Monday Poster Session
Category: Liver
P3754 - Navigating Cirrhosis Care: The Impact of Clear Goals and Seamless Transitions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah Darnell, DO
University of Kentucky
Lexington, KY
Presenting Author(s)
Hannah Darnell, DO, Nishant Tripathi, MBBS, Stephanie Leung, MD, Elizabeth Wilson, RN, Jamie Edwards, RN, Thomas Jackson, MHS, Patricia Santos, MD, Rani Chikkanna, MD
University of Kentucky, Lexington, KY
Introduction: Hospital readmissions among patients with decompensated cirrhosis present a significant clinical and economic burden, with 30-day readmission rates ranging from 20–37%. While many readmissions are non-preventable, some may be avoided through targeted interventions. In 2023, the University of Kentucky reported a 21% 30-day unplanned readmission rate for patients with decompensated cirrhosis. In response, a quality improvement (QI) initiative was launched to reduce 30-day readmissions to 16% by June 2025, focusing on timely outpatient large-volume paracentesis (LVP) and improved transitions of care (TOC) via nurse navigators.
Methods: This QI project included adults >18 years hospitalized under medical severity diagnosis-related group codes 432, 433, or 434. In August 2024, three primary interventions were implemented: (1) timely LVP scheduling, (2) referral to high-risk discharge clinics, and (3) nurse navigator-led follow-up coordination. An Epic discharge order set was developed to streamline ambulatory lab orders and follow-up appointment scheduling. The target was ≥50% adherence for each intervention. Data was extracted from Vizient and Epic.
Results: In 2024, 474 patients met inclusion criteria and 104 (21.9%) were readmitted within 30 days. Following intervention in August, the average readmission rate fell to 19.3% by December. Monthly unplanned readmissions dropped from nine to seven (October–December), with estimated monthly cost savings of $29,675. However, rates rose to 32.5% in January–February 2025, revealing poor process adherence: only 30% had LVP scheduled, 46% were referred to the high-risk clinic, and 27.6% had nurse navigator coordination.
Discussion: Initial reductions in readmission rates suggest our interventions were effective, but sustainability was a challenge. A rise in readmissions in early 2025 highlighted gaps in process adherence, particularly in TOC through nurse navigators. In response, a dashboard was developed to help nurse navigators identify high-risk patients and proactively coordinate LVP and follow-up appointments with the primary team. As a result, 72% of patients had follow-up in March and 92.9% in April of 2025. A chart review of Oct–Dec 2024 readmissions showed 35% mortality within 3 months, an average MELD of 25, with 59% likely to benefit from palliative care and 18% deemed preventable. Future interventions will encourage early palliative care consults for patients with higher MELD to clarify goals of care and reduce avoidable hospitalizations.
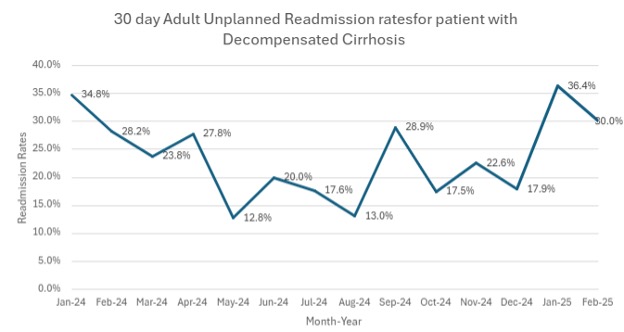
Figure: 30 day adult unplanned readmission rates for patients with decompensated cirrhosis
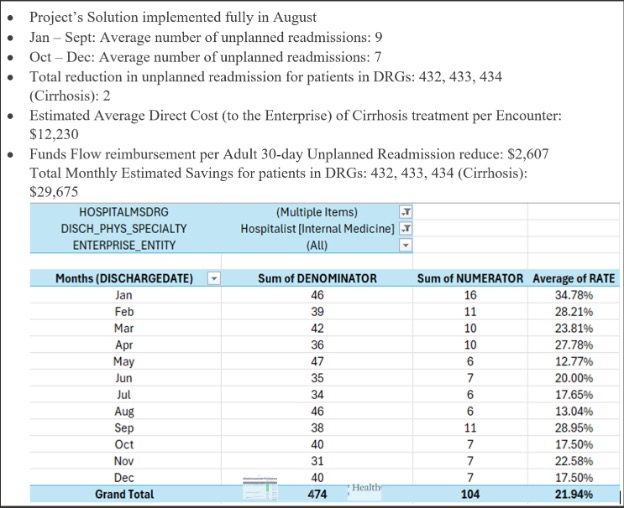
Figure: Return on Investment Following Implementation of Readmission Reduction Interventions in August 2024
Disclosures:
Hannah Darnell indicated no relevant financial relationships.
Nishant Tripathi indicated no relevant financial relationships.
Stephanie Leung indicated no relevant financial relationships.
Elizabeth Wilson indicated no relevant financial relationships.
Jamie Edwards indicated no relevant financial relationships.
Thomas Jackson indicated no relevant financial relationships.
Patricia Santos indicated no relevant financial relationships.
Rani Chikkanna indicated no relevant financial relationships.
Hannah Darnell, DO, Nishant Tripathi, MBBS, Stephanie Leung, MD, Elizabeth Wilson, RN, Jamie Edwards, RN, Thomas Jackson, MHS, Patricia Santos, MD, Rani Chikkanna, MD. P3754 - Navigating Cirrhosis Care: The Impact of Clear Goals and Seamless Transitions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Kentucky, Lexington, KY
Introduction: Hospital readmissions among patients with decompensated cirrhosis present a significant clinical and economic burden, with 30-day readmission rates ranging from 20–37%. While many readmissions are non-preventable, some may be avoided through targeted interventions. In 2023, the University of Kentucky reported a 21% 30-day unplanned readmission rate for patients with decompensated cirrhosis. In response, a quality improvement (QI) initiative was launched to reduce 30-day readmissions to 16% by June 2025, focusing on timely outpatient large-volume paracentesis (LVP) and improved transitions of care (TOC) via nurse navigators.
Methods: This QI project included adults >18 years hospitalized under medical severity diagnosis-related group codes 432, 433, or 434. In August 2024, three primary interventions were implemented: (1) timely LVP scheduling, (2) referral to high-risk discharge clinics, and (3) nurse navigator-led follow-up coordination. An Epic discharge order set was developed to streamline ambulatory lab orders and follow-up appointment scheduling. The target was ≥50% adherence for each intervention. Data was extracted from Vizient and Epic.
Results: In 2024, 474 patients met inclusion criteria and 104 (21.9%) were readmitted within 30 days. Following intervention in August, the average readmission rate fell to 19.3% by December. Monthly unplanned readmissions dropped from nine to seven (October–December), with estimated monthly cost savings of $29,675. However, rates rose to 32.5% in January–February 2025, revealing poor process adherence: only 30% had LVP scheduled, 46% were referred to the high-risk clinic, and 27.6% had nurse navigator coordination.
Discussion: Initial reductions in readmission rates suggest our interventions were effective, but sustainability was a challenge. A rise in readmissions in early 2025 highlighted gaps in process adherence, particularly in TOC through nurse navigators. In response, a dashboard was developed to help nurse navigators identify high-risk patients and proactively coordinate LVP and follow-up appointments with the primary team. As a result, 72% of patients had follow-up in March and 92.9% in April of 2025. A chart review of Oct–Dec 2024 readmissions showed 35% mortality within 3 months, an average MELD of 25, with 59% likely to benefit from palliative care and 18% deemed preventable. Future interventions will encourage early palliative care consults for patients with higher MELD to clarify goals of care and reduce avoidable hospitalizations.
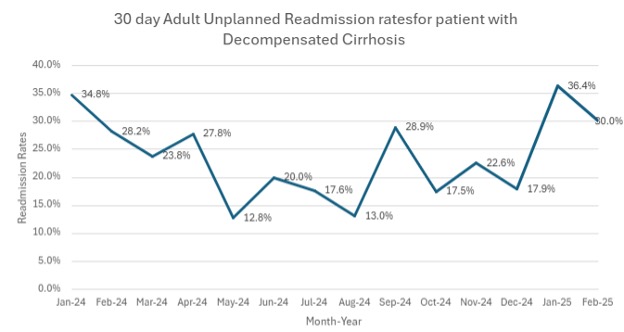
Figure: 30 day adult unplanned readmission rates for patients with decompensated cirrhosis
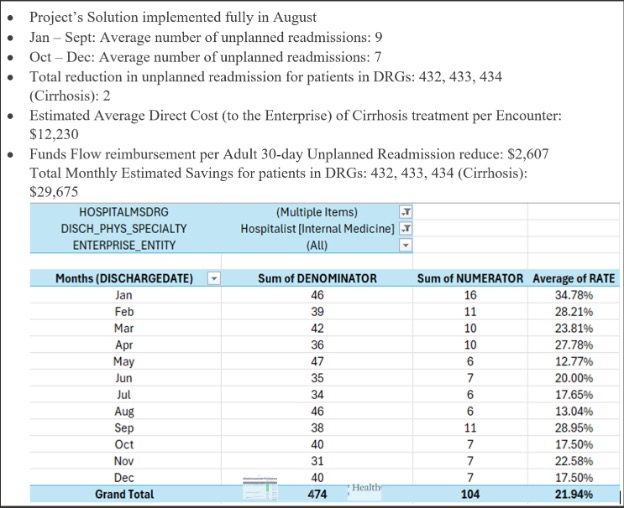
Figure: Return on Investment Following Implementation of Readmission Reduction Interventions in August 2024
Disclosures:
Hannah Darnell indicated no relevant financial relationships.
Nishant Tripathi indicated no relevant financial relationships.
Stephanie Leung indicated no relevant financial relationships.
Elizabeth Wilson indicated no relevant financial relationships.
Jamie Edwards indicated no relevant financial relationships.
Thomas Jackson indicated no relevant financial relationships.
Patricia Santos indicated no relevant financial relationships.
Rani Chikkanna indicated no relevant financial relationships.
Hannah Darnell, DO, Nishant Tripathi, MBBS, Stephanie Leung, MD, Elizabeth Wilson, RN, Jamie Edwards, RN, Thomas Jackson, MHS, Patricia Santos, MD, Rani Chikkanna, MD. P3754 - Navigating Cirrhosis Care: The Impact of Clear Goals and Seamless Transitions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
