Monday Poster Session
Category: Liver
The Great Pretender: A <i>Gemella morbillorum</i> and <i>Streptococcus constellatus</i> Liver Abscess That Faked a Tumor
P3881 - The Great Pretender: A Gemella morbillorum and Streptococcus constellatus Liver Abscess That Faked a Tumor
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Mariam Nikolaishvili, MD
Ascension Saint Francis Hospital
Evanston, IL
Presenting Author(s)
Mariam Nikolaishvili, MD1, Aleksandre Asatiani, MD2, Parya Rahimi, MD3, Abhi K. Singh, MD4, Tasneem Anagreh, MD1, Jeongsoo Yoon, MD1, Khaled Al Khodari, MD1, Bhargav Koyani, MD1, Muhammad Ahsan. Siddiqui, MD1
1Ascension Saint Francis Hospital, Evanston, IL; 2David Tvildiani Medical University, Evanston, IL; 3Ascension Saint Francis Hospital, Chicago, IL; 4St. Francis Hospital, Evanston, IL
Introduction: Pyogenic liver abscesses (PLAs) are rare but potentially fatal, with an incidence of 2.3 per 100,000 in the U.S. and a 30-day mortality rate up to 27%. Most PLAs are caused by enteric pathogens such as Klebsiella pneumoniae, E. coli, and anaerobes. Infections due to uncommon organisms like Gemella morbillorum and the Streptococcus anginosus group are exceedingly rare and diagnostically challenging, particularly when radiographic findings mimic malignancy or gastrointestinal perforation.
Case Description/
Methods: We report a case of a 60-year-old Hispanic male with no significant medical history presented with four days of severe epigastric pain, intractable emesis, and oral intolerance. Initially hemodynamically stable, he progressed to septic shock with multiorgan failure. Labs revealed leukocytosis, acute kidney injury (Cr 3.43), severe transaminitis (AST/ALT 580/251), and high anion gap metabolic acidosis (pH 7.01, lactate 14.7). Non-contrast CT abdomen showed a heterogeneous hepatic mass with trace ascites and omental nodularity, raising concern for peritoneal carcinomatosis.
Hours later, due to clinical deterioration, repeat CT with IV contrast demonstrated portal venous gas, pneumoperitoneum, and gastric wall air—suggesting possible gastric perforation. Emergent laparotomy revealed a ruptured hepatic abscess, with no bowel perforation.
Cultures from blood and hepatic abscess grew Gemella morbillorum, Streptococcus constellatus, and Streptococcus anginosus. Despite broad-spectrum antibiotics, surgical drainage, and ICU support, the patient developed refractory septic shock, cardiomyopathy (EF 30%), and renal failure, ultimately leading to fatal outcome.
Discussion: This case highlights how hepatic abscesses due to atypical organisms can mimic malignancy on initial imaging, particularly when contrast is not used. G. morbillorum, a commensal of the oropharynx and GI tract, can cause life-threatening infections. The initial non-contrast CT led to misdiagnosis and delayed source control. In patients with systemic inflammation and hepatic lesions, contrast-enhanced imaging should be the preferred modality, as it can reveal key features such as rim enhancement, portal venous gas, and abscess formation. Early contrast administration can facilitate timely diagnosis, appropriate intervention, and may reduce mortality in rapidly progressive infections such as PLA. Further research is needed to optimize imaging strategies, identify risk factors, and improve diagnostic tools for atypical presentations.
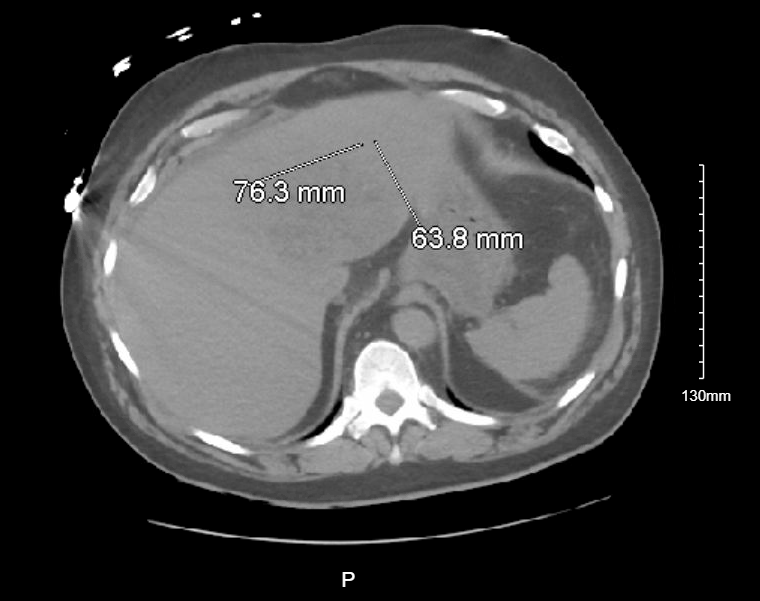
Figure: CTAP wo contrast
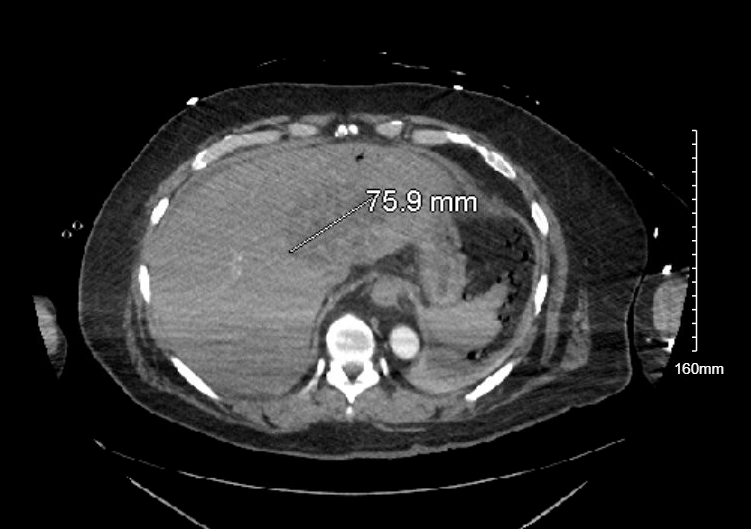
Figure: CTAP w IV contrast
Disclosures:
Mariam Nikolaishvili indicated no relevant financial relationships.
Aleksandre Asatiani indicated no relevant financial relationships.
Parya Rahimi indicated no relevant financial relationships.
Abhi Singh indicated no relevant financial relationships.
Tasneem Anagreh indicated no relevant financial relationships.
Jeongsoo Yoon indicated no relevant financial relationships.
Khaled Al Khodari indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Muhammad Siddiqui indicated no relevant financial relationships.
Mariam Nikolaishvili, MD1, Aleksandre Asatiani, MD2, Parya Rahimi, MD3, Abhi K. Singh, MD4, Tasneem Anagreh, MD1, Jeongsoo Yoon, MD1, Khaled Al Khodari, MD1, Bhargav Koyani, MD1, Muhammad Ahsan. Siddiqui, MD1. P3881 - The Great Pretender: A <i>Gemella morbillorum</i> and <i>Streptococcus constellatus</i> Liver Abscess That Faked a Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ascension Saint Francis Hospital, Evanston, IL; 2David Tvildiani Medical University, Evanston, IL; 3Ascension Saint Francis Hospital, Chicago, IL; 4St. Francis Hospital, Evanston, IL
Introduction: Pyogenic liver abscesses (PLAs) are rare but potentially fatal, with an incidence of 2.3 per 100,000 in the U.S. and a 30-day mortality rate up to 27%. Most PLAs are caused by enteric pathogens such as Klebsiella pneumoniae, E. coli, and anaerobes. Infections due to uncommon organisms like Gemella morbillorum and the Streptococcus anginosus group are exceedingly rare and diagnostically challenging, particularly when radiographic findings mimic malignancy or gastrointestinal perforation.
Case Description/
Methods: We report a case of a 60-year-old Hispanic male with no significant medical history presented with four days of severe epigastric pain, intractable emesis, and oral intolerance. Initially hemodynamically stable, he progressed to septic shock with multiorgan failure. Labs revealed leukocytosis, acute kidney injury (Cr 3.43), severe transaminitis (AST/ALT 580/251), and high anion gap metabolic acidosis (pH 7.01, lactate 14.7). Non-contrast CT abdomen showed a heterogeneous hepatic mass with trace ascites and omental nodularity, raising concern for peritoneal carcinomatosis.
Hours later, due to clinical deterioration, repeat CT with IV contrast demonstrated portal venous gas, pneumoperitoneum, and gastric wall air—suggesting possible gastric perforation. Emergent laparotomy revealed a ruptured hepatic abscess, with no bowel perforation.
Cultures from blood and hepatic abscess grew Gemella morbillorum, Streptococcus constellatus, and Streptococcus anginosus. Despite broad-spectrum antibiotics, surgical drainage, and ICU support, the patient developed refractory septic shock, cardiomyopathy (EF 30%), and renal failure, ultimately leading to fatal outcome.
Discussion: This case highlights how hepatic abscesses due to atypical organisms can mimic malignancy on initial imaging, particularly when contrast is not used. G. morbillorum, a commensal of the oropharynx and GI tract, can cause life-threatening infections. The initial non-contrast CT led to misdiagnosis and delayed source control. In patients with systemic inflammation and hepatic lesions, contrast-enhanced imaging should be the preferred modality, as it can reveal key features such as rim enhancement, portal venous gas, and abscess formation. Early contrast administration can facilitate timely diagnosis, appropriate intervention, and may reduce mortality in rapidly progressive infections such as PLA. Further research is needed to optimize imaging strategies, identify risk factors, and improve diagnostic tools for atypical presentations.
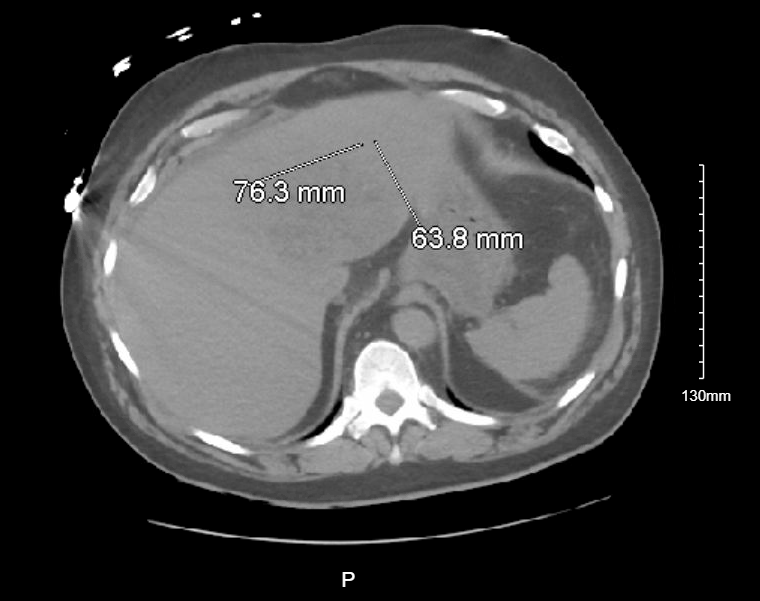
Figure: CTAP wo contrast
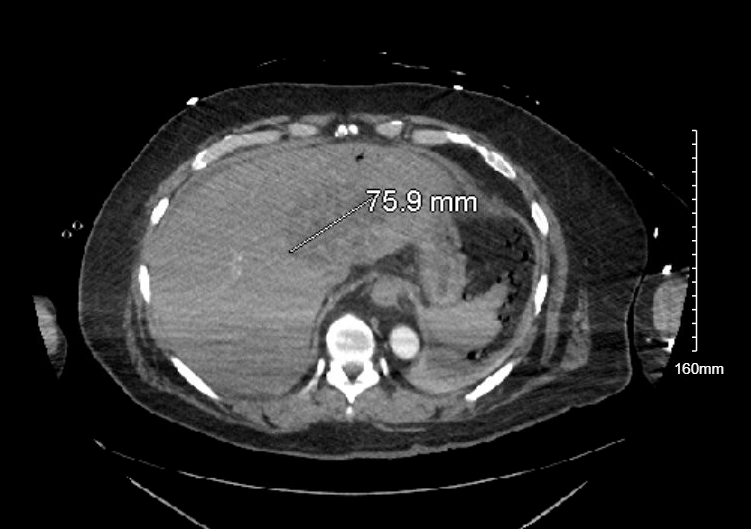
Figure: CTAP w IV contrast
Disclosures:
Mariam Nikolaishvili indicated no relevant financial relationships.
Aleksandre Asatiani indicated no relevant financial relationships.
Parya Rahimi indicated no relevant financial relationships.
Abhi Singh indicated no relevant financial relationships.
Tasneem Anagreh indicated no relevant financial relationships.
Jeongsoo Yoon indicated no relevant financial relationships.
Khaled Al Khodari indicated no relevant financial relationships.
Bhargav Koyani indicated no relevant financial relationships.
Muhammad Siddiqui indicated no relevant financial relationships.
Mariam Nikolaishvili, MD1, Aleksandre Asatiani, MD2, Parya Rahimi, MD3, Abhi K. Singh, MD4, Tasneem Anagreh, MD1, Jeongsoo Yoon, MD1, Khaled Al Khodari, MD1, Bhargav Koyani, MD1, Muhammad Ahsan. Siddiqui, MD1. P3881 - The Great Pretender: A <i>Gemella morbillorum</i> and <i>Streptococcus constellatus</i> Liver Abscess That Faked a Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

