Monday Poster Session
Category: Liver
P3880 - Liver Let Die: A Malignant Budd-Chiari Crisis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sabri Elmansouri, MD, MPH
Insight Hospital & Medical Center
Chicago, IL
Presenting Author(s)
Ahmed Abbas Farooqui, MD, Sabri Elmansouri, MD, MPH, Shafaq Taj, MD, Syed Samad, MD, Sharif Murphy, MD
Insight Hospital & Medical Center, Chicago, IL
Introduction: Budd-Chiari syndrome (BCS) is a rare condition caused by hepatic venous outflow obstruction, classified as primary (intrinsic venous thrombosis) or secondary (external compression or invasion by malignancy or other pathology). Clinical presentation varies from subacute ascites to fulminant hepatic failure, making early diagnosis essential. This case highlights rapidly progressive secondary BCS in a patient with untreated hepatitis C virus (HCV), cirrhosis, and malignancy, complicated by hepatic infarction, hemorrhagic ascites, and multi-organ failure.
Case Description/
Methods: A 71-year-old female with hypertension, untreated HCV, and a history of non-small cell lung cancer (status post left upper lobectomy in 2019), presented with 5 days of abdominal pain and distension. She met criteria for sepsis and was treated with intravenous fluids and broad-spectrum antibiotics (vancomycin and piperacillin-tazobactam). Labs showed a white blood cell count of 33.4 ×10⁹/L, platelet count 158 ×10⁹/L, international normalized ratio (INR) 5.3, total bilirubin 5.1 mg/dL, alanine aminotransferase 133 U/L, aspartate aminotransferase 269 U/L, albumin 2.5 g/dL, and lactic acid 6.0 mmol/L. Computed tomography (CT) of the abdomen and pelvis (AP) demonstrated cirrhotic-type colopathy, abnormal liver architecture, and pulmonary nodules suspicious for metastases. Blood and urine cultures showed no growth. Despite IV vitamin K and antibiotics, INR and lactic acid worsened to 7.1 and 9.9 mmol/L respectively. Ultrasound showed a cirrhotic liver with reversed (hepato-fugal) portal venous flow. CT angiography revealed thrombus in the hepatic veins and hypoattenuation of the liver concerning for infarction. Fresh frozen plasma was perfused, leading to improvement in INR to 3.1. The patient was transferred to a tertiary center for trans-jugular intrahepatic portosystemic shunt (TIPS) placement, inferior vena cava venography (further confirming BCS), and mechanical thrombectomy. Paracentesis yielded 1,700 mL of bloody ascitic fluid with malignant cells. She developed refractory septic and hypovolemic shock and passed away following transition to comfort care.
Discussion: This case highlights the rapid progression and high mortality associated with secondary BCS in patients with underlying malignancy and chronic liver disease. Findings such as hepatofugal flow and hepatic infarction warrant urgent hepatology and interventional radiology involvement. Despite timely intervention, prognosis remains poor in advanced disease.
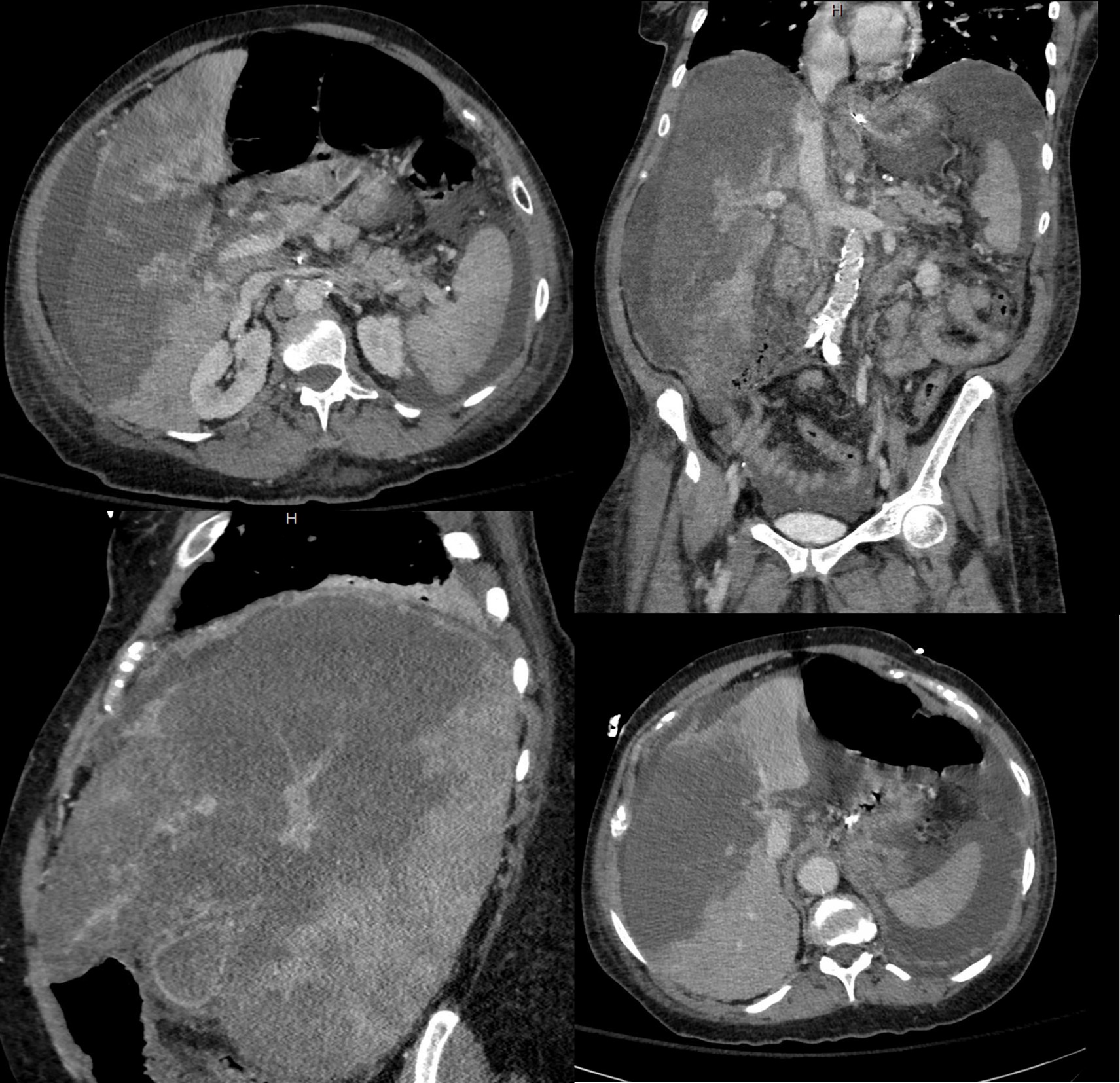
Figure: CT AP (venous phase): extensive thrombi in the hepatic veins and large hepatic infarct
Disclosures:
Ahmed Abbas Farooqui indicated no relevant financial relationships.
Sabri Elmansouri indicated no relevant financial relationships.
Shafaq Taj indicated no relevant financial relationships.
Syed Samad indicated no relevant financial relationships.
Sharif Murphy indicated no relevant financial relationships.
Ahmed Abbas Farooqui, MD, Sabri Elmansouri, MD, MPH, Shafaq Taj, MD, Syed Samad, MD, Sharif Murphy, MD. P3880 - Liver Let Die: A Malignant Budd-Chiari Crisis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Insight Hospital & Medical Center, Chicago, IL
Introduction: Budd-Chiari syndrome (BCS) is a rare condition caused by hepatic venous outflow obstruction, classified as primary (intrinsic venous thrombosis) or secondary (external compression or invasion by malignancy or other pathology). Clinical presentation varies from subacute ascites to fulminant hepatic failure, making early diagnosis essential. This case highlights rapidly progressive secondary BCS in a patient with untreated hepatitis C virus (HCV), cirrhosis, and malignancy, complicated by hepatic infarction, hemorrhagic ascites, and multi-organ failure.
Case Description/
Methods: A 71-year-old female with hypertension, untreated HCV, and a history of non-small cell lung cancer (status post left upper lobectomy in 2019), presented with 5 days of abdominal pain and distension. She met criteria for sepsis and was treated with intravenous fluids and broad-spectrum antibiotics (vancomycin and piperacillin-tazobactam). Labs showed a white blood cell count of 33.4 ×10⁹/L, platelet count 158 ×10⁹/L, international normalized ratio (INR) 5.3, total bilirubin 5.1 mg/dL, alanine aminotransferase 133 U/L, aspartate aminotransferase 269 U/L, albumin 2.5 g/dL, and lactic acid 6.0 mmol/L. Computed tomography (CT) of the abdomen and pelvis (AP) demonstrated cirrhotic-type colopathy, abnormal liver architecture, and pulmonary nodules suspicious for metastases. Blood and urine cultures showed no growth. Despite IV vitamin K and antibiotics, INR and lactic acid worsened to 7.1 and 9.9 mmol/L respectively. Ultrasound showed a cirrhotic liver with reversed (hepato-fugal) portal venous flow. CT angiography revealed thrombus in the hepatic veins and hypoattenuation of the liver concerning for infarction. Fresh frozen plasma was perfused, leading to improvement in INR to 3.1. The patient was transferred to a tertiary center for trans-jugular intrahepatic portosystemic shunt (TIPS) placement, inferior vena cava venography (further confirming BCS), and mechanical thrombectomy. Paracentesis yielded 1,700 mL of bloody ascitic fluid with malignant cells. She developed refractory septic and hypovolemic shock and passed away following transition to comfort care.
Discussion: This case highlights the rapid progression and high mortality associated with secondary BCS in patients with underlying malignancy and chronic liver disease. Findings such as hepatofugal flow and hepatic infarction warrant urgent hepatology and interventional radiology involvement. Despite timely intervention, prognosis remains poor in advanced disease.
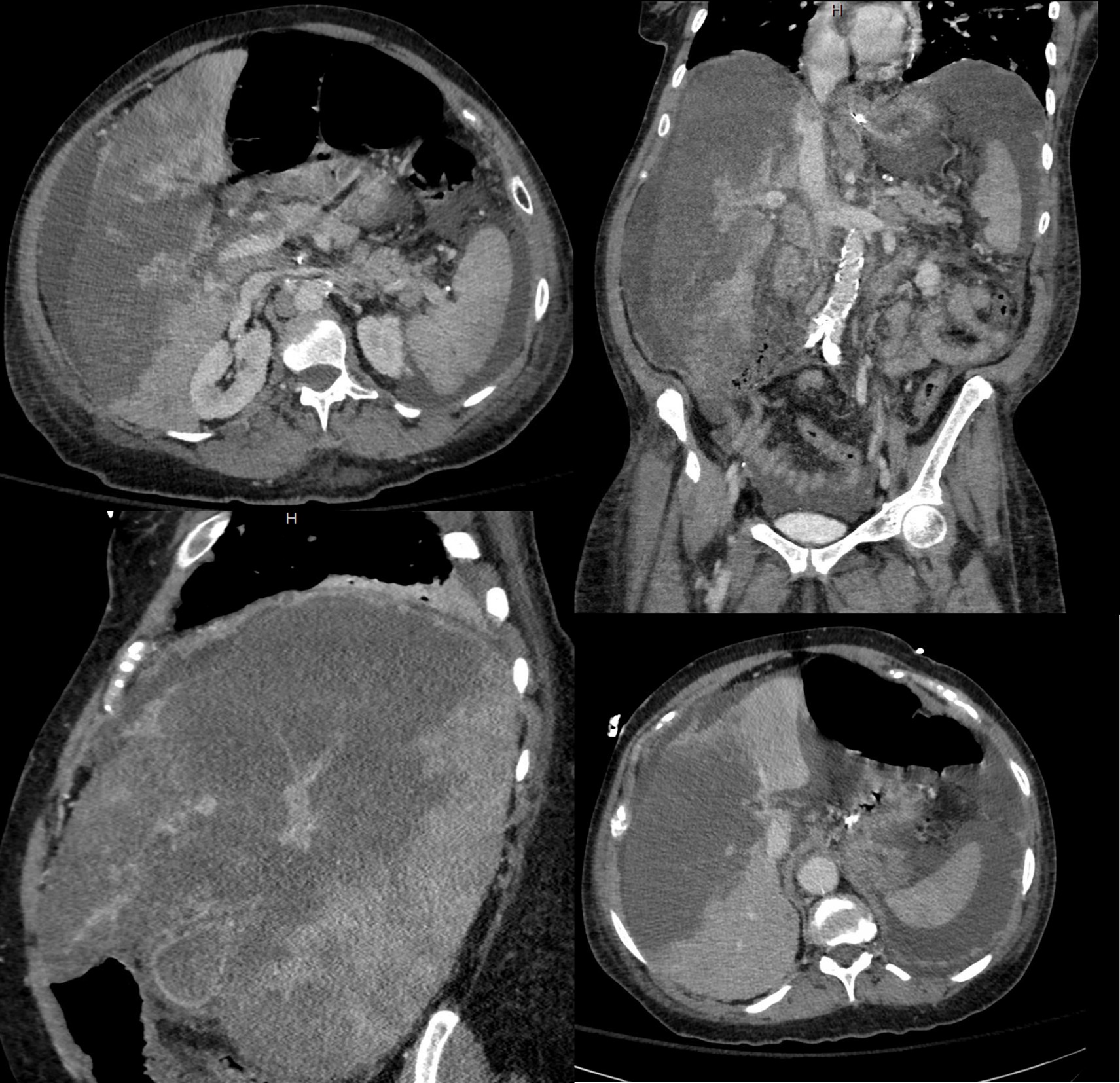
Figure: CT AP (venous phase): extensive thrombi in the hepatic veins and large hepatic infarct
Disclosures:
Ahmed Abbas Farooqui indicated no relevant financial relationships.
Sabri Elmansouri indicated no relevant financial relationships.
Shafaq Taj indicated no relevant financial relationships.
Syed Samad indicated no relevant financial relationships.
Sharif Murphy indicated no relevant financial relationships.
Ahmed Abbas Farooqui, MD, Sabri Elmansouri, MD, MPH, Shafaq Taj, MD, Syed Samad, MD, Sharif Murphy, MD. P3880 - Liver Let Die: A Malignant Budd-Chiari Crisis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
