Monday Poster Session
Category: Liver
P3838 - Spontaneous Hepatic Artery Rupture in Decompensated Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hetal Patel, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Hetal Patel, MD1, Yousif Esho, MD1, James S. Love, MD1, Jamie Berkes, MD2
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL
Introduction: Spontaneous hepatic artery rupture is an exceedingly rare event, particularly in the absence of predisposing factors, such as aneurysm, recent hepatic intervention, or trauma. Patients with advanced cirrhosis are predisposed to bleeding complications due to coagulopathy, which increases vascular fragility. However, spontaneous rupture of a non-aneurysmal hepatic artery in this population remains a seldom-reported phenomenon. We present a case of a 60-year-old male with decompensated cirrhosis who developed hemorrhagic shock secondary to spontaneous rupture of the right hepatic artery, without radiologic evidence of aneurysmal disease or trauma.
Case Description/
Methods: A 60 year old male with alcohol-related decompensated cirrhosis presented with chest and abdominal pain. His labs showed negative troponin elevations several hours apart, and his EKG did not indicate ischemia. His total bilirubin was 10.2MG/DL from 3.5MG/DL, AST 128U/L from 29U/L, ALT 65U/L from 15U/L, and INR 3.5 from 1.7. CT of the abdomen showed duodenal wall thickening. He was discharged against medical advice prior to further evaluation but was subsequently found down. He arrived hypothermic to 34.2 C and hypotensive to 82/59. He was alert and conversational but suddenly became disoriented with acute anemia from hemoglobin 8GM/DL to 5.8GM/DL on readmission 13 hours later with lactic acidosis to 5.6MMOL/L. A repeat CT Abdomen indicated new fluid collections in the perihepatic, perisplenic, and paracolic regions. CT Angiogram revealed hemoperitoneum from the inferior right hepatic lobe segment 6 and prominent peritoneal varices. Hemorrhagic shock was managed with vasopressors, massive transfusion protocol, and antibiotics. For rapid hemorrhage control, embolization of the posterior division of the right hepatic artery was pursued rather than hepatectomy due to high risk of mortality from cirrhosis. Despite this, he developed multiorgan failure, metabolic acidosis, and abdominal compartment syndrome that resulted in cardiac arrest.
Discussion: We present a rare case of spontaneous hepatic artery rupture in the setting of decompensated cirrhosis without any known aneurysm or vascular pathology. Portal hypertension and worsening hepatic decompensation increased the risk of persistent bleeding despite embolization. This case highlights the importance of initial evaluation of hemodynamic instability in decompensated cirrhosis with CT Angiography as the preferred diagnostic tool due to high risk of hemobilia in cirrhosis.

Figure: Figure 1: CT Abdomen on admission without hemoperitoneum
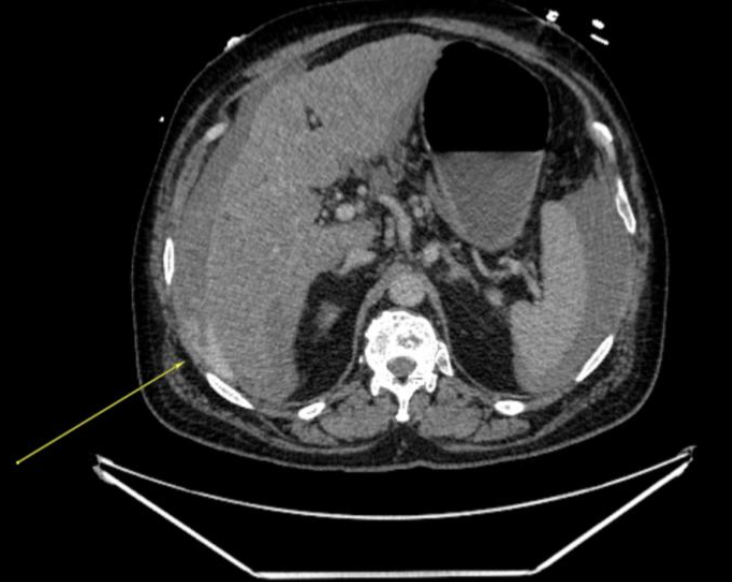
Figure: Figure 2: CT Angiography demonstrating active contrast extravasation of the inferior right hepatic lobe segment 6 with hemoperitoneum
Disclosures:
Hetal Patel indicated no relevant financial relationships.
Yousif Esho indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Jamie Berkes indicated no relevant financial relationships.
Hetal Patel, MD1, Yousif Esho, MD1, James S. Love, MD1, Jamie Berkes, MD2. P3838 - Spontaneous Hepatic Artery Rupture in Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL
Introduction: Spontaneous hepatic artery rupture is an exceedingly rare event, particularly in the absence of predisposing factors, such as aneurysm, recent hepatic intervention, or trauma. Patients with advanced cirrhosis are predisposed to bleeding complications due to coagulopathy, which increases vascular fragility. However, spontaneous rupture of a non-aneurysmal hepatic artery in this population remains a seldom-reported phenomenon. We present a case of a 60-year-old male with decompensated cirrhosis who developed hemorrhagic shock secondary to spontaneous rupture of the right hepatic artery, without radiologic evidence of aneurysmal disease or trauma.
Case Description/
Methods: A 60 year old male with alcohol-related decompensated cirrhosis presented with chest and abdominal pain. His labs showed negative troponin elevations several hours apart, and his EKG did not indicate ischemia. His total bilirubin was 10.2MG/DL from 3.5MG/DL, AST 128U/L from 29U/L, ALT 65U/L from 15U/L, and INR 3.5 from 1.7. CT of the abdomen showed duodenal wall thickening. He was discharged against medical advice prior to further evaluation but was subsequently found down. He arrived hypothermic to 34.2 C and hypotensive to 82/59. He was alert and conversational but suddenly became disoriented with acute anemia from hemoglobin 8GM/DL to 5.8GM/DL on readmission 13 hours later with lactic acidosis to 5.6MMOL/L. A repeat CT Abdomen indicated new fluid collections in the perihepatic, perisplenic, and paracolic regions. CT Angiogram revealed hemoperitoneum from the inferior right hepatic lobe segment 6 and prominent peritoneal varices. Hemorrhagic shock was managed with vasopressors, massive transfusion protocol, and antibiotics. For rapid hemorrhage control, embolization of the posterior division of the right hepatic artery was pursued rather than hepatectomy due to high risk of mortality from cirrhosis. Despite this, he developed multiorgan failure, metabolic acidosis, and abdominal compartment syndrome that resulted in cardiac arrest.
Discussion: We present a rare case of spontaneous hepatic artery rupture in the setting of decompensated cirrhosis without any known aneurysm or vascular pathology. Portal hypertension and worsening hepatic decompensation increased the risk of persistent bleeding despite embolization. This case highlights the importance of initial evaluation of hemodynamic instability in decompensated cirrhosis with CT Angiography as the preferred diagnostic tool due to high risk of hemobilia in cirrhosis.

Figure: Figure 1: CT Abdomen on admission without hemoperitoneum
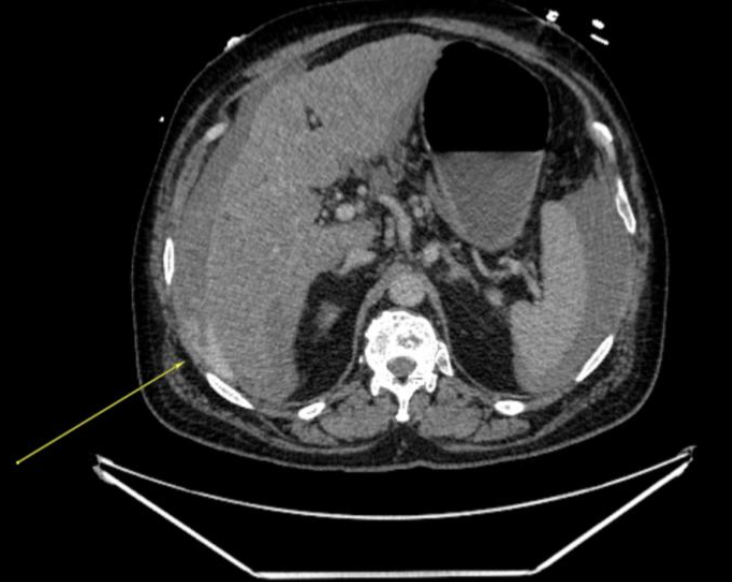
Figure: Figure 2: CT Angiography demonstrating active contrast extravasation of the inferior right hepatic lobe segment 6 with hemoperitoneum
Disclosures:
Hetal Patel indicated no relevant financial relationships.
Yousif Esho indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Jamie Berkes indicated no relevant financial relationships.
Hetal Patel, MD1, Yousif Esho, MD1, James S. Love, MD1, Jamie Berkes, MD2. P3838 - Spontaneous Hepatic Artery Rupture in Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
