Monday Poster Session
Category: Liver
P3853 - Rare Case of Cholestatic Stauffer’s Syndrome in the Setting of Prostate Cancer
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Israa M. Jahan, BS
Creighton University School of Medicine
Gilbert, AZ
Presenting Author(s)
Israa M. Jahan, BS1, Ericka Charley, MD2, Vikash Kumar, MD3, Dalbir Sandhu, MD3, Justin Reynolds, MD3, Aida Rezaie, MD3
1Creighton University School of Medicine, Gilbert, AZ; 2Creighton University School of Medicine, Mesa, AZ; 3Creighton University School of Medicine, Phoenix, AZ
Introduction: Stauffer’s syndrome is a rare paraneoplastic syndrome that is seen primarily with renal cell carcinoma but can also occur with prostate cancer and soft tissue sarcomas. It presents as liver dysfunction with abnormal liver function tests including elevated alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine transaminase (ALT), and prothrombin times (1). Cholestatic jaundice is a rare sequela, as there is no overt blockage of hepatic or bile ducts. In this case report, we discuss a prostate cancer patient who presented with jaundice secondary to Stauffer’s syndrome.
Case Description/
Methods: A 70-year-old male presented with jaundice. Labs showed total bilirubin of 24 mg/dL, ALT 73 U/L, AST 97 U/L, ALP 1255 U/L, and elevated ammonia at 38. Liver ultrasound showed no intrahepatic biliary ductal dilation or mass, and biopsy revealed severe cholestatic hepatitis. Computed tomography (CT) was notable for aortocaval and parailiac lymphadenopathy, severely enlarged prostate, and scattered sclerotic lesions (see Figure 1). PSA levels were over 5000. Biopsy of a lymph node was characterized by atypical nuclei and positive NKX3.1, CAM5.2, and MOC31, confirming prostatic adenocarcinoma. Lupron was initiated, but other antiandrogens were avoided due to risk of further liver injury. After Lupron, bilirubin decreased from 24 to 19 and PSA levels dropped from 5000 to 3200 in two weeks.
Discussion: Stauffer’s syndrome is an uncommon hepatic paraneoplastic syndrome seen in prostatic cancer. This patient presented with elevated transaminases, suggestive of a non-cholestatic form; however, bilirubin elevation and jaundice suggest the rarer cholestatic version. Jaundice is unusual in prostate cancer due to lack of overt duct obstruction. Inflammatory markers such as IL-6 secreted by the neoplasm are hypothesized to cause this liver injury. These markers may also inhibit the expression of hepatobiliary transporter genes, impairing biliary flow (1).
Though the exact cause remains unclear, treatment of the primary tumor resolves the liver abnormalities (1). In this case, Lupron effectively treated the cancer as shown by the downtrend in PSA and bilirubin levels. Recognizing cholestasis as a presentation of Stauffer’s syndrome may help identify and treat the tumor.
Works Cited
1. Kim YH, Park JM, Kang CD, Seo SO, Lee K, Song G. Prostate cancer presenting with pruritus and cholestasis. The Korean Journal of Gastroenterology. 2021;78(1):59-64. doi:10.4166/kjg.2021.059
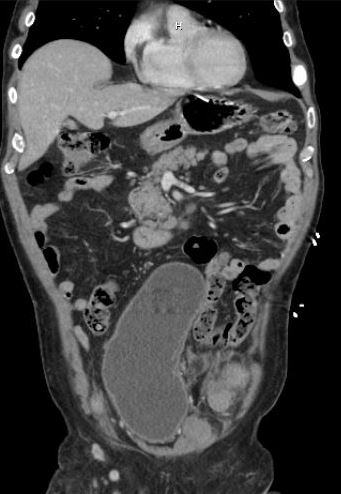
Figure: Figure 1. CT shows enlarged prostate, parailiac and aortocaval lymphadenopathy, hepatomegaly with no obstruction, and sclerotic lesions in the pelvis
Disclosures:
Israa Jahan indicated no relevant financial relationships.
Ericka Charley indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Justin Reynolds indicated no relevant financial relationships.
Aida Rezaie indicated no relevant financial relationships.
Israa M. Jahan, BS1, Ericka Charley, MD2, Vikash Kumar, MD3, Dalbir Sandhu, MD3, Justin Reynolds, MD3, Aida Rezaie, MD3. P3853 - Rare Case of Cholestatic Stauffer’s Syndrome in the Setting of Prostate Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Gilbert, AZ; 2Creighton University School of Medicine, Mesa, AZ; 3Creighton University School of Medicine, Phoenix, AZ
Introduction: Stauffer’s syndrome is a rare paraneoplastic syndrome that is seen primarily with renal cell carcinoma but can also occur with prostate cancer and soft tissue sarcomas. It presents as liver dysfunction with abnormal liver function tests including elevated alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine transaminase (ALT), and prothrombin times (1). Cholestatic jaundice is a rare sequela, as there is no overt blockage of hepatic or bile ducts. In this case report, we discuss a prostate cancer patient who presented with jaundice secondary to Stauffer’s syndrome.
Case Description/
Methods: A 70-year-old male presented with jaundice. Labs showed total bilirubin of 24 mg/dL, ALT 73 U/L, AST 97 U/L, ALP 1255 U/L, and elevated ammonia at 38. Liver ultrasound showed no intrahepatic biliary ductal dilation or mass, and biopsy revealed severe cholestatic hepatitis. Computed tomography (CT) was notable for aortocaval and parailiac lymphadenopathy, severely enlarged prostate, and scattered sclerotic lesions (see Figure 1). PSA levels were over 5000. Biopsy of a lymph node was characterized by atypical nuclei and positive NKX3.1, CAM5.2, and MOC31, confirming prostatic adenocarcinoma. Lupron was initiated, but other antiandrogens were avoided due to risk of further liver injury. After Lupron, bilirubin decreased from 24 to 19 and PSA levels dropped from 5000 to 3200 in two weeks.
Discussion: Stauffer’s syndrome is an uncommon hepatic paraneoplastic syndrome seen in prostatic cancer. This patient presented with elevated transaminases, suggestive of a non-cholestatic form; however, bilirubin elevation and jaundice suggest the rarer cholestatic version. Jaundice is unusual in prostate cancer due to lack of overt duct obstruction. Inflammatory markers such as IL-6 secreted by the neoplasm are hypothesized to cause this liver injury. These markers may also inhibit the expression of hepatobiliary transporter genes, impairing biliary flow (1).
Though the exact cause remains unclear, treatment of the primary tumor resolves the liver abnormalities (1). In this case, Lupron effectively treated the cancer as shown by the downtrend in PSA and bilirubin levels. Recognizing cholestasis as a presentation of Stauffer’s syndrome may help identify and treat the tumor.
Works Cited
1. Kim YH, Park JM, Kang CD, Seo SO, Lee K, Song G. Prostate cancer presenting with pruritus and cholestasis. The Korean Journal of Gastroenterology. 2021;78(1):59-64. doi:10.4166/kjg.2021.059
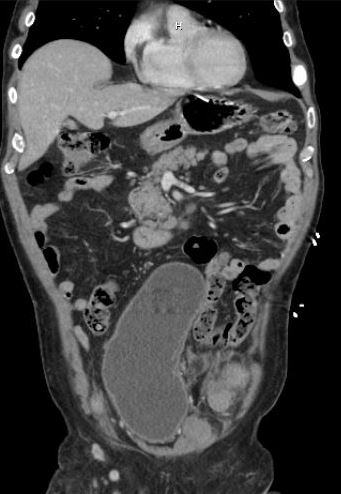
Figure: Figure 1. CT shows enlarged prostate, parailiac and aortocaval lymphadenopathy, hepatomegaly with no obstruction, and sclerotic lesions in the pelvis
Disclosures:
Israa Jahan indicated no relevant financial relationships.
Ericka Charley indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Justin Reynolds indicated no relevant financial relationships.
Aida Rezaie indicated no relevant financial relationships.
Israa M. Jahan, BS1, Ericka Charley, MD2, Vikash Kumar, MD3, Dalbir Sandhu, MD3, Justin Reynolds, MD3, Aida Rezaie, MD3. P3853 - Rare Case of Cholestatic Stauffer’s Syndrome in the Setting of Prostate Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

