Monday Poster Session
Category: Liver
P3812 - National Disparities in Variceal Upper GI Hemorrhage Between Teaching and Non-Teaching Institutions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Luqman Baloch, MD
Mercyhealth Gastroenterology Fellowship
Rockford, IL
Presenting Author(s)
Luqman Baloch, MD1, Abu Fahad Abbasi, MD1, Ahmet Sakiri, MD2, Sultan Ahmed, DO2, Ammar Aqeel, MD1, Abdul Mubeen Khan, MD1, Thayer Hamoudah, MD3, Altaf Dawood, MD3, Naser Khan, MD3, Baseer Qazi, MD3
1Mercyhealth Gastroenterology Fellowship, Rockford, IL; 2Mercyhealth Internal Medicine Residency, Rockford, IL; 3Mercyhealth Gastroenterology, Rockford, IL
Introduction: This study evaluates national outcomes for variceal upper GI hemorrhage (VUGIH) treated at teaching vs. non-teaching facilities.
Methods: National Inpatient Sample data from 2016 to 2020 was analyzed for VUGIH. In-hospital mortality was the primary outcome assessed. ICD-10 codes categorized patients by facility teaching status, insurance status, sex, & race. A multivariate logistic regression evaluated risk factors associated with in-hospital mortality. Secondary outcomes included variceal banding rates, time to endoscopy, TIPS placement, & time to TIPS. P < 0.05 was statistically significant. AI software ChatGPT was utilized to verify statistical analyses.
Results: In 333,120 patients with VUGIH, teaching facilities had higher in-hospital mortality (10.6% vs. 8.2%; OR 1.27 [1.23-1.30]; P < 0.01). Variceal banding was similar with no statistical significant difference between teaching & non-teaching hospitals (36.4% vs. 37.7%; OR 0.94; P = 0.052). Time to endoscopy was longer in teaching facilities (1.2 days vs. 1 day; P = 0.012). Teaching facilities performed TIPS procedures more often (0.75% vs. 0.19%; OR 3.42; P < 0.01) however time to TIPS was similar (1.7 days vs. 1.4 days; P = 0.07).
Multivariate logistic regression revealed several other risk factors for in-hospital mortality. These included malignancy, CHF, HIV, CVA, male sex, Asian race, & uninsured status all increased risk of mortality (P < 0.01).
Discussion: Teaching hospitals had higher in-hospital mortality likely reflecting greater patient complexity. Similar banding rates suggest similar access to endoscopic treatment. Time to TIPS, though not statistically different, did approach near significance (P = 0.07). This difference may be attributed to slightly longer times to endoscopy & TIPS at teaching facilities.
Despite correction with multivariate logistic regression that confirmed risk factors that increased in-hospital mortality, our analysis revealed 27% higher odds of mortality in teaching hospitals. This may reflect unaccounted for variables that may be contributing to the higher mortality rates. Factors such as active alcohol use, degree of hepatic disease, & severity of portal hypertension were not assessed. Limitations of our study include its retrospective design, use of ICD-10 codes, & lack of access to procedural findings. AI ChatGPT verified our statistical analyses. Despite these limitations, the large sample size & multivariate analysis strengthen our findings.
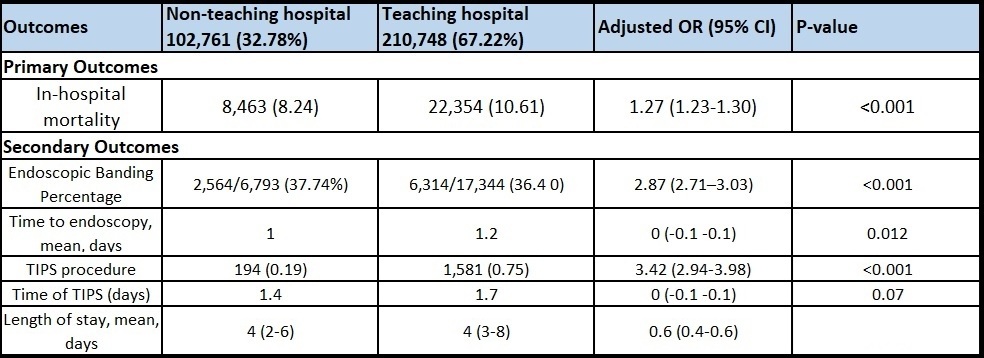
Figure: Variceal Upper GI Hemorrhage Outcomes
Disclosures:
Luqman Baloch indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Ahmet Sakiri indicated no relevant financial relationships.
Sultan Ahmed indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Abdul Mubeen Khan indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Luqman Baloch, MD1, Abu Fahad Abbasi, MD1, Ahmet Sakiri, MD2, Sultan Ahmed, DO2, Ammar Aqeel, MD1, Abdul Mubeen Khan, MD1, Thayer Hamoudah, MD3, Altaf Dawood, MD3, Naser Khan, MD3, Baseer Qazi, MD3. P3812 - National Disparities in Variceal Upper GI Hemorrhage Between Teaching and Non-Teaching Institutions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mercyhealth Gastroenterology Fellowship, Rockford, IL; 2Mercyhealth Internal Medicine Residency, Rockford, IL; 3Mercyhealth Gastroenterology, Rockford, IL
Introduction: This study evaluates national outcomes for variceal upper GI hemorrhage (VUGIH) treated at teaching vs. non-teaching facilities.
Methods: National Inpatient Sample data from 2016 to 2020 was analyzed for VUGIH. In-hospital mortality was the primary outcome assessed. ICD-10 codes categorized patients by facility teaching status, insurance status, sex, & race. A multivariate logistic regression evaluated risk factors associated with in-hospital mortality. Secondary outcomes included variceal banding rates, time to endoscopy, TIPS placement, & time to TIPS. P < 0.05 was statistically significant. AI software ChatGPT was utilized to verify statistical analyses.
Results: In 333,120 patients with VUGIH, teaching facilities had higher in-hospital mortality (10.6% vs. 8.2%; OR 1.27 [1.23-1.30]; P < 0.01). Variceal banding was similar with no statistical significant difference between teaching & non-teaching hospitals (36.4% vs. 37.7%; OR 0.94; P = 0.052). Time to endoscopy was longer in teaching facilities (1.2 days vs. 1 day; P = 0.012). Teaching facilities performed TIPS procedures more often (0.75% vs. 0.19%; OR 3.42; P < 0.01) however time to TIPS was similar (1.7 days vs. 1.4 days; P = 0.07).
Multivariate logistic regression revealed several other risk factors for in-hospital mortality. These included malignancy, CHF, HIV, CVA, male sex, Asian race, & uninsured status all increased risk of mortality (P < 0.01).
Discussion: Teaching hospitals had higher in-hospital mortality likely reflecting greater patient complexity. Similar banding rates suggest similar access to endoscopic treatment. Time to TIPS, though not statistically different, did approach near significance (P = 0.07). This difference may be attributed to slightly longer times to endoscopy & TIPS at teaching facilities.
Despite correction with multivariate logistic regression that confirmed risk factors that increased in-hospital mortality, our analysis revealed 27% higher odds of mortality in teaching hospitals. This may reflect unaccounted for variables that may be contributing to the higher mortality rates. Factors such as active alcohol use, degree of hepatic disease, & severity of portal hypertension were not assessed. Limitations of our study include its retrospective design, use of ICD-10 codes, & lack of access to procedural findings. AI ChatGPT verified our statistical analyses. Despite these limitations, the large sample size & multivariate analysis strengthen our findings.
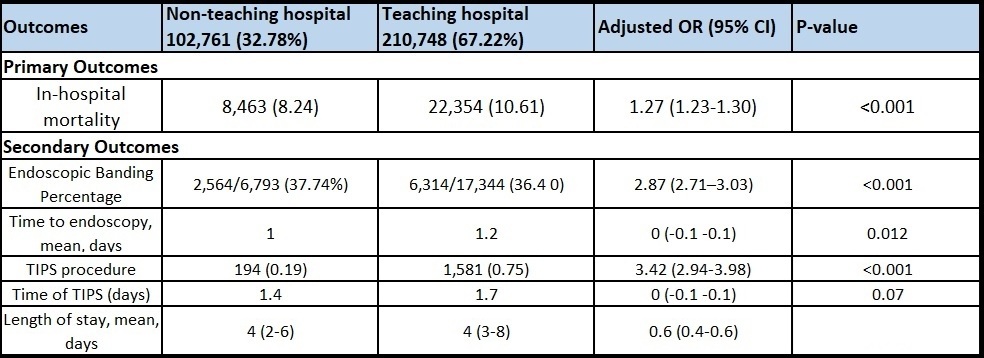
Figure: Variceal Upper GI Hemorrhage Outcomes
Disclosures:
Luqman Baloch indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Ahmet Sakiri indicated no relevant financial relationships.
Sultan Ahmed indicated no relevant financial relationships.
Ammar Aqeel indicated no relevant financial relationships.
Abdul Mubeen Khan indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Luqman Baloch, MD1, Abu Fahad Abbasi, MD1, Ahmet Sakiri, MD2, Sultan Ahmed, DO2, Ammar Aqeel, MD1, Abdul Mubeen Khan, MD1, Thayer Hamoudah, MD3, Altaf Dawood, MD3, Naser Khan, MD3, Baseer Qazi, MD3. P3812 - National Disparities in Variceal Upper GI Hemorrhage Between Teaching and Non-Teaching Institutions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
