Monday Poster Session
Category: Liver
P3743 - Improved Graft Outcomes With Statins in Liver Transplant Recipients With Hepatitis B- or C-Induced Cirrhosis and Rejection
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Karecia Byfield, MBBS
Jefferson Einstein Hospital
Philadelphia, PA
Presenting Author(s)
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Danielle Lewis, MBBS2, Megan Johnson, MBBS3, Kevin Robinson, MBBS2, Maria Lagarde, MD4
1Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA; 2Jefferson Einstein Philadelphia Hospital, Philadelphia, PA; 3Spanish Town Hospital, Kingston, Saint Catherine, Jamaica; 4Einstein Healthcare Network, Philadelphia, PA
Introduction: Statins are commonly used in liver transplant (LT) recipients with cardiovascular indications and are considered safe in this population of patients. Furthermore, statins possess anti-inflammatory and immunomodulatory properties which may confer additional benefits in LT recipients. Previous studies including work by Y.J. Ho et al. suggest that statins may be associated with reduced mortality, graft rejection and hepatocellular carcinoma recurrence, without increased risk of complications. However, despite these benefits, a gap in understanding exists regarding the effect of statin therapy once rejection has occurred. Given the complexity of management of transplant rejection and the need to improve outcomes, our study aims to investigate the impact of statin exposure on transplant rejection outcomes in patients with viral hepatitis-induced cirrhosis.
Methods: We utilized data from the US Collaborative Network-TriNetX to evaluate the impact of statin use on patients aged 18 years and older hospitalized for liver transplant rejection with a history of viral cirrhosis between January 1, 2014 and January 1, 2024 using the relevant ICD-10 codes. Patients were divided into two cohorts: those with concurrent statin use, and those without. Both cohorts were propensity score matched based on demographics and comorbidities such as diabetes, hypertension and kidney disease. They were followed for 30 days post-hospitalization to assess outcomes including graft failure, readmission, ICU admission, acute kidney injury (AKI) and death.
Results: Each cohort consisted of 449 patients after propensity score matching. The mean age was 68 ± 9 years with 67% of the cohort being male. Our analysis revealed that within 30 days post-hospitalization, the cohort without concurrent statin exposure had a significantly higher risk of graft failure (HR: 2.27, 95%CI: 1.70-3.02, p < 0.0001) and readmission (HR:1.16, CI: 1.01-1.34, p 0.04). There was no significant difference in mortality rate, ICU admission and AKI.
Discussion: Concurrent statin exposure in patients hospitalized with liver transplant rejection and a history of hepatitis B or C-induced cirrhosis is associated with a significantly reduced risk of graft failure suggesting a potential protective role of statins outside of known indications. Further prospective cohort studies are needed to explore the effect of statins in the context of liver transplant rejection and further delineate their role as possible adjunctive therapy in post-transplant care.
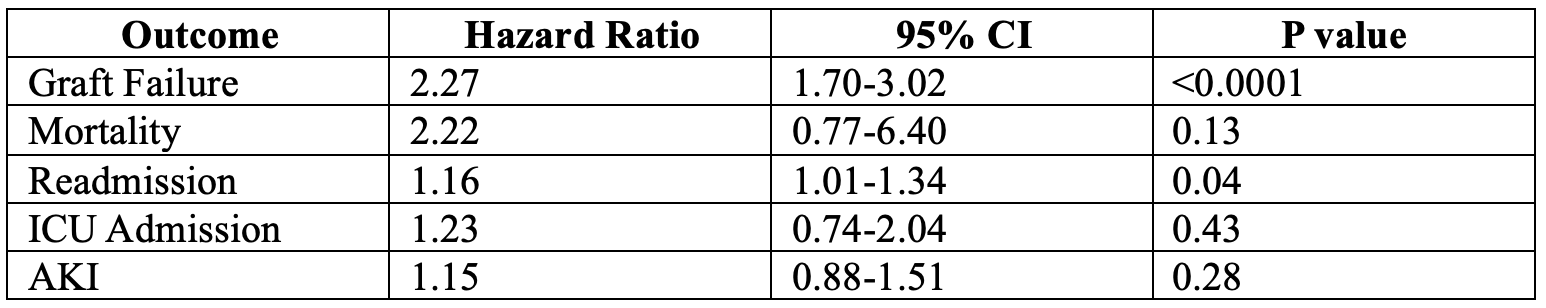
Figure: Table Outlining Clinical Outcomes
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Danielle Lewis indicated no relevant financial relationships.
Megan Johnson indicated no relevant financial relationships.
Kevin Robinson indicated no relevant financial relationships.
Maria Lagarde indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Danielle Lewis, MBBS2, Megan Johnson, MBBS3, Kevin Robinson, MBBS2, Maria Lagarde, MD4. P3743 - Improved Graft Outcomes With Statins in Liver Transplant Recipients With Hepatitis B- or C-Induced Cirrhosis and Rejection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA; 2Jefferson Einstein Philadelphia Hospital, Philadelphia, PA; 3Spanish Town Hospital, Kingston, Saint Catherine, Jamaica; 4Einstein Healthcare Network, Philadelphia, PA
Introduction: Statins are commonly used in liver transplant (LT) recipients with cardiovascular indications and are considered safe in this population of patients. Furthermore, statins possess anti-inflammatory and immunomodulatory properties which may confer additional benefits in LT recipients. Previous studies including work by Y.J. Ho et al. suggest that statins may be associated with reduced mortality, graft rejection and hepatocellular carcinoma recurrence, without increased risk of complications. However, despite these benefits, a gap in understanding exists regarding the effect of statin therapy once rejection has occurred. Given the complexity of management of transplant rejection and the need to improve outcomes, our study aims to investigate the impact of statin exposure on transplant rejection outcomes in patients with viral hepatitis-induced cirrhosis.
Methods: We utilized data from the US Collaborative Network-TriNetX to evaluate the impact of statin use on patients aged 18 years and older hospitalized for liver transplant rejection with a history of viral cirrhosis between January 1, 2014 and January 1, 2024 using the relevant ICD-10 codes. Patients were divided into two cohorts: those with concurrent statin use, and those without. Both cohorts were propensity score matched based on demographics and comorbidities such as diabetes, hypertension and kidney disease. They were followed for 30 days post-hospitalization to assess outcomes including graft failure, readmission, ICU admission, acute kidney injury (AKI) and death.
Results: Each cohort consisted of 449 patients after propensity score matching. The mean age was 68 ± 9 years with 67% of the cohort being male. Our analysis revealed that within 30 days post-hospitalization, the cohort without concurrent statin exposure had a significantly higher risk of graft failure (HR: 2.27, 95%CI: 1.70-3.02, p < 0.0001) and readmission (HR:1.16, CI: 1.01-1.34, p 0.04). There was no significant difference in mortality rate, ICU admission and AKI.
Discussion: Concurrent statin exposure in patients hospitalized with liver transplant rejection and a history of hepatitis B or C-induced cirrhosis is associated with a significantly reduced risk of graft failure suggesting a potential protective role of statins outside of known indications. Further prospective cohort studies are needed to explore the effect of statins in the context of liver transplant rejection and further delineate their role as possible adjunctive therapy in post-transplant care.
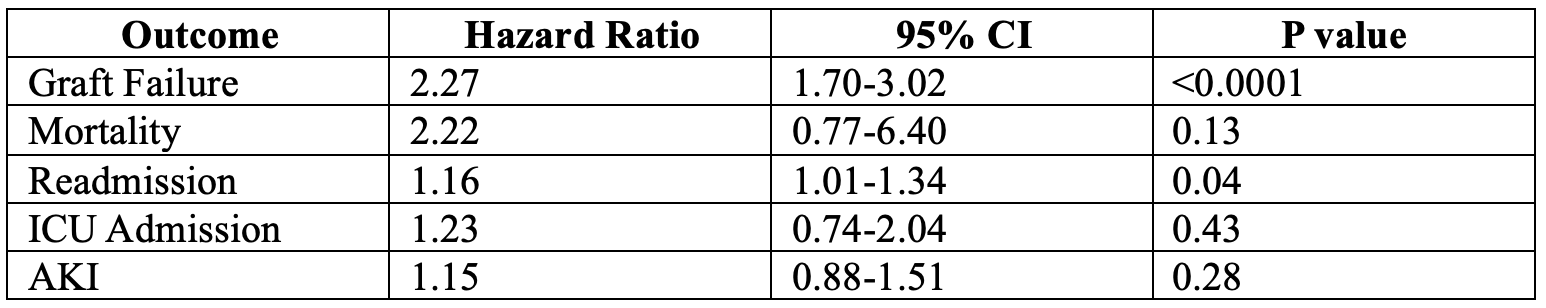
Figure: Table Outlining Clinical Outcomes
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Danielle Lewis indicated no relevant financial relationships.
Megan Johnson indicated no relevant financial relationships.
Kevin Robinson indicated no relevant financial relationships.
Maria Lagarde indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Danielle Lewis, MBBS2, Megan Johnson, MBBS3, Kevin Robinson, MBBS2, Maria Lagarde, MD4. P3743 - Improved Graft Outcomes With Statins in Liver Transplant Recipients With Hepatitis B- or C-Induced Cirrhosis and Rejection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
