Monday Poster Session
Category: Liver
P3896 - A Familiar Pseudocyst in Unfamiliar Places: An Unusual Case of an Intrahepatic Pancreatic Pseudocyst
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nikolay Lifshaz, DO
HCA Healthcare
Overland Park, KS
Presenting Author(s)
Nikolay Lifshaz, DO1, Sanjana Sabesan, MD1, Idrees Siddiqui, DO2, Fadi Bdair, MD1
1HCA Healthcare, Overland Park, KS; 2Kansas City University, Overland Park, KS
Introduction: Intrahepatic Pancreatic Pseudocyst (IHPPs) is a rare variant of pancreatitis-induced pseudocyst formation extending into the liver, with fewer than 60 cases reported in literature. Given the atypical location and resemblance to other hepatic pathologies, IHPPs present a significant diagnostic conundrum. Here we present a unique case of a subcapsular intrahepatic pseudocyst.
Case Description/
Methods: A 59-year-old male presented to the hospital with two months of ongoing upper abdominal pain, decreased appetite and shortness of breath. His medical history is significant for G6PD deficiency, chronic alcohol use and previous peripancreatic pseudocyst drainage. On physical exam, he had diffusely tender abdominal distension. Labs were remarkable for Lipase of 597 U/L, normal LFTs. Infectious workup was negative. CT of abdomen and pelvis showed acute pancreatitis with multiple thick walled collections across the abdomen, including a discrete subcapsular hepatic fluid collection measuring 10 cm across, and a perigastric collection measuring 6.8 x 6.4 cm. Pseudocyst drainage was performed with upper endoscopic ultrasound fine needle aspiration and cystogastrostomy with AXIOS stent placement. Lab analysis of pseudocyst aspirate showed elevated lipase >5000 U/L and amylase >6500 U/L. Aspirate cytology revealed scant squamous cells and macrophages without malignant cells, consistent with tissue inflammation in the setting of pancreatic fluid exposure. Patient was ultimately discharged after interval decrease in size of perigastric fluid collections was demonstrated on follow-up imaging. (Figure A&B)
Discussion: Formation of IHPPs has been proposed to result from either leakage of pancreatic fluid along the gastrohepatic ligament into the left liver lobe or along the hepatoduodenal ligament directly into the liver parenchyma.1 These cysts are frequently misdiagnosed as abscesses or cystic tumors due to their unusual location and non-specific imaging features. Our case underscores the importance of including IHPP in the differential diagnosis of atypical hepatic cystic lesions, especially in patients with known or suspected history of pancreatitis. Prompt recognition and appropriate non-surgical management can lead to favorable outcomes and prevent invasive procedures.
References
Tomar S, Ghasi RG, Agarwal J. “Multiple intrahepatic pancreatic pseudocyst (MIHPPs): an overlooked and misdiagnosed entity”. Gastroenterol Hepatol Bed Bench. 2019 Summer;12(3):263-266. PMID: 31528312

Figure: A) Axial Plan Abdominal CT demonstrating septated subcapsular and perigastric pseudocyst
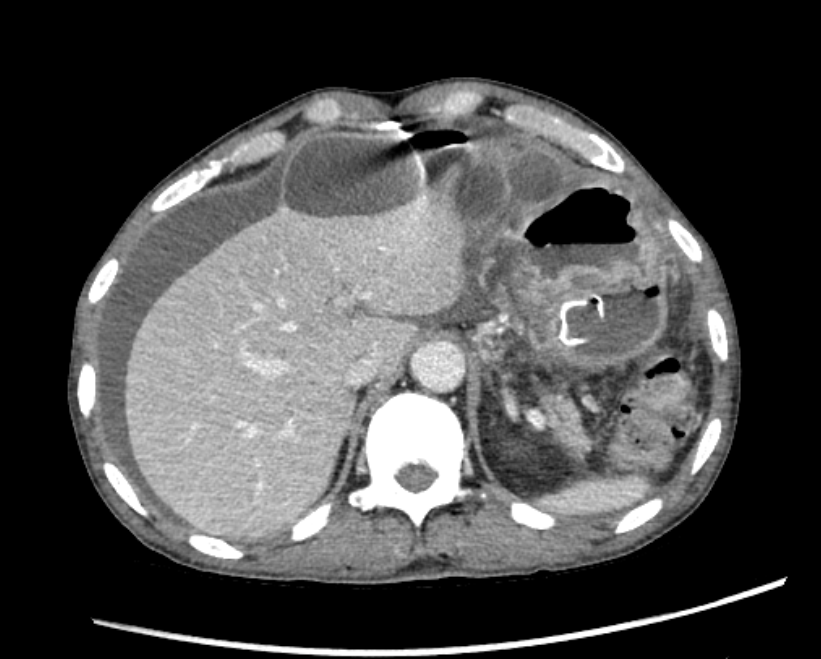
Figure: B) Axial Plan Abdominal CT demonstrating reduction of perigastric pseudocyst after AXIOS stenting
Disclosures:
Nikolay Lifshaz indicated no relevant financial relationships.
Sanjana Sabesan indicated no relevant financial relationships.
Idrees Siddiqui indicated no relevant financial relationships.
Fadi Bdair indicated no relevant financial relationships.
Nikolay Lifshaz, DO1, Sanjana Sabesan, MD1, Idrees Siddiqui, DO2, Fadi Bdair, MD1. P3896 - A Familiar Pseudocyst in Unfamiliar Places: An Unusual Case of an Intrahepatic Pancreatic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare, Overland Park, KS; 2Kansas City University, Overland Park, KS
Introduction: Intrahepatic Pancreatic Pseudocyst (IHPPs) is a rare variant of pancreatitis-induced pseudocyst formation extending into the liver, with fewer than 60 cases reported in literature. Given the atypical location and resemblance to other hepatic pathologies, IHPPs present a significant diagnostic conundrum. Here we present a unique case of a subcapsular intrahepatic pseudocyst.
Case Description/
Methods: A 59-year-old male presented to the hospital with two months of ongoing upper abdominal pain, decreased appetite and shortness of breath. His medical history is significant for G6PD deficiency, chronic alcohol use and previous peripancreatic pseudocyst drainage. On physical exam, he had diffusely tender abdominal distension. Labs were remarkable for Lipase of 597 U/L, normal LFTs. Infectious workup was negative. CT of abdomen and pelvis showed acute pancreatitis with multiple thick walled collections across the abdomen, including a discrete subcapsular hepatic fluid collection measuring 10 cm across, and a perigastric collection measuring 6.8 x 6.4 cm. Pseudocyst drainage was performed with upper endoscopic ultrasound fine needle aspiration and cystogastrostomy with AXIOS stent placement. Lab analysis of pseudocyst aspirate showed elevated lipase >5000 U/L and amylase >6500 U/L. Aspirate cytology revealed scant squamous cells and macrophages without malignant cells, consistent with tissue inflammation in the setting of pancreatic fluid exposure. Patient was ultimately discharged after interval decrease in size of perigastric fluid collections was demonstrated on follow-up imaging. (Figure A&B)
Discussion: Formation of IHPPs has been proposed to result from either leakage of pancreatic fluid along the gastrohepatic ligament into the left liver lobe or along the hepatoduodenal ligament directly into the liver parenchyma.1 These cysts are frequently misdiagnosed as abscesses or cystic tumors due to their unusual location and non-specific imaging features. Our case underscores the importance of including IHPP in the differential diagnosis of atypical hepatic cystic lesions, especially in patients with known or suspected history of pancreatitis. Prompt recognition and appropriate non-surgical management can lead to favorable outcomes and prevent invasive procedures.
References
Tomar S, Ghasi RG, Agarwal J. “Multiple intrahepatic pancreatic pseudocyst (MIHPPs): an overlooked and misdiagnosed entity”. Gastroenterol Hepatol Bed Bench. 2019 Summer;12(3):263-266. PMID: 31528312

Figure: A) Axial Plan Abdominal CT demonstrating septated subcapsular and perigastric pseudocyst
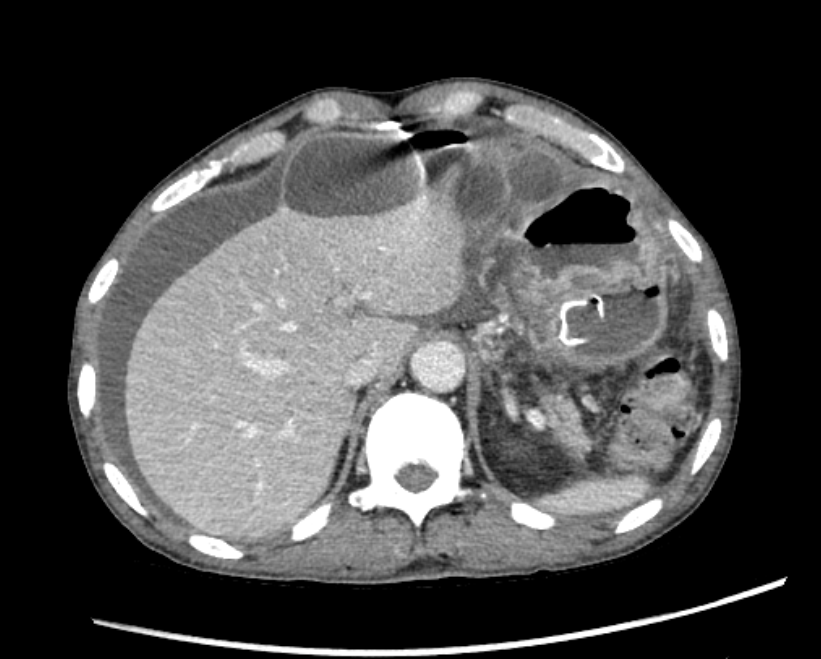
Figure: B) Axial Plan Abdominal CT demonstrating reduction of perigastric pseudocyst after AXIOS stenting
Disclosures:
Nikolay Lifshaz indicated no relevant financial relationships.
Sanjana Sabesan indicated no relevant financial relationships.
Idrees Siddiqui indicated no relevant financial relationships.
Fadi Bdair indicated no relevant financial relationships.
Nikolay Lifshaz, DO1, Sanjana Sabesan, MD1, Idrees Siddiqui, DO2, Fadi Bdair, MD1. P3896 - A Familiar Pseudocyst in Unfamiliar Places: An Unusual Case of an Intrahepatic Pancreatic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
