Monday Poster Session
Category: Liver
P3903 - A Curious Case of Auto-Brewery Syndrome in a Patient Undergoing Liver Transplant Evaluation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jeff Angelo F. Taclob, MD
University of Tennessee Health Science Center - Methodist University Hospital
Lubbock, TX
Presenting Author(s)
Jeff Angelo Taclob, MD1, Lauren Lyssy, DO1, Shehnaz Nansiyani, FNP1, Beth Ruiz, PA-C1, Satheesh Nair, MD2
1University of Tennessee Health Science Center - Methodist University Hospital, Memphis, TN; 2Methodist LeBonheur Healthcare, Memphis, TN
Introduction: Serum Posphatidylethanol (PEth) is a biomarker for alcohol use with high specificity and sensitivity. It has become the gold standard in evaluating fatty liver disease and determining eligibility for liver transplant. Auto-brewery syndrome (ABS), also known as “gut fermentation syndrome,” occurs when endogenous ethanol is produced by fermentation of carbohydrates in the intestinal tract by microorganisms such as Candida and Saccharomyces.
Case Description/
Methods: A 60 y/o Caucasian male was diagnosed with cirrhosis in 2011 after an abdominal CT scan following a motor vehicle accident. He had HCV and was referred to our liver clinic. He was drinking 3-4 beers daily and stopped completely after being diagnosed with cirrhosis. HCV was cured with sofosbuvir and ribavirin in 2012. He was followed by his PCP and was referred back in 2021 after developing hepatic encephalopathy. On evaluation, PEth was 20 ng/mL (lower limit of detection). However, he had denied any alcohol intake since 2011. He continued to follow in our transplant center, and in 2023, his PEth was 119 ng/mL despite being abstinent. He had reported feelings of intoxication after carbohydrate-rich meals. His abdominal scans showed "large stomach with food contents” (Fig 1). Retained food was also seen in EGD, confirming delayed gastric emptying. He was given a course of fluconazole, and his PEth became negative. A few weeks after completing fluconazole, PEth was again detectable at low levels. The patient was extensively evaluated by the transplant psychosocial team and determined to have been truly abstinent since 2011. After another course of fluconazole, the PEth test became negative, supporting Candida-related fermentation as the cause. The CT scan showed a large Hepatocellular carcinoma (6 cm), and transplant evaluation with down-staging protocol was started. Unfortunately, his HCC progressed despite Loco-Regional therapy (Fig 2).
Discussion: Our patient clearly had ABS, evidenced by three negative PEth tests following three fluconazole treatments. Given the implications of detectable PEth for liver disease management and transplant eligibility, clinicians should recognize the potential for ABS. One unanswered question in our patient is whether endogenous alcohol production contributed to the progression of his cirrhosis despite the eradication of HCV 13 years ago. While progression of cirrhosis is possible despite eradication of HCV, his delayed decompensation may be attributed to the recent onset of ABS and endogenous alcohol.
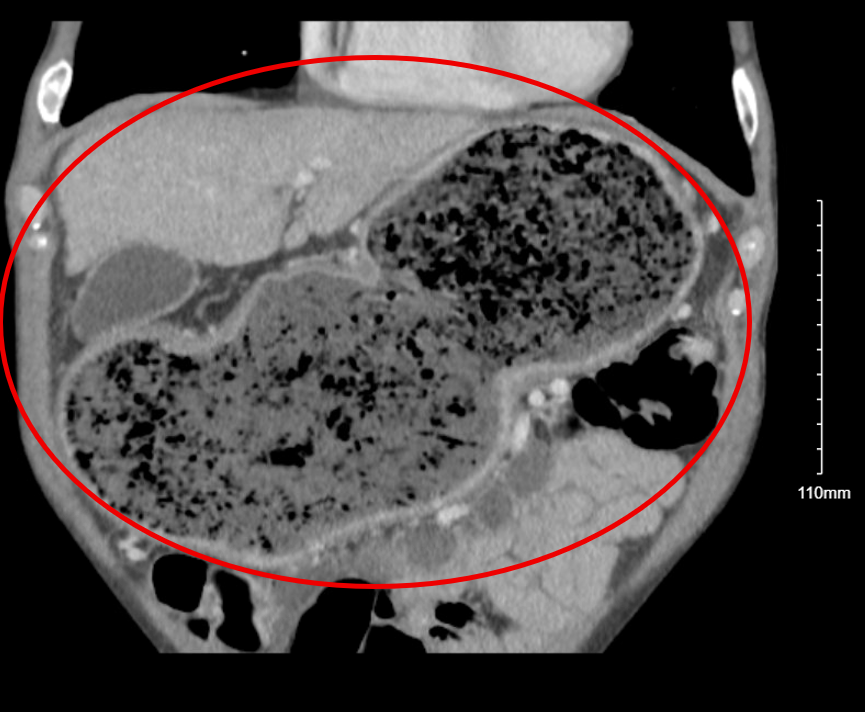
Figure: Fig 1. CT Scan of the abdomen. The coronal view shows a significantly dilated stomach (red circle).

Figure: Fig 2. CT Abdomen Triple Phase. The thin venous phase axial view shows numerous hypoenhancing nodules (red circle) throughout the right lobe of the liver, which is concerning for infiltrative HCC and indicative of progression of hepatocellular carcinoma.
Disclosures:
Jeff Angelo Taclob indicated no relevant financial relationships.
Lauren Lyssy indicated no relevant financial relationships.
Shehnaz Nansiyani indicated no relevant financial relationships.
Beth Ruiz indicated no relevant financial relationships.
Satheesh Nair indicated no relevant financial relationships.
Jeff Angelo Taclob, MD1, Lauren Lyssy, DO1, Shehnaz Nansiyani, FNP1, Beth Ruiz, PA-C1, Satheesh Nair, MD2. P3903 - A Curious Case of Auto-Brewery Syndrome in a Patient Undergoing Liver Transplant Evaluation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Tennessee Health Science Center - Methodist University Hospital, Memphis, TN; 2Methodist LeBonheur Healthcare, Memphis, TN
Introduction: Serum Posphatidylethanol (PEth) is a biomarker for alcohol use with high specificity and sensitivity. It has become the gold standard in evaluating fatty liver disease and determining eligibility for liver transplant. Auto-brewery syndrome (ABS), also known as “gut fermentation syndrome,” occurs when endogenous ethanol is produced by fermentation of carbohydrates in the intestinal tract by microorganisms such as Candida and Saccharomyces.
Case Description/
Methods: A 60 y/o Caucasian male was diagnosed with cirrhosis in 2011 after an abdominal CT scan following a motor vehicle accident. He had HCV and was referred to our liver clinic. He was drinking 3-4 beers daily and stopped completely after being diagnosed with cirrhosis. HCV was cured with sofosbuvir and ribavirin in 2012. He was followed by his PCP and was referred back in 2021 after developing hepatic encephalopathy. On evaluation, PEth was 20 ng/mL (lower limit of detection). However, he had denied any alcohol intake since 2011. He continued to follow in our transplant center, and in 2023, his PEth was 119 ng/mL despite being abstinent. He had reported feelings of intoxication after carbohydrate-rich meals. His abdominal scans showed "large stomach with food contents” (Fig 1). Retained food was also seen in EGD, confirming delayed gastric emptying. He was given a course of fluconazole, and his PEth became negative. A few weeks after completing fluconazole, PEth was again detectable at low levels. The patient was extensively evaluated by the transplant psychosocial team and determined to have been truly abstinent since 2011. After another course of fluconazole, the PEth test became negative, supporting Candida-related fermentation as the cause. The CT scan showed a large Hepatocellular carcinoma (6 cm), and transplant evaluation with down-staging protocol was started. Unfortunately, his HCC progressed despite Loco-Regional therapy (Fig 2).
Discussion: Our patient clearly had ABS, evidenced by three negative PEth tests following three fluconazole treatments. Given the implications of detectable PEth for liver disease management and transplant eligibility, clinicians should recognize the potential for ABS. One unanswered question in our patient is whether endogenous alcohol production contributed to the progression of his cirrhosis despite the eradication of HCV 13 years ago. While progression of cirrhosis is possible despite eradication of HCV, his delayed decompensation may be attributed to the recent onset of ABS and endogenous alcohol.
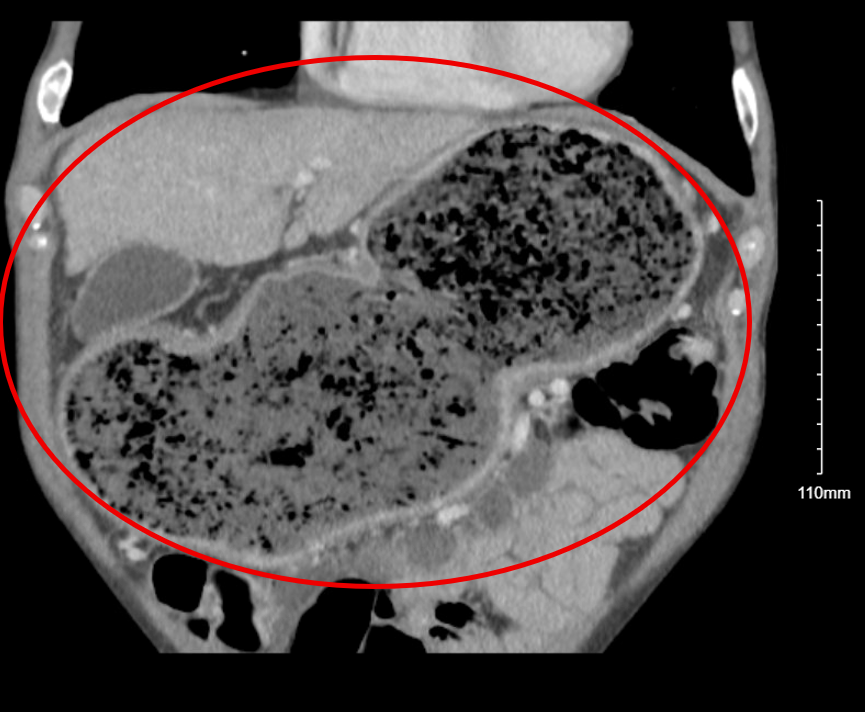
Figure: Fig 1. CT Scan of the abdomen. The coronal view shows a significantly dilated stomach (red circle).

Figure: Fig 2. CT Abdomen Triple Phase. The thin venous phase axial view shows numerous hypoenhancing nodules (red circle) throughout the right lobe of the liver, which is concerning for infiltrative HCC and indicative of progression of hepatocellular carcinoma.
Disclosures:
Jeff Angelo Taclob indicated no relevant financial relationships.
Lauren Lyssy indicated no relevant financial relationships.
Shehnaz Nansiyani indicated no relevant financial relationships.
Beth Ruiz indicated no relevant financial relationships.
Satheesh Nair indicated no relevant financial relationships.
Jeff Angelo Taclob, MD1, Lauren Lyssy, DO1, Shehnaz Nansiyani, FNP1, Beth Ruiz, PA-C1, Satheesh Nair, MD2. P3903 - A Curious Case of Auto-Brewery Syndrome in a Patient Undergoing Liver Transplant Evaluation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
