Monday Poster Session
Category: Liver
P3819 - Effects of Cardiometabolic Risk Factors on Alcoholic Liver Disease: A Systematic Review
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DP
Dhiraj Peddu, MD
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Dhiraj Peddu, MD1, Matthew Kubina, MD1, Jasnoor Singh, BS1, Matthew Roslund, MS2, Ponni Perumalswami, MD1, Karn Wijarnpreecha, MD3, Vincent L. Chen, MD, MS1
1University of Michigan, Ann Arbor, MI; 2Bassett Medical Center, Cooperstown, NY; 3University of Arizona, Phoenix, AZ
Introduction: Alcohol-associated liver disease (ALD) is a leading cause of advanced liver disease and liver transplantation globally. Cardiometabolic risk factors (CMRF) such as obesity, type 2 diabetes (T2DM), and metabolic syndrome may be associated with worse prognosis in ALD. While recent nomenclature recognizes the interaction between CMRF and moderate alcohol use (MetALD), individuals with very high alcohol intake are classified as ALD regardless of metabolic status. In this study, we performed a systematic review to determine the impact of CMRF on clinical outcomes in patients with ALD.
Methods: We conducted a systematic review of studies published through July 12, 2024, using PubMed, Embase, Scopus, with supplementation from the 2024 AASLD conference abstract catalog. Studies were included if they involved adults (≥18 years) with confirmed ALD, evaluated at least one CMRF such as T2DM, obesity, or metabolic syndrome, and reported longitudinal outcomes using time-to-event metrics. Titles and abstracts were independently screened by two reviewers, followed by a full-text review to determine final eligibility. The primary outcomes included incident cirrhosis, hepatocellular carcinoma, mortality (overall, liver-related, and cardiovascular-related), cardiovascular events, liver-related complications, liver transplantation, and other systemic outcomes.
Results: Thirteen studies, comprising 56,876 patients with ALD, were included in the final analysis. Diabetes was consistently associated with increased risks of overall mortality (aHR 3.00), liver-related mortality (aHR 3.6), HCC (HRs 1.6–21.7), and cardiovascular mortality (aHR 19.91) (Table 1). Elevated BMI was linked to higher all-cause mortality (aHR 1.16-1.58), cardiovascular mortality (aHR 3.76), HCC incidence (HR 2.0-2.9), and liver-related mortality (aHR 16.22) (Table 1). Metabolic syndrome was associated with increased risks of overall (HR 1.27-2.37) and liver-related mortality (HR 1.47-2.06) with a higher burden of CMRF associated with declines in both transplant-free survival and hepatic recompensation (Figure 1).
Discussion: CMRF, including diabetes, obesity, and metabolic syndrome, are consistently associated with worse hepatic and extra-hepatic outcomes in individuals with ALD. A nomenclature amendment acknowledging the impact of CMRF in ALD—not just moderate alcohol use—may more accurately characterize ALD subcategories.
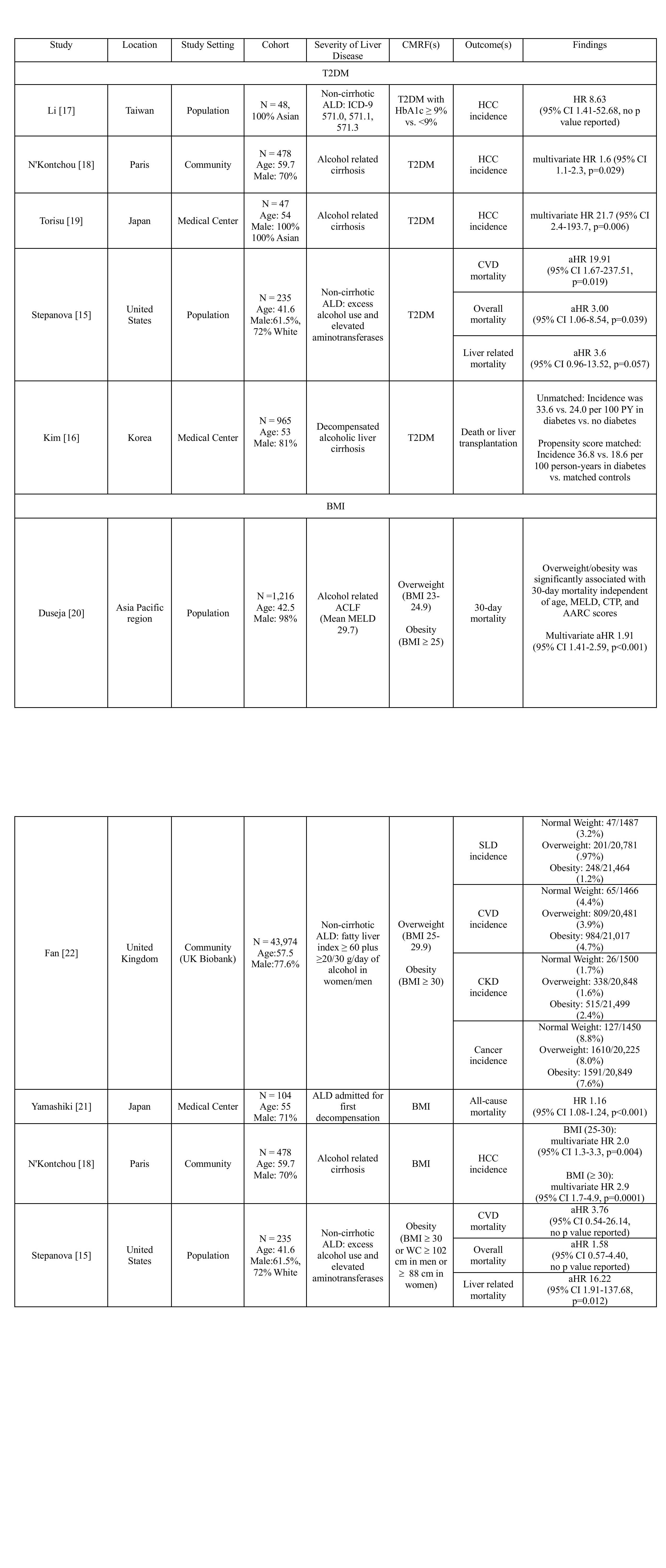
Figure: Table 1: Impact of Type 2 Diabetes Mellitus (T2DM) and Body Mass Index (BMI) on Clinical Outcomes in Alcohol-associated Liver Disease (ALD). Unless otherwise specified, effect sizes are shown as either HR (95% confidence interval), OR (95% confidence interval), RR (95% confidence interval).
Abbreviations: cMRF, cardiometabolic risk factor; HCC, hepatocellular carcinoma; HR, hazard ratio; aHR, adjusted hazard ratio; MELD, model for end stage liver disease; ACLF, acute on chronic liver failure; CTP, child Turcotte pugh; AARC, APASL ACLF Research Consortium; BMI, body mass index; ALD, alcohol related liver disease; WC, waist circumference; SLD, significant liver disease; CVD, cardiovascular disease; CKD, chronic kidney disease.
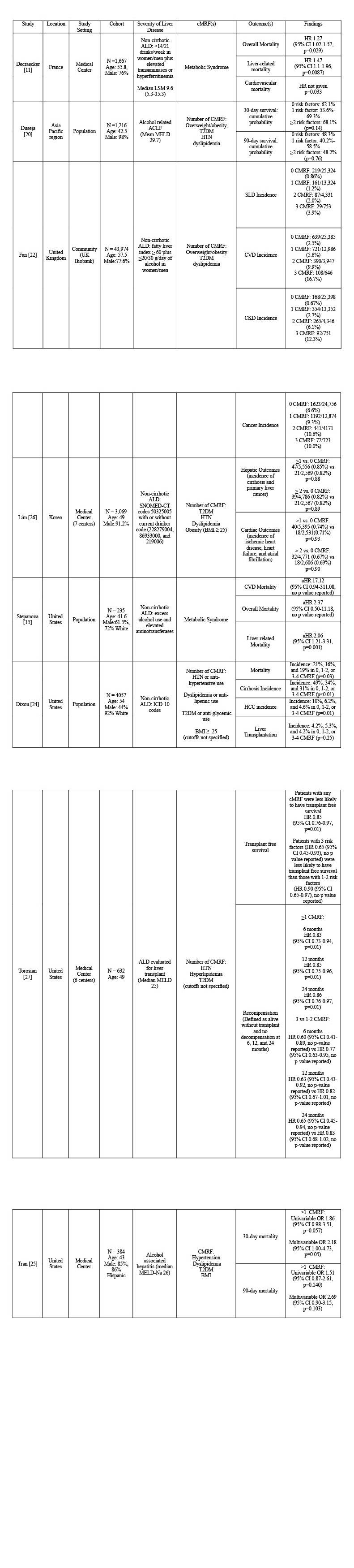
Figure: Figure 1: Impact of Metabolic Syndrome (MS) on Clinical Outcomes in Alcohol-associated Liver Disease (ALD). Unless otherwise specified, effect sizes are shown as either HR (95% confidence interval), OR (95% confidence interval), RR (95% confidence interval).
Abbreviations: cMRF, cardiometabolic risk factor; HCC, hepatocellular carcinoma; HR, hazard ratio; aHR, adjusted hazard ratio; LSM, liver stiffness measurement; CVD, cardiovascular disease; CV, cardiovascular; MI, myocardial infarction; OR, odds ratio; ACLF, acute on chronic liver failure; MELD, model for end stage liver disease; BMI, body mass index; T2DM, type 2 diabetes mellitus; RR, relative risk; ALD, alcohol related liver disease; MetS, metabolic dysfunction score; MetR, metabolic risk factor; BP, blood pressure; HDL, high density lipoprotein; WC, waist circumference; SLD, significant liver disease; CKD, chronic kidney disease; SNOMED-CT, systemized nomenclature for medicine-clinical terms; CI, confidence interval.
Disclosures:
Dhiraj Peddu indicated no relevant financial relationships.
Matthew Kubina indicated no relevant financial relationships.
Jasnoor Singh indicated no relevant financial relationships.
Matthew Roslund indicated no relevant financial relationships.
Ponni Perumalswami indicated no relevant financial relationships.
Karn Wijarnpreecha indicated no relevant financial relationships.
Vincent Chen: AstraZeneca – Grant/Research Support. Ipsen – Grant/Research Support. KOWA – Grant/Research Support.
Dhiraj Peddu, MD1, Matthew Kubina, MD1, Jasnoor Singh, BS1, Matthew Roslund, MS2, Ponni Perumalswami, MD1, Karn Wijarnpreecha, MD3, Vincent L. Chen, MD, MS1. P3819 - Effects of Cardiometabolic Risk Factors on Alcoholic Liver Disease: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Bassett Medical Center, Cooperstown, NY; 3University of Arizona, Phoenix, AZ
Introduction: Alcohol-associated liver disease (ALD) is a leading cause of advanced liver disease and liver transplantation globally. Cardiometabolic risk factors (CMRF) such as obesity, type 2 diabetes (T2DM), and metabolic syndrome may be associated with worse prognosis in ALD. While recent nomenclature recognizes the interaction between CMRF and moderate alcohol use (MetALD), individuals with very high alcohol intake are classified as ALD regardless of metabolic status. In this study, we performed a systematic review to determine the impact of CMRF on clinical outcomes in patients with ALD.
Methods: We conducted a systematic review of studies published through July 12, 2024, using PubMed, Embase, Scopus, with supplementation from the 2024 AASLD conference abstract catalog. Studies were included if they involved adults (≥18 years) with confirmed ALD, evaluated at least one CMRF such as T2DM, obesity, or metabolic syndrome, and reported longitudinal outcomes using time-to-event metrics. Titles and abstracts were independently screened by two reviewers, followed by a full-text review to determine final eligibility. The primary outcomes included incident cirrhosis, hepatocellular carcinoma, mortality (overall, liver-related, and cardiovascular-related), cardiovascular events, liver-related complications, liver transplantation, and other systemic outcomes.
Results: Thirteen studies, comprising 56,876 patients with ALD, were included in the final analysis. Diabetes was consistently associated with increased risks of overall mortality (aHR 3.00), liver-related mortality (aHR 3.6), HCC (HRs 1.6–21.7), and cardiovascular mortality (aHR 19.91) (Table 1). Elevated BMI was linked to higher all-cause mortality (aHR 1.16-1.58), cardiovascular mortality (aHR 3.76), HCC incidence (HR 2.0-2.9), and liver-related mortality (aHR 16.22) (Table 1). Metabolic syndrome was associated with increased risks of overall (HR 1.27-2.37) and liver-related mortality (HR 1.47-2.06) with a higher burden of CMRF associated with declines in both transplant-free survival and hepatic recompensation (Figure 1).
Discussion: CMRF, including diabetes, obesity, and metabolic syndrome, are consistently associated with worse hepatic and extra-hepatic outcomes in individuals with ALD. A nomenclature amendment acknowledging the impact of CMRF in ALD—not just moderate alcohol use—may more accurately characterize ALD subcategories.
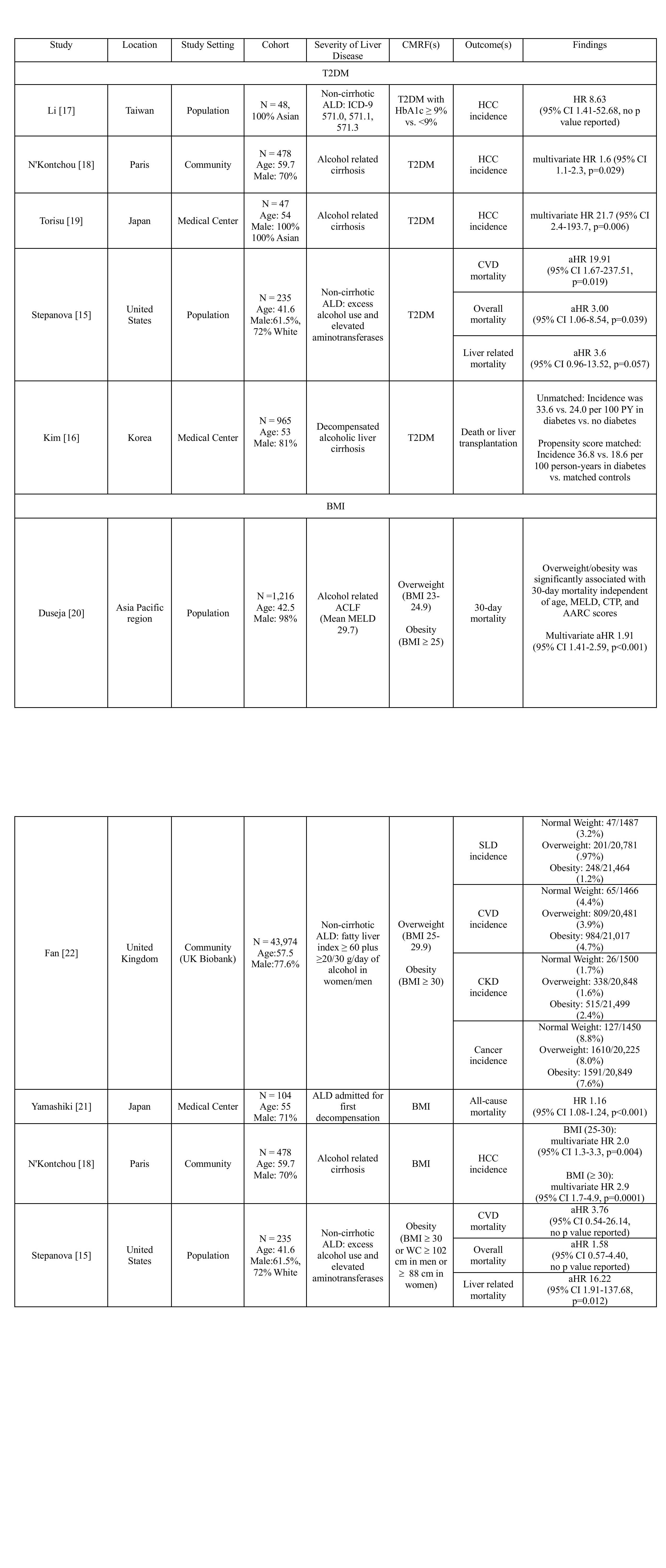
Figure: Table 1: Impact of Type 2 Diabetes Mellitus (T2DM) and Body Mass Index (BMI) on Clinical Outcomes in Alcohol-associated Liver Disease (ALD). Unless otherwise specified, effect sizes are shown as either HR (95% confidence interval), OR (95% confidence interval), RR (95% confidence interval).
Abbreviations: cMRF, cardiometabolic risk factor; HCC, hepatocellular carcinoma; HR, hazard ratio; aHR, adjusted hazard ratio; MELD, model for end stage liver disease; ACLF, acute on chronic liver failure; CTP, child Turcotte pugh; AARC, APASL ACLF Research Consortium; BMI, body mass index; ALD, alcohol related liver disease; WC, waist circumference; SLD, significant liver disease; CVD, cardiovascular disease; CKD, chronic kidney disease.
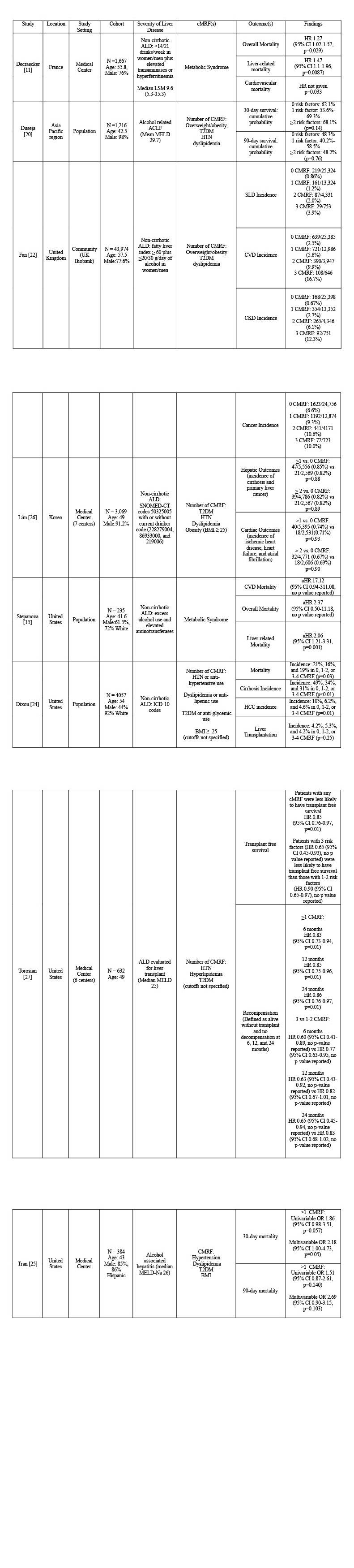
Figure: Figure 1: Impact of Metabolic Syndrome (MS) on Clinical Outcomes in Alcohol-associated Liver Disease (ALD). Unless otherwise specified, effect sizes are shown as either HR (95% confidence interval), OR (95% confidence interval), RR (95% confidence interval).
Abbreviations: cMRF, cardiometabolic risk factor; HCC, hepatocellular carcinoma; HR, hazard ratio; aHR, adjusted hazard ratio; LSM, liver stiffness measurement; CVD, cardiovascular disease; CV, cardiovascular; MI, myocardial infarction; OR, odds ratio; ACLF, acute on chronic liver failure; MELD, model for end stage liver disease; BMI, body mass index; T2DM, type 2 diabetes mellitus; RR, relative risk; ALD, alcohol related liver disease; MetS, metabolic dysfunction score; MetR, metabolic risk factor; BP, blood pressure; HDL, high density lipoprotein; WC, waist circumference; SLD, significant liver disease; CKD, chronic kidney disease; SNOMED-CT, systemized nomenclature for medicine-clinical terms; CI, confidence interval.
Disclosures:
Dhiraj Peddu indicated no relevant financial relationships.
Matthew Kubina indicated no relevant financial relationships.
Jasnoor Singh indicated no relevant financial relationships.
Matthew Roslund indicated no relevant financial relationships.
Ponni Perumalswami indicated no relevant financial relationships.
Karn Wijarnpreecha indicated no relevant financial relationships.
Vincent Chen: AstraZeneca – Grant/Research Support. Ipsen – Grant/Research Support. KOWA – Grant/Research Support.
Dhiraj Peddu, MD1, Matthew Kubina, MD1, Jasnoor Singh, BS1, Matthew Roslund, MS2, Ponni Perumalswami, MD1, Karn Wijarnpreecha, MD3, Vincent L. Chen, MD, MS1. P3819 - Effects of Cardiometabolic Risk Factors on Alcoholic Liver Disease: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
