Monday Poster Session
Category: Liver
P3846 - When Cirrhosis Isn't the Only Culprit: Recognizing ITP in Severe Thrombocytopenia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- ME
Mohamad Elgozair, MD
Danbury / Yale New Haven Hospital
Danbury, CT
Presenting Author(s)
Mohamad Elgozair, MD1, Mohammed Y. Youssef, MD2, Resham Ramkissoon, MD3, Lewis Roberts, MBChB, PhD3
1Danbury / Yale New Haven Hospital, Danbury, CT; 2Hunt Regional Medical Center, Greenville, TX; 3Mayo Clinic, Rochester, MN
Introduction: Thrombocytopenia, defined as a platelet count below 150,000/µL, is common in advanced chronic liver disease and is associated with increased mortality. Its pathophysiology is multifactorial, involving splenic sequestration, reduced thrombopoietin production, and immune-mediated platelet destruction. In cirrhosis, an acute, severe drop in platelet count should warrant investigation for secondary causes, including infection, malignancy, autoimmunity, medications, or marrow suppression. We present a case of cirrhosis complicated by profound thrombocytopenia due to immune thrombocytopenic purpura (ITP) and alcohol-induced bone marrow suppression.
Case Description/
Methods: A 51-year-old Caucasian woman with alcohol and opioid use disorders, untreated Helicobacter pylori infection, and cirrhosis with portal hypertension presented with nausea, vomiting, tremors, and diaphoresis, consistent with alcohol withdrawal. She had resumed drinking weeks earlier, after sobriety, but stopped four days before admission. On examination, she was jaundiced, lethargic, and encephalopathic. Vitals: HR 113 bpm, RR 30/min. Abdominal exam showed tender hepatomegaly. Labs revealed platelets 17 × 10⁹/L [baseline 60 × 10⁹/L], WBC 1.4 × 10⁹/L, bilirubin 10.2 mg/dL, AST 183 U/L, ammonia 111 µmol/L, hypokalemia, and hypomagnesemia. Imaging showed cirrhotic liver and splenomegaly (15.3 cm) with no thrombosis. Given the severe thrombocytopenia and untreated H. pylori, ITP was suspected. Positive antiplatelet antibodies confirmed the diagnosis. The patient was treated with lorazepam, thiamine, folate, rifaximin, electrolytes, and prednisone 40 mg daily with taper. Platelet counts improved significantly.
Discussion: While thrombocytopenia in cirrhosis is typically attributed to portal hypertension and thrombopoietin deficiency, the abrupt and severe decline in this case suggested an additional process. Alcohol use likely contributed to bone marrow suppression, but the presence of untreated H. pylori and positive antiplatelet antibodies pointed to ITP. H. pylori is an established rare trigger for ITP, potentially through molecular mimicry and immune activation. Identifying and managing such triggers is key in selected patients.
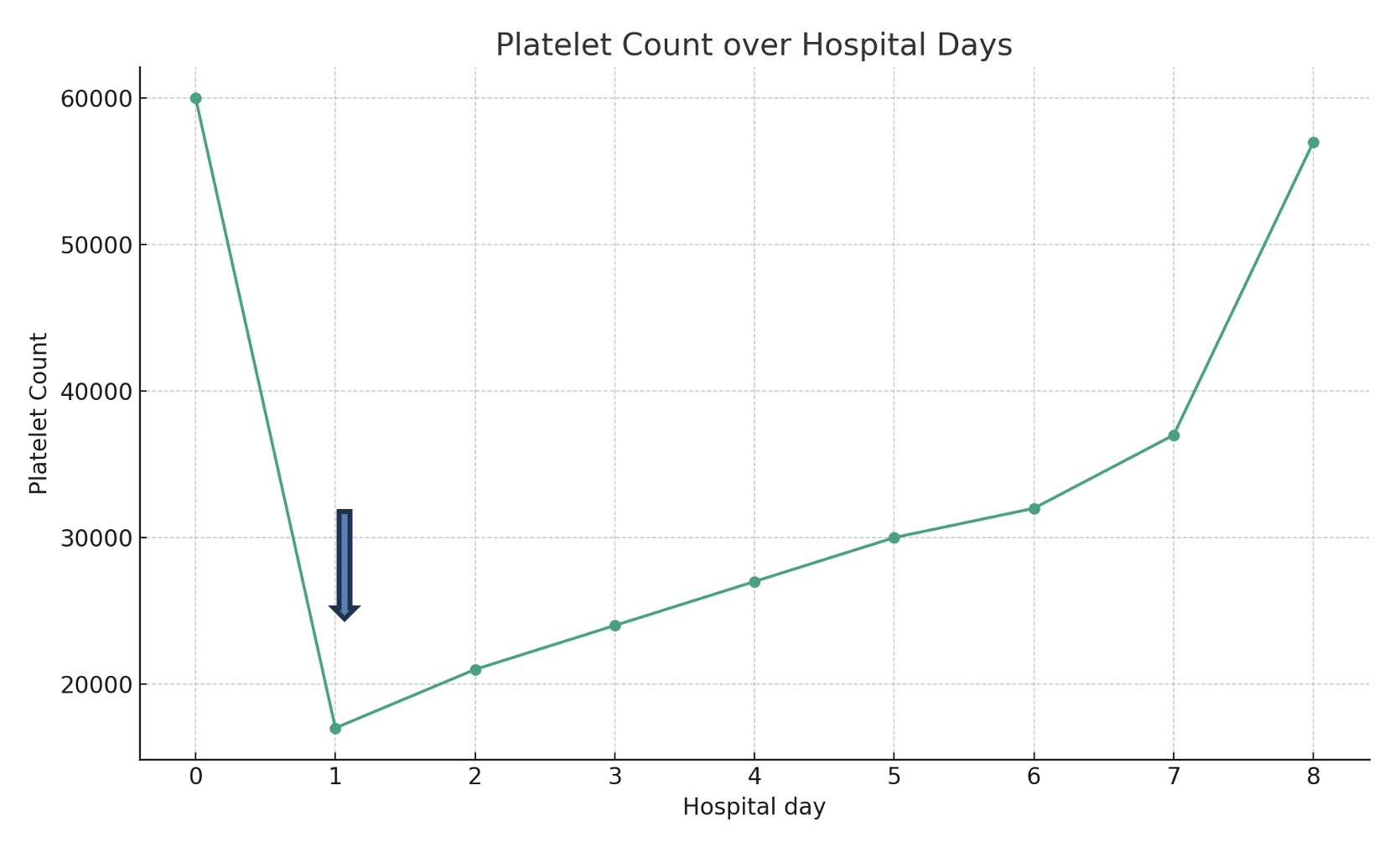
Figure: Trend of platelet count in response to prednisone. The blue arrow indicates when prednisone treatment began.
Disclosures:
Mohamad Elgozair indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Resham Ramkissoon indicated no relevant financial relationships.
Lewis Roberts indicated no relevant financial relationships.
Mohamad Elgozair, MD1, Mohammed Y. Youssef, MD2, Resham Ramkissoon, MD3, Lewis Roberts, MBChB, PhD3. P3846 - When Cirrhosis Isn't the Only Culprit: Recognizing ITP in Severe Thrombocytopenia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Danbury / Yale New Haven Hospital, Danbury, CT; 2Hunt Regional Medical Center, Greenville, TX; 3Mayo Clinic, Rochester, MN
Introduction: Thrombocytopenia, defined as a platelet count below 150,000/µL, is common in advanced chronic liver disease and is associated with increased mortality. Its pathophysiology is multifactorial, involving splenic sequestration, reduced thrombopoietin production, and immune-mediated platelet destruction. In cirrhosis, an acute, severe drop in platelet count should warrant investigation for secondary causes, including infection, malignancy, autoimmunity, medications, or marrow suppression. We present a case of cirrhosis complicated by profound thrombocytopenia due to immune thrombocytopenic purpura (ITP) and alcohol-induced bone marrow suppression.
Case Description/
Methods: A 51-year-old Caucasian woman with alcohol and opioid use disorders, untreated Helicobacter pylori infection, and cirrhosis with portal hypertension presented with nausea, vomiting, tremors, and diaphoresis, consistent with alcohol withdrawal. She had resumed drinking weeks earlier, after sobriety, but stopped four days before admission. On examination, she was jaundiced, lethargic, and encephalopathic. Vitals: HR 113 bpm, RR 30/min. Abdominal exam showed tender hepatomegaly. Labs revealed platelets 17 × 10⁹/L [baseline 60 × 10⁹/L], WBC 1.4 × 10⁹/L, bilirubin 10.2 mg/dL, AST 183 U/L, ammonia 111 µmol/L, hypokalemia, and hypomagnesemia. Imaging showed cirrhotic liver and splenomegaly (15.3 cm) with no thrombosis. Given the severe thrombocytopenia and untreated H. pylori, ITP was suspected. Positive antiplatelet antibodies confirmed the diagnosis. The patient was treated with lorazepam, thiamine, folate, rifaximin, electrolytes, and prednisone 40 mg daily with taper. Platelet counts improved significantly.
Discussion: While thrombocytopenia in cirrhosis is typically attributed to portal hypertension and thrombopoietin deficiency, the abrupt and severe decline in this case suggested an additional process. Alcohol use likely contributed to bone marrow suppression, but the presence of untreated H. pylori and positive antiplatelet antibodies pointed to ITP. H. pylori is an established rare trigger for ITP, potentially through molecular mimicry and immune activation. Identifying and managing such triggers is key in selected patients.
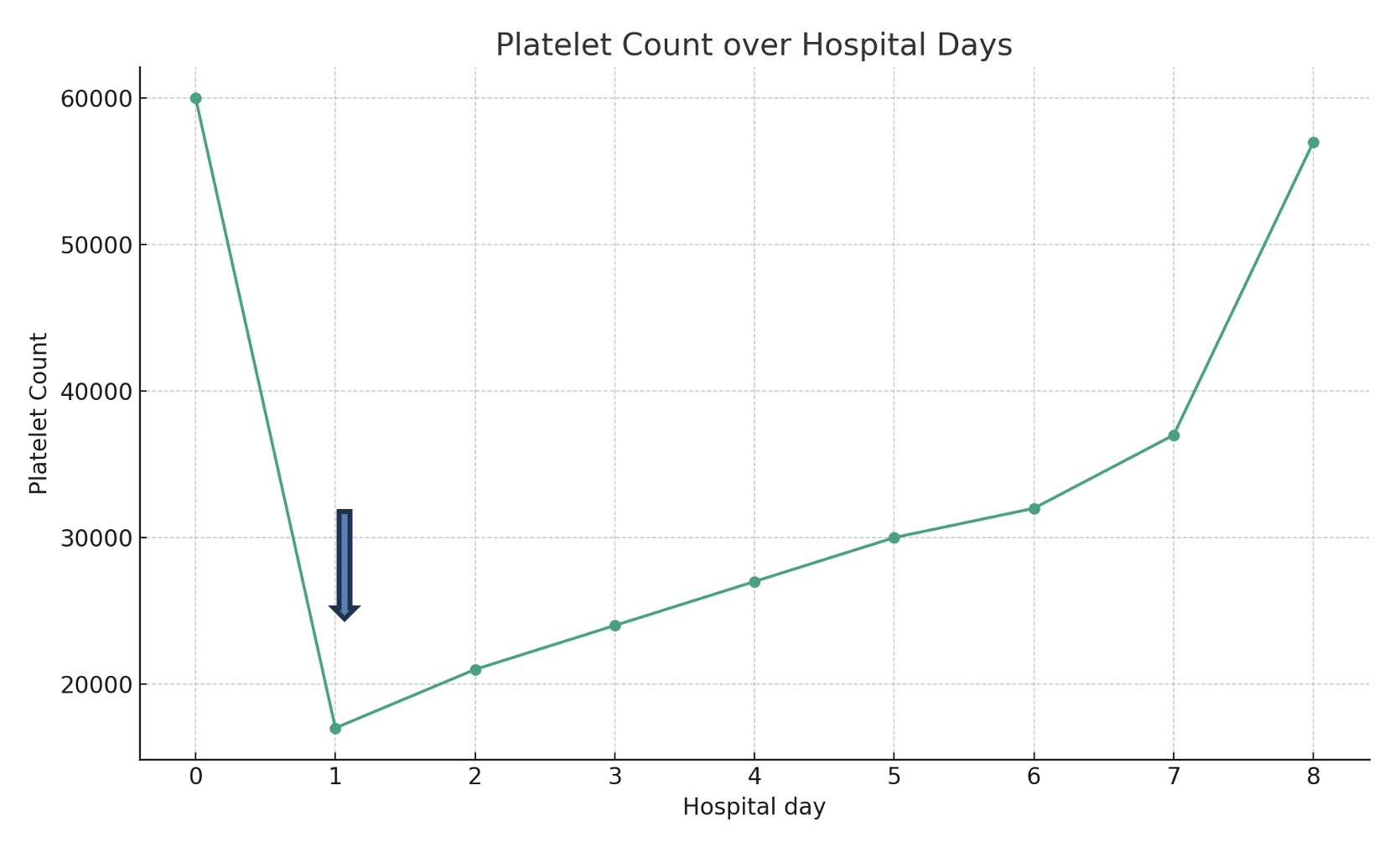
Figure: Trend of platelet count in response to prednisone. The blue arrow indicates when prednisone treatment began.
Disclosures:
Mohamad Elgozair indicated no relevant financial relationships.
Mohammed Y. Youssef indicated no relevant financial relationships.
Resham Ramkissoon indicated no relevant financial relationships.
Lewis Roberts indicated no relevant financial relationships.
Mohamad Elgozair, MD1, Mohammed Y. Youssef, MD2, Resham Ramkissoon, MD3, Lewis Roberts, MBChB, PhD3. P3846 - When Cirrhosis Isn't the Only Culprit: Recognizing ITP in Severe Thrombocytopenia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
