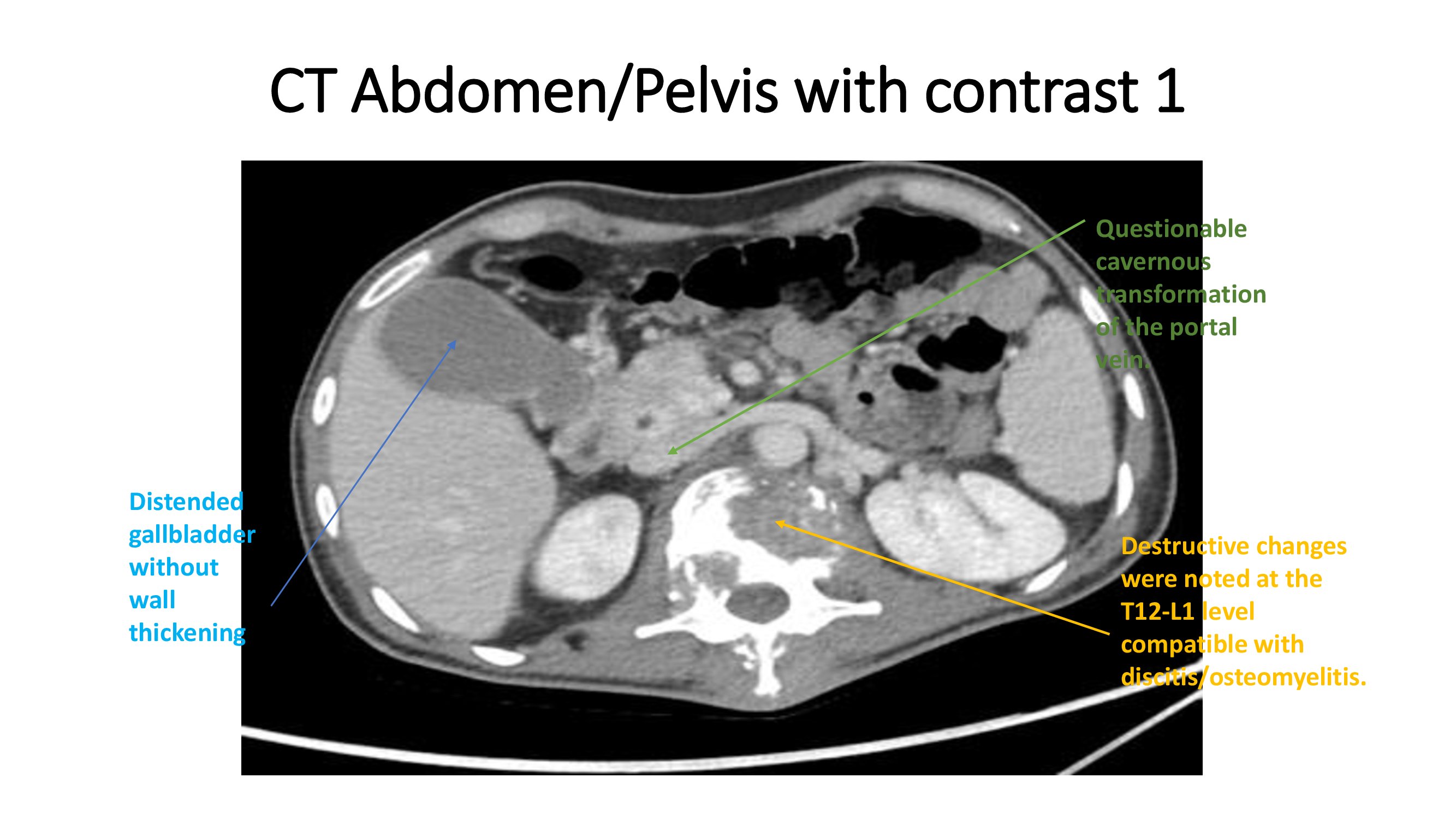
Figure: CT scan of abdomen and pelvis with contrast
Disclosures:
Enoch Abbey indicated no relevant financial relationships.
Daniyal Abbas indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Enoch Joseph. Abbey, MD, MPH1, Daniyal Abbas, MD1, Joan A.. Culpepper-Morgan, MD, FACG2. P3906 - From Psoas Abscess to Hemobilia: Unveiling a Case of Portal Biliopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Harlem, New York, NY; 2NYC Health + Hospitals, New York, NY
Introduction: Extrahepatic portal vein obstruction (EHPVO) is a rare but serious consequence of deep-seated abdominal infections, often progressing silently to portal cavernoma and biliary complications. While osteomyelitis and psoas abscesses are typically localized infections, they may under certain conditions initiate septic thrombotic events involving the portal system. We describe a case of portal biliopathy with hemobilia, evolving from vertebral osteomyelitis and psoas abscess in the absence of known prothrombotic risk factors.
Case Description/
Methods: A 60-year-old black man with a history of T2DM presented with one day of epigastric abdominal pain, nausea, and vomiting. He denied jaundice or history of hepatitis. The patient had treatment 2 months ago for T12/L1 osteomyelitis with left psoas muscle MRSA abscess. On admission initial vital signs were stable. The patient was notably cachectic (BMI 15.7) but otherwise not in distress with a benign abdomen. Over the next week he had progressive worsening of liver enzymes with evidence of gall bladder distention without wall thickening or stones but dilated intrahepatic ducts (DAY: 5- Total Bili 1.1/ DB 0.5/ ALK 511/ ALT 424/ AST 184). There was no evidence of mass (fig). Although the patient had pain and rising liver enzymes, he remained afebrile and his white count was normal (WBC 6.7). He was given broad-spectrum antibiotics out of an abundance of caution. On hospital day 7 patient had an abrupt increase in WBC to 18.1. He had a seizure and was transferred to an OSH for emergent ERCP. There he was found to have hemobilia and was treated with a fully covered metal stent. Post procedure his Hb dropped to 5.7g/dL. CT abdomen revealed the stent in the CBD with pneumobilia, gallbladder containing intraluminal contrast, non-visualized portal vein, and superior mesenteric vein with cavernous transformation in the porta hepatis with numerous peripancreatic collaterals.
Discussion: While portal vein thrombosis is most often attributed to cirrhosis, malignancy, or thrombophilia, this case underscores the potential for deep tissue infection to precipitate septic thrombosis of the portal system. The development of cavernous transformation within weeks leads to biliary compression, portal ductopathy, and complications like choledocholithiasis and hemobilia, particularly during endoscopic manipulation. Recognizing these complications early is critical, especially when infection and thrombosis intersect.
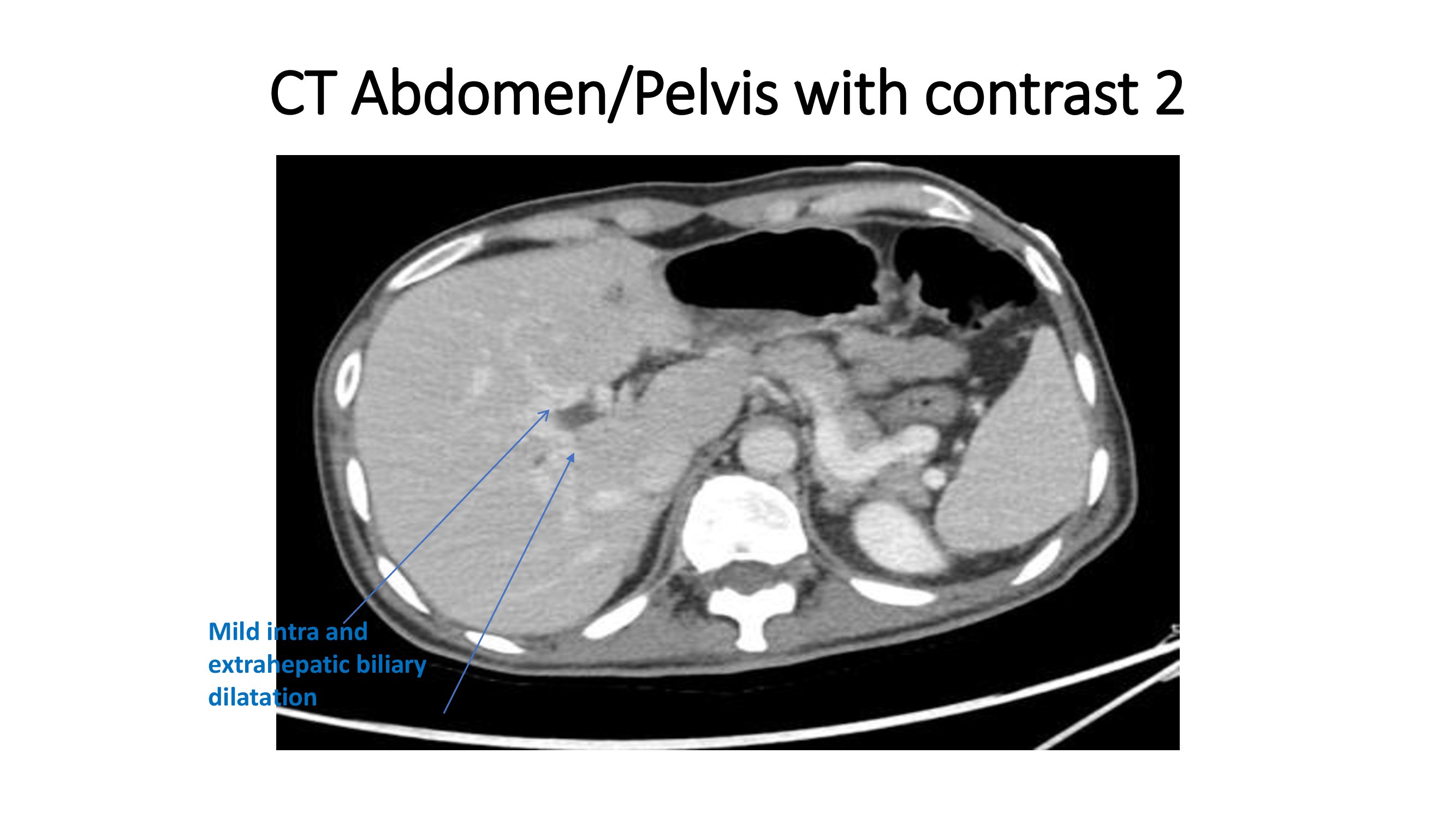
Figure: CT scan of abdomen and pelvis with contrast
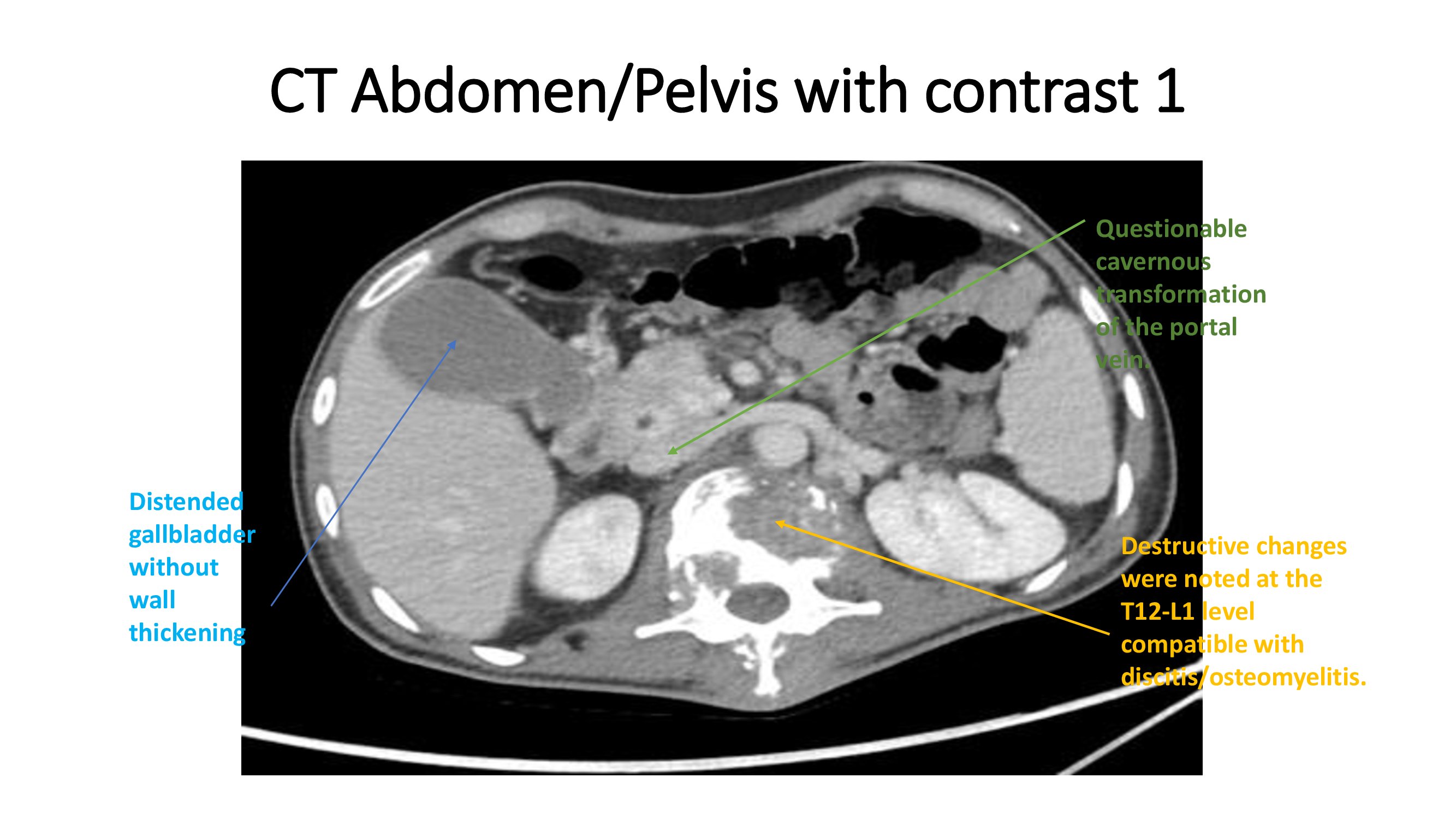
Figure: CT scan of abdomen and pelvis with contrast
Disclosures:
Enoch Abbey indicated no relevant financial relationships.
Daniyal Abbas indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Enoch Joseph. Abbey, MD, MPH1, Daniyal Abbas, MD1, Joan A.. Culpepper-Morgan, MD, FACG2. P3906 - From Psoas Abscess to Hemobilia: Unveiling a Case of Portal Biliopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
