Monday Poster Session
Category: Liver
P3900 - Exploring the Liver-Heart Axis: Cirrhosis as a Complication of Hypertrophic Obstructive Cardiomyopathy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Daniel Alejandro Gonzalez Mosquera, MD (he/him/his)
NYC Health + Hospitals/Lincoln
Bronx, NY
Presenting Author(s)
Daniel Alejandro. Gonzalez Mosquera, MD, Mariana Nunes Ferreira, MD, Daniel Alejandro. Sittler, MD
NYC Health + Hospitals/Lincoln, Bronx, NY
Introduction: Cardiac cirrhosis, or congestive hepatopathy, results from chronic right-sided heart failure causing hepatic congestion and fibrosis. Transplant waitlist mortality ranges from 11% to 30%, yet post-transplant survival reaches ~80% at 1 year and 70% at 3 years. Hypertrophic Obstructive Cardiomyopathy (HOCM) is a rare but potential cause. We present a case of new-onset ascites in a young patient with HOCM.
Case Description/
Methods: A 33-year-old male with HOCM diagnosed 18 years ago, complicated by atrial fibrillation, presented to the Emergency Department with 2 months of abdominal pain, pericardial effusion, and massive ascites requiring paracentesis. Fluid analysis showed a SAAG >1.4, total protein of 8.0 g/dL, and albumin of 4.0 g/dL, indicating portal hypertension. In early February, he returned to the ED with severe abdominal pain (8.5/10) and persistent distension. POCUS showed moderate pericardial effusion and a large ascitic pocket. Abdominal ultrasound revealed liver nodularity consistent with cirrhosis.
Labs revealed macrocytosis, hyponatremia, positive ANA, and weakly positive anti-smooth muscle antibody, highly likely due to hepatic congestion.. A newly paracentesis revealed a SAAG of 1.1 g/dL and fluid protein of 2.5 g/dL, draining 3.5 liters. Additional liver workup was normal, including genetic and metabolic screening for HFE, Wilson’s disease, and alpha-1 antitrypsin. The hepatitis panel showed a resolved Hepatitis A infection. A contrast-enhanced CT scan ruled out Budd-Chiari syndrome. After excluding other diagnoses, the patient was discharged with a referral to an outside cardiology facility for further evaluation regarding potential cardiac transplant.
Three months later, outpatient liver biopsy confirmed cirrhosis with trichrome staining showing centrilobular sinusoidal dilatation and focal congestion, consistent with cirrhosis from HOCM. Due to progressive disease and morbidity, he was referred for combined heart-liver transplant (CHLT) evaluation.
Discussion: HOCM can lead to cardiac cirrhosis via diastolic dysfunction, increased cardiac pressures, and right-sided heart failure, resulting in congestive hepatopathy. The end-stage treatment is CHLT, with cardiac cirrhosis as one of the three main indications. Effective management requires an interprofessional team focused on both the underlying cardiac dysfunction and conventional liver cirrhosis care. Early recognition and comprehensive management of both heart-liver conditions are essential for improving patient outcomes.
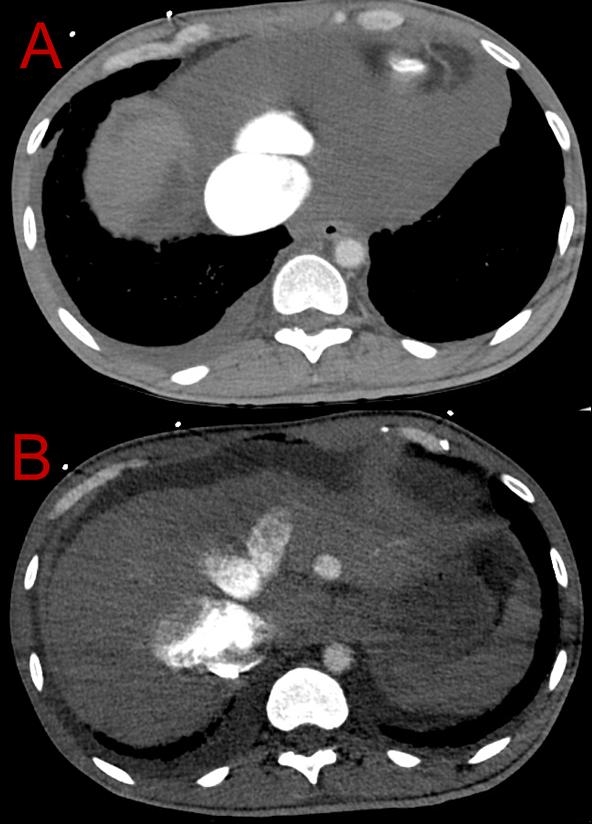
Figure: CT of the abdomen with contrast in the arterial phase. Fig. A: Reflux of contrast into a dilated IVC. Fig. B: Heterogeneous enhancement of the liver due to contrast reflux.
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Mariana Nunes Ferreira indicated no relevant financial relationships.
Daniel Sittler indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD, Mariana Nunes Ferreira, MD, Daniel Alejandro. Sittler, MD. P3900 - Exploring the Liver-Heart Axis: Cirrhosis as a Complication of Hypertrophic Obstructive Cardiomyopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NYC Health + Hospitals/Lincoln, Bronx, NY
Introduction: Cardiac cirrhosis, or congestive hepatopathy, results from chronic right-sided heart failure causing hepatic congestion and fibrosis. Transplant waitlist mortality ranges from 11% to 30%, yet post-transplant survival reaches ~80% at 1 year and 70% at 3 years. Hypertrophic Obstructive Cardiomyopathy (HOCM) is a rare but potential cause. We present a case of new-onset ascites in a young patient with HOCM.
Case Description/
Methods: A 33-year-old male with HOCM diagnosed 18 years ago, complicated by atrial fibrillation, presented to the Emergency Department with 2 months of abdominal pain, pericardial effusion, and massive ascites requiring paracentesis. Fluid analysis showed a SAAG >1.4, total protein of 8.0 g/dL, and albumin of 4.0 g/dL, indicating portal hypertension. In early February, he returned to the ED with severe abdominal pain (8.5/10) and persistent distension. POCUS showed moderate pericardial effusion and a large ascitic pocket. Abdominal ultrasound revealed liver nodularity consistent with cirrhosis.
Labs revealed macrocytosis, hyponatremia, positive ANA, and weakly positive anti-smooth muscle antibody, highly likely due to hepatic congestion.. A newly paracentesis revealed a SAAG of 1.1 g/dL and fluid protein of 2.5 g/dL, draining 3.5 liters. Additional liver workup was normal, including genetic and metabolic screening for HFE, Wilson’s disease, and alpha-1 antitrypsin. The hepatitis panel showed a resolved Hepatitis A infection. A contrast-enhanced CT scan ruled out Budd-Chiari syndrome. After excluding other diagnoses, the patient was discharged with a referral to an outside cardiology facility for further evaluation regarding potential cardiac transplant.
Three months later, outpatient liver biopsy confirmed cirrhosis with trichrome staining showing centrilobular sinusoidal dilatation and focal congestion, consistent with cirrhosis from HOCM. Due to progressive disease and morbidity, he was referred for combined heart-liver transplant (CHLT) evaluation.
Discussion: HOCM can lead to cardiac cirrhosis via diastolic dysfunction, increased cardiac pressures, and right-sided heart failure, resulting in congestive hepatopathy. The end-stage treatment is CHLT, with cardiac cirrhosis as one of the three main indications. Effective management requires an interprofessional team focused on both the underlying cardiac dysfunction and conventional liver cirrhosis care. Early recognition and comprehensive management of both heart-liver conditions are essential for improving patient outcomes.
Figure: CT of the abdomen with contrast in the arterial phase. Fig. A: Reflux of contrast into a dilated IVC. Fig. B: Heterogeneous enhancement of the liver due to contrast reflux.
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Mariana Nunes Ferreira indicated no relevant financial relationships.
Daniel Sittler indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD, Mariana Nunes Ferreira, MD, Daniel Alejandro. Sittler, MD. P3900 - Exploring the Liver-Heart Axis: Cirrhosis as a Complication of Hypertrophic Obstructive Cardiomyopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
