Monday Poster Session
Category: Liver
P3814 - Fighting the Silent Threat: A Guideline-Directed Quality Improvement Initiative for Hepatitis C Screening in Primary Care
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- TA
Tareq Alsaleh, MD
Department of Internal Medicine, AdventHealth Orlando
Orlando, FL
Presenting Author(s)
Tareq Alsaleh, MD1, Prachi Mann, MD2, Amna Malik, MD1, Nouman Shafique, MD1, Magda Elamin, MD1, Nihal Khan, MD1, Daniel Tambunan, MD1
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, Adventhealth Orlando, Orlando, FL
Introduction: Hepatitis C virus (HCV) is the most prevalent blood-borne pathogen in the US, linked to more deaths than the top 60 other reportable infectious diseases combined. Most patients with chronic HCV infection are asymptomatic, and 10-20% of untreated cases can progress to cirrhosis. Screening is critical for identifying and treating asymptomatic cases. We assessed the use of USPSTF guideline-directed HCV screening at our primary care clinic with the aim to identify potential barriers and improve screening compliance.
Methods: Using the Epic electronic medical record (EMR) clinical data exploration and analysis tool, we retrospectively reviewed new patient visits at our primary care clinic from August 2024 to February 2025 to identify adults aged 18-79 with no prior history of hepatitis C testing. The primary outcome was the use of HCV testing for screening. Subsequently, we implemented an electronic survey among clinic providers to identify barriers to screening.
Results: A total of 589 new-patient clinic visits were included, with mean patient age 42.8 years and 190 (32.2%) males. Hepatitis-C screening tests for average-risk adults were ordered for 93 (15.8%) patients, with only 67 (72%) tests being completed by patients with one positive result. Test refusal was documented in only 2 (0.4%) visits, and the need for screening was revisited in 3.8% of patients who had follow-up visits (n=316).
The survey response rate was 47.9%. Most respondents (65.2%) reported being comfortable with hepatitis C screening and diagnostic algorithms. The most commonly used tool to identify screening subjects were clinical guidelines (54.5%), followed by EHR-based decision support tools (40.9%). The most common barrier to screening was patient refusal or lack of interest (60.9%), with most patients not believing they are at risk (60.9%). The most favored support tool to improve screening among the respondents was EMR prompts (73.9%), followed by patient education materials (34.8%).
Discussion: Our study highlights a glaring gap in HCV screening performance, both on the part of providers and patients. Our providers expressed high awareness of screening guidelines but marked resistance to screening from patients. This may be due to a lack of awareness of the risks of HCV by the general population. The respondents also expressed the importance of EHR-support-based tools. Based on respondent feedback, we aim to implement EHR-based support tools and focused educational events to improve screening compliance.
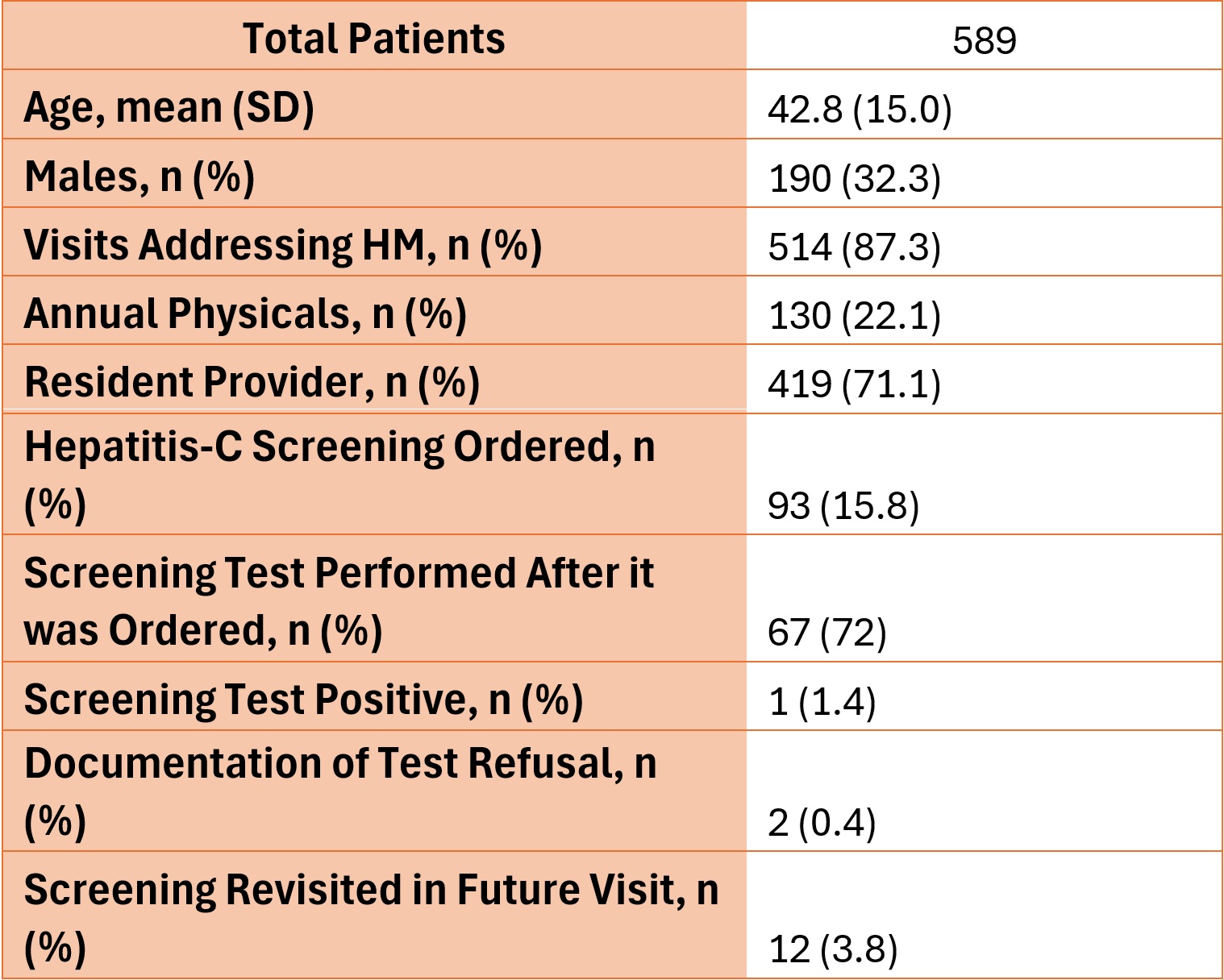
Figure: Table 1: Patient Characteristics and Hepatitis C Screening Outcomes
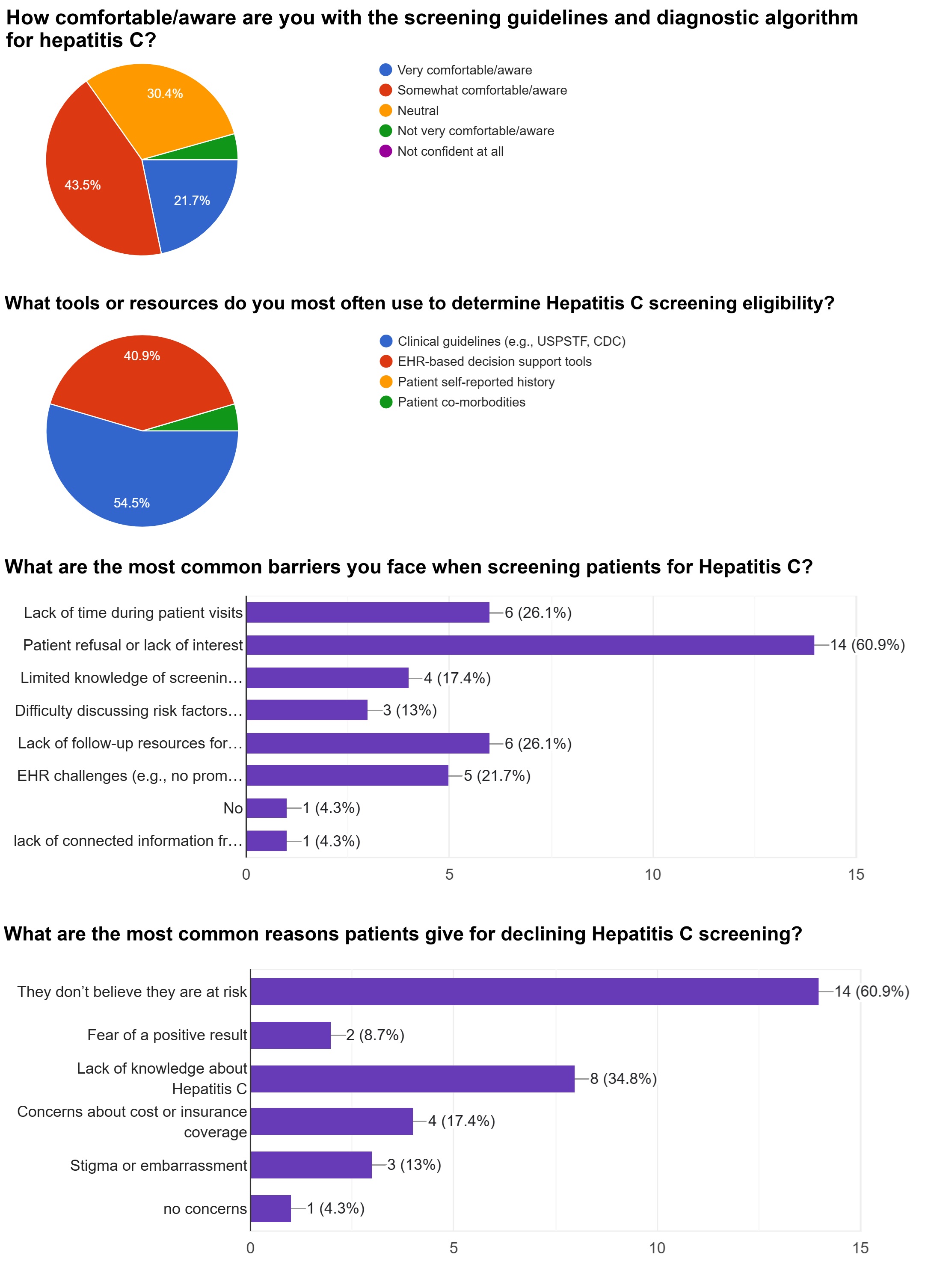
Figure: Figure 1. Answers to four of the questions from the questionnaire. Patient refusal was the most commonly reported barrier to screening, with believing they are not at risk.
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Prachi Mann indicated no relevant financial relationships.
Amna Malik indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Magda Elamin indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Daniel Tambunan indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Prachi Mann, MD2, Amna Malik, MD1, Nouman Shafique, MD1, Magda Elamin, MD1, Nihal Khan, MD1, Daniel Tambunan, MD1. P3814 - Fighting the Silent Threat: A Guideline-Directed Quality Improvement Initiative for Hepatitis C Screening in Primary Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, AdventHealth Orlando, Orlando, FL; 2Department of Internal Medicine, Adventhealth Orlando, Orlando, FL
Introduction: Hepatitis C virus (HCV) is the most prevalent blood-borne pathogen in the US, linked to more deaths than the top 60 other reportable infectious diseases combined. Most patients with chronic HCV infection are asymptomatic, and 10-20% of untreated cases can progress to cirrhosis. Screening is critical for identifying and treating asymptomatic cases. We assessed the use of USPSTF guideline-directed HCV screening at our primary care clinic with the aim to identify potential barriers and improve screening compliance.
Methods: Using the Epic electronic medical record (EMR) clinical data exploration and analysis tool, we retrospectively reviewed new patient visits at our primary care clinic from August 2024 to February 2025 to identify adults aged 18-79 with no prior history of hepatitis C testing. The primary outcome was the use of HCV testing for screening. Subsequently, we implemented an electronic survey among clinic providers to identify barriers to screening.
Results: A total of 589 new-patient clinic visits were included, with mean patient age 42.8 years and 190 (32.2%) males. Hepatitis-C screening tests for average-risk adults were ordered for 93 (15.8%) patients, with only 67 (72%) tests being completed by patients with one positive result. Test refusal was documented in only 2 (0.4%) visits, and the need for screening was revisited in 3.8% of patients who had follow-up visits (n=316).
The survey response rate was 47.9%. Most respondents (65.2%) reported being comfortable with hepatitis C screening and diagnostic algorithms. The most commonly used tool to identify screening subjects were clinical guidelines (54.5%), followed by EHR-based decision support tools (40.9%). The most common barrier to screening was patient refusal or lack of interest (60.9%), with most patients not believing they are at risk (60.9%). The most favored support tool to improve screening among the respondents was EMR prompts (73.9%), followed by patient education materials (34.8%).
Discussion: Our study highlights a glaring gap in HCV screening performance, both on the part of providers and patients. Our providers expressed high awareness of screening guidelines but marked resistance to screening from patients. This may be due to a lack of awareness of the risks of HCV by the general population. The respondents also expressed the importance of EHR-support-based tools. Based on respondent feedback, we aim to implement EHR-based support tools and focused educational events to improve screening compliance.
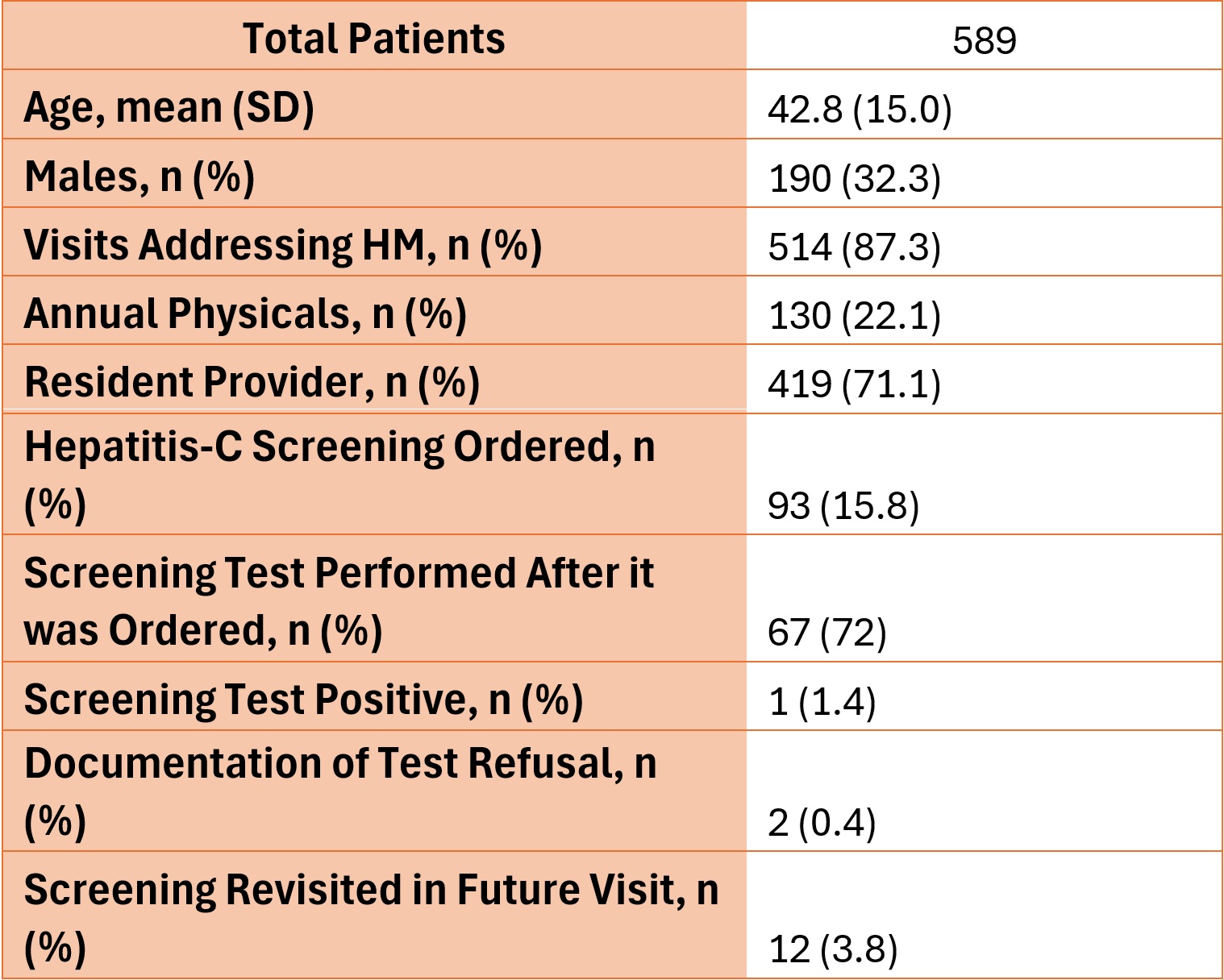
Figure: Table 1: Patient Characteristics and Hepatitis C Screening Outcomes
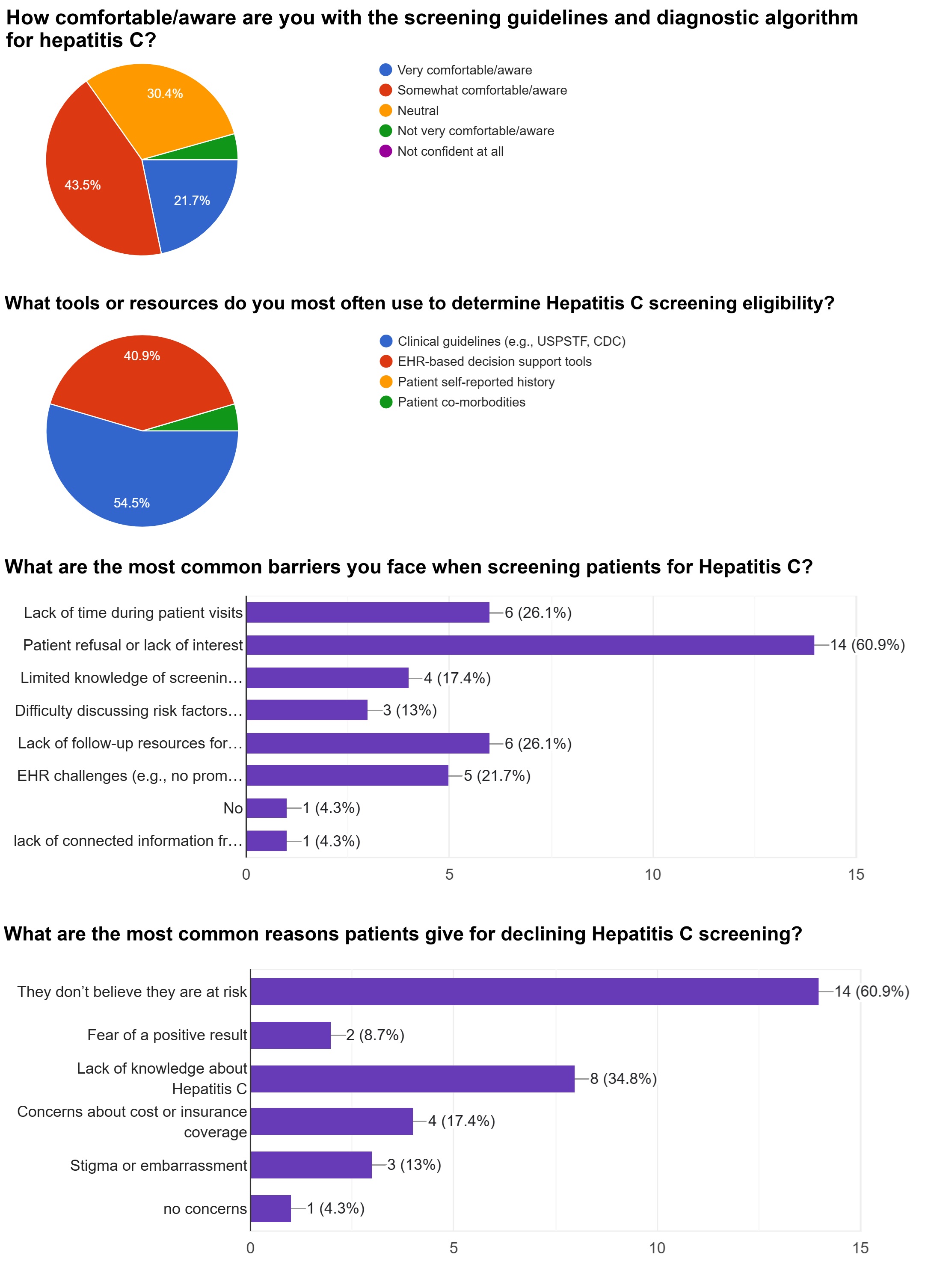
Figure: Figure 1. Answers to four of the questions from the questionnaire. Patient refusal was the most commonly reported barrier to screening, with believing they are not at risk.
Disclosures:
Tareq Alsaleh indicated no relevant financial relationships.
Prachi Mann indicated no relevant financial relationships.
Amna Malik indicated no relevant financial relationships.
Nouman Shafique indicated no relevant financial relationships.
Magda Elamin indicated no relevant financial relationships.
Nihal Khan indicated no relevant financial relationships.
Daniel Tambunan indicated no relevant financial relationships.
Tareq Alsaleh, MD1, Prachi Mann, MD2, Amna Malik, MD1, Nouman Shafique, MD1, Magda Elamin, MD1, Nihal Khan, MD1, Daniel Tambunan, MD1. P3814 - Fighting the Silent Threat: A Guideline-Directed Quality Improvement Initiative for Hepatitis C Screening in Primary Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
