Monday Poster Session
Category: Liver
P3739 - Rates of Portal Venous Thrombosis in Cirrhotics With or Without Clotting Disorders: A 7-Year Nationwide Study on Rates of PVT
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Andrej M. Sodoma, DO
Northwell Health
Lake Grove, NY
Presenting Author(s)
Andrej M. Sodoma, DO1, James Pellegrini, MD2, Samuel Greenberg, BA3, Tayab Kirmani, MD4, Jaspreet Singh, MD4
1Northwell Health, Lake Grove, NY; 2Nassau University Medical Center, East Meadow, NY; 3Stony Brook Medicine, Stony Brook, NY; 4Northwell Health, Bay Shore, NY
Introduction: Cirrhotics can be both hypercoagulable and hypocoagulable, with various reasons for either state. A common thrombotic event in this group is portal venous thrombosis (PVT)—many reasons for this to occur. Current research states that inherited hemostatic disorders do not predict the development of PVT. In this study, various thrombophilias were analyzed: activated protein C resistance (APCR), prothrombin gene mutation (PTM), paroxysmal nocturnal hemoglobinuria (PNH), other thrombophilia (OT), and disseminated intravascular coagulation (DIC).
Methods: The National Inpatient Sample (NIS) from 2015-2021 was used to identify patients diagnosed with cirrhosis with or without thrombophilias using the International Classification of Disease (ICD) 10 codes. Records were weighted per the NIS algorithm to produce accurate population estimates. Cirrhotic patients with or without thrombophilia were analyzed for baseline characteristics. Various primary outcomes were analyzed, which included PVT, death, acute kidney injury (AKI), acute myocardial infarction (AMI), shock, and composite outcomes. Secondary outcomes were analyzed, which included transjugular intrahepatic portosystemic shunt (TIPS) during hospitalization, length of stay (LOS), and hospital charges.
Results: A weighted total of 2,391,389 patients with cirrhosis without a known coagulation pathology, 4,075 patients with cirrhosis and APCR, 425 patients with cirrhosis and PTM, 175 patients with cirrhosis and PNH, 14,155 patients with cirrhosis and DIC. Cirrhotic patients with PTM had the highest odds of developing PVT (OR (95% CI): 2.848 (2.24-3.62) APCR, 8.801 (5.471-14.157) PTM, 4.286 (3.708-4.955) OT, 2.904 (0.908-9.286) PNH, 1.744 (1.49-2.04) DIC). Cirrhotic patients with DIC had higher odds of death (OR (95% CI): 24.748 (22.82-26.839) DIC), AKI (7.458 (6.82-8.155), AMI (3.205 (2.801-3.667)), shock (21.454 (19.793-23.254)), and overall worse outcomes (15.912 (14.127-17.922)). Secondary outcomes were analyzed, which included higher odds of TIPS during hospitalization for cirrhotic patients with DIC (1.913 (1.369-2.674)). In turn, cirrhotic patients with DIC had greater lengths of stay (LOS) (5.270 (4.759-5.781)) and greater hospital charges (168463 (147901-189024)).
Discussion: Patients with cirrhosis and thrombophilic disorders had higher odds of PVT, which supports alterations in coagulation factors as predictive factors in the development of PVT.
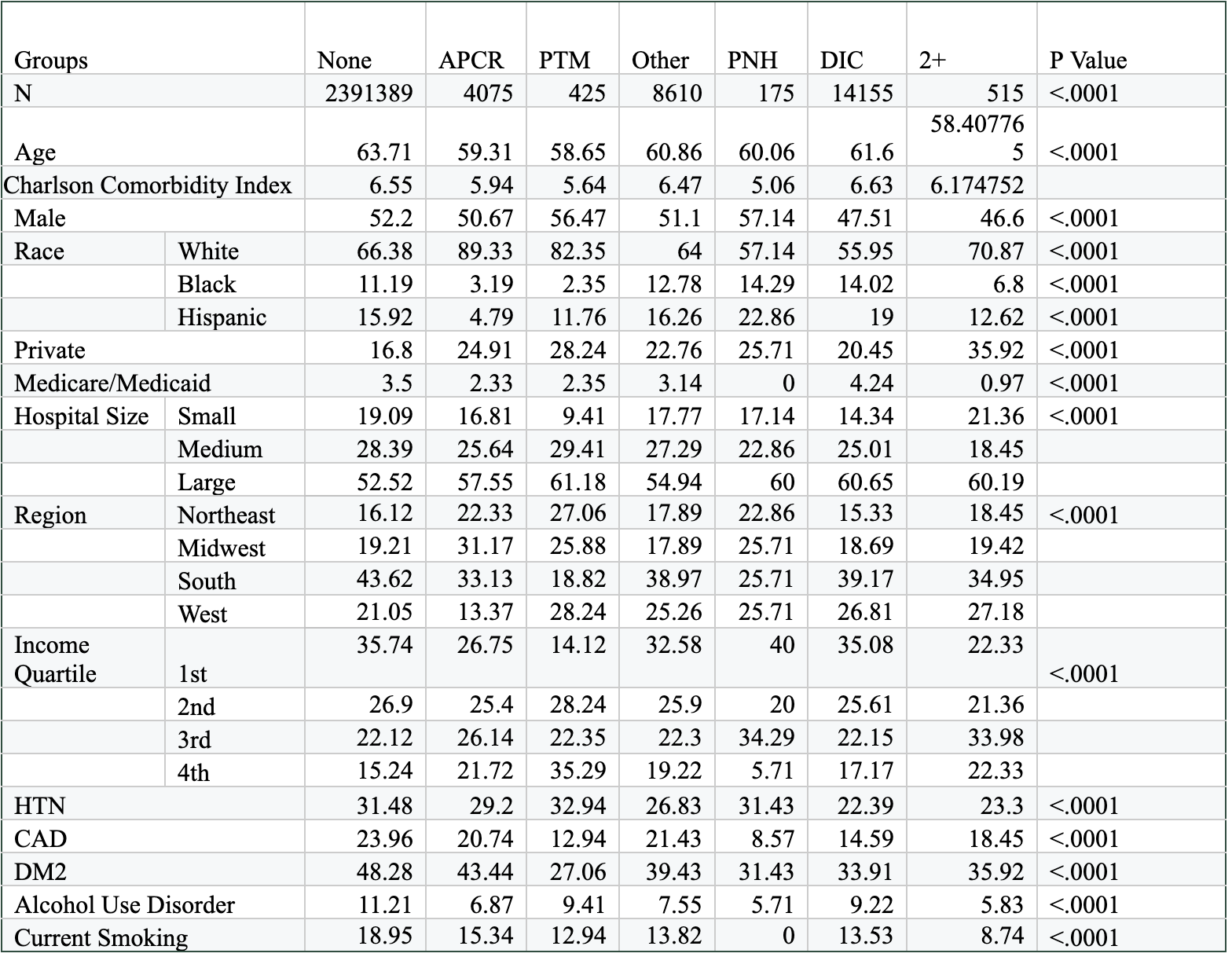
Figure: Baseline Characteristics of Patients Admitted for PVT in Cirrhotics Stratified by Clotting Disorder.
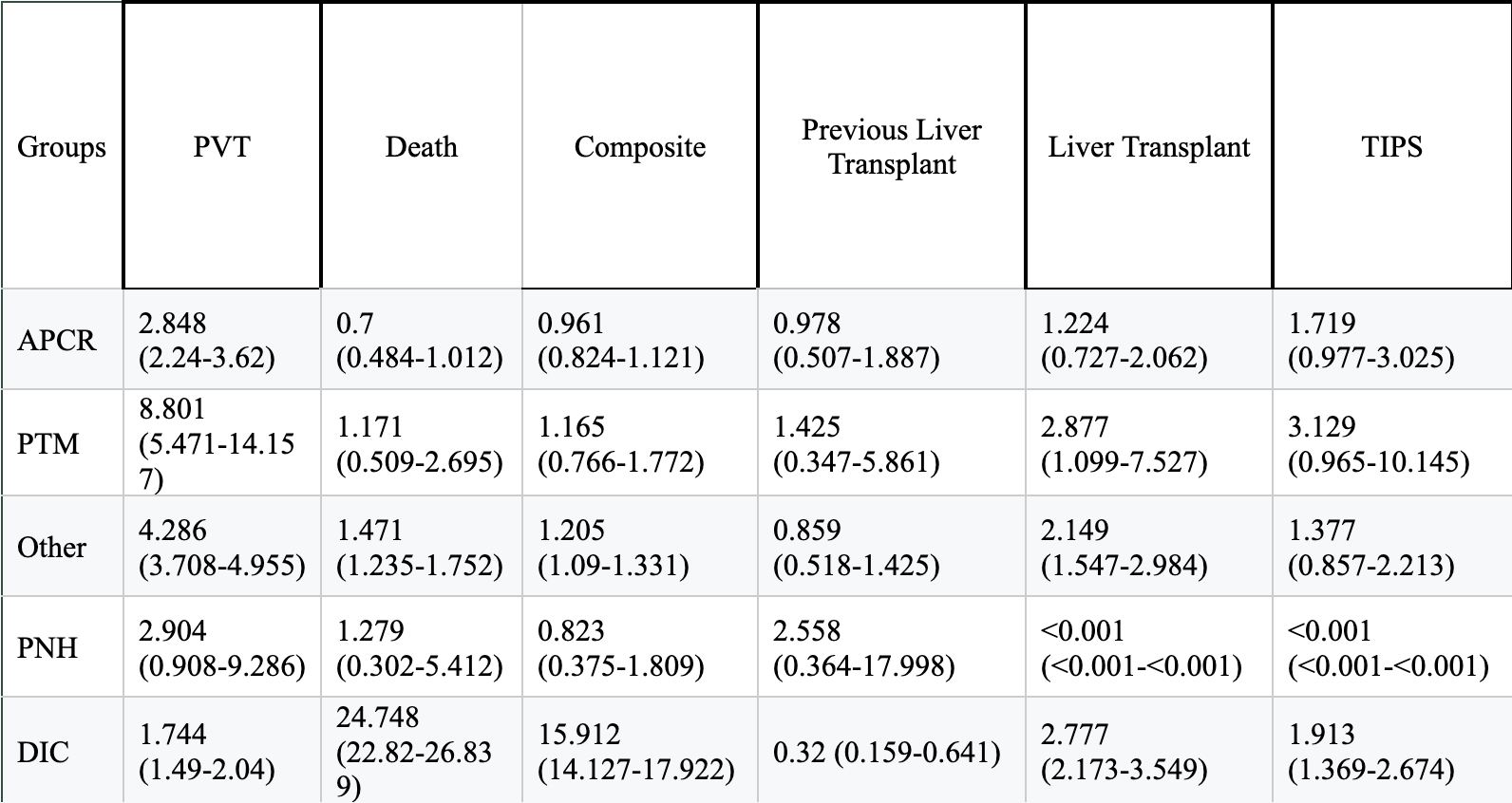
Figure: Outcomes for Patients Admitted for PVT in Cirrhotics Stratified by Clotting Disorder
Disclosures:
Andrej Sodoma indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Samuel Greenberg indicated no relevant financial relationships.
Tayab Kirmani indicated no relevant financial relationships.
Jaspreet Singh indicated no relevant financial relationships.
Andrej M. Sodoma, DO1, James Pellegrini, MD2, Samuel Greenberg, BA3, Tayab Kirmani, MD4, Jaspreet Singh, MD4. P3739 - Rates of Portal Venous Thrombosis in Cirrhotics With or Without Clotting Disorders: A 7-Year Nationwide Study on Rates of PVT, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Lake Grove, NY; 2Nassau University Medical Center, East Meadow, NY; 3Stony Brook Medicine, Stony Brook, NY; 4Northwell Health, Bay Shore, NY
Introduction: Cirrhotics can be both hypercoagulable and hypocoagulable, with various reasons for either state. A common thrombotic event in this group is portal venous thrombosis (PVT)—many reasons for this to occur. Current research states that inherited hemostatic disorders do not predict the development of PVT. In this study, various thrombophilias were analyzed: activated protein C resistance (APCR), prothrombin gene mutation (PTM), paroxysmal nocturnal hemoglobinuria (PNH), other thrombophilia (OT), and disseminated intravascular coagulation (DIC).
Methods: The National Inpatient Sample (NIS) from 2015-2021 was used to identify patients diagnosed with cirrhosis with or without thrombophilias using the International Classification of Disease (ICD) 10 codes. Records were weighted per the NIS algorithm to produce accurate population estimates. Cirrhotic patients with or without thrombophilia were analyzed for baseline characteristics. Various primary outcomes were analyzed, which included PVT, death, acute kidney injury (AKI), acute myocardial infarction (AMI), shock, and composite outcomes. Secondary outcomes were analyzed, which included transjugular intrahepatic portosystemic shunt (TIPS) during hospitalization, length of stay (LOS), and hospital charges.
Results: A weighted total of 2,391,389 patients with cirrhosis without a known coagulation pathology, 4,075 patients with cirrhosis and APCR, 425 patients with cirrhosis and PTM, 175 patients with cirrhosis and PNH, 14,155 patients with cirrhosis and DIC. Cirrhotic patients with PTM had the highest odds of developing PVT (OR (95% CI): 2.848 (2.24-3.62) APCR, 8.801 (5.471-14.157) PTM, 4.286 (3.708-4.955) OT, 2.904 (0.908-9.286) PNH, 1.744 (1.49-2.04) DIC). Cirrhotic patients with DIC had higher odds of death (OR (95% CI): 24.748 (22.82-26.839) DIC), AKI (7.458 (6.82-8.155), AMI (3.205 (2.801-3.667)), shock (21.454 (19.793-23.254)), and overall worse outcomes (15.912 (14.127-17.922)). Secondary outcomes were analyzed, which included higher odds of TIPS during hospitalization for cirrhotic patients with DIC (1.913 (1.369-2.674)). In turn, cirrhotic patients with DIC had greater lengths of stay (LOS) (5.270 (4.759-5.781)) and greater hospital charges (168463 (147901-189024)).
Discussion: Patients with cirrhosis and thrombophilic disorders had higher odds of PVT, which supports alterations in coagulation factors as predictive factors in the development of PVT.
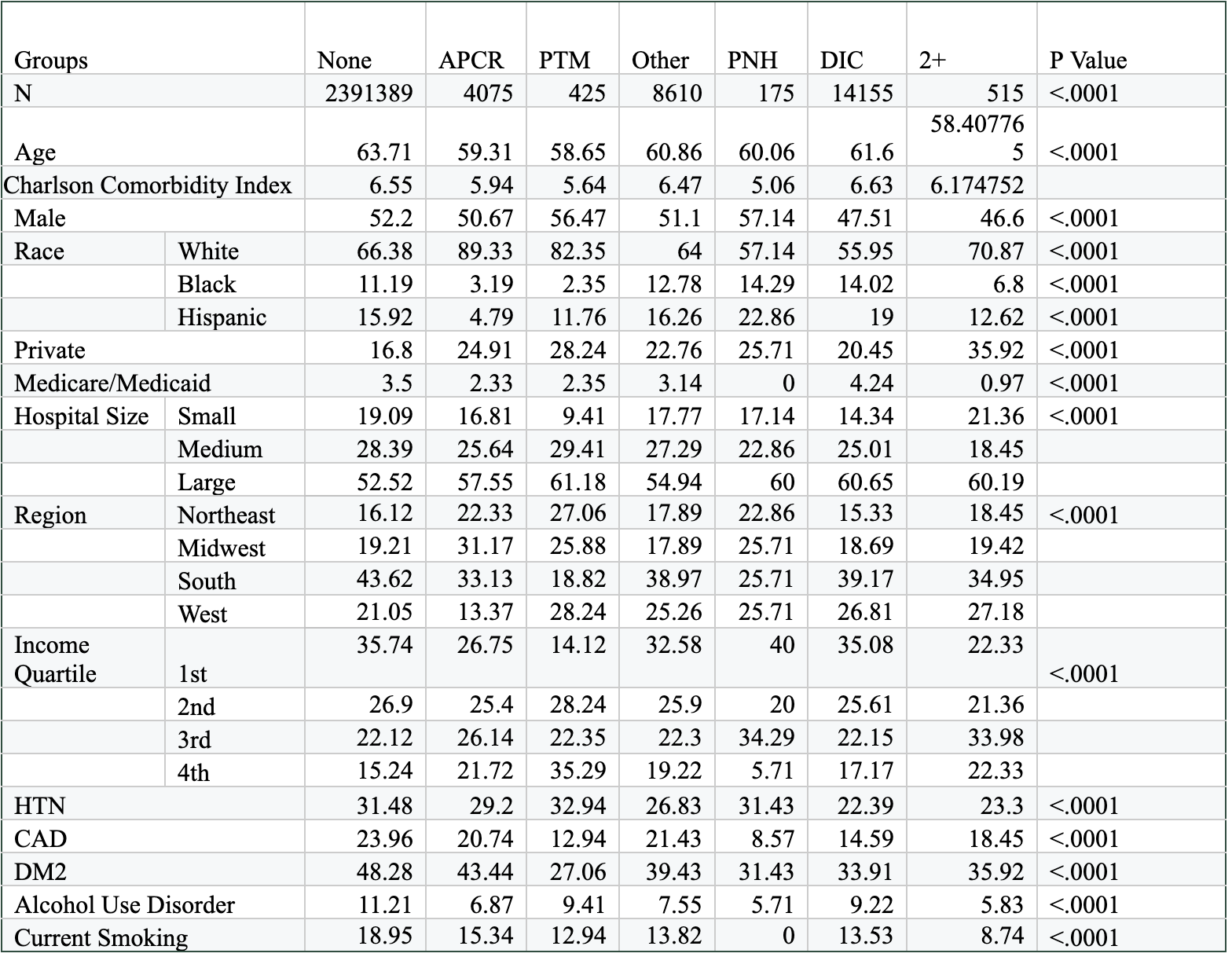
Figure: Baseline Characteristics of Patients Admitted for PVT in Cirrhotics Stratified by Clotting Disorder.
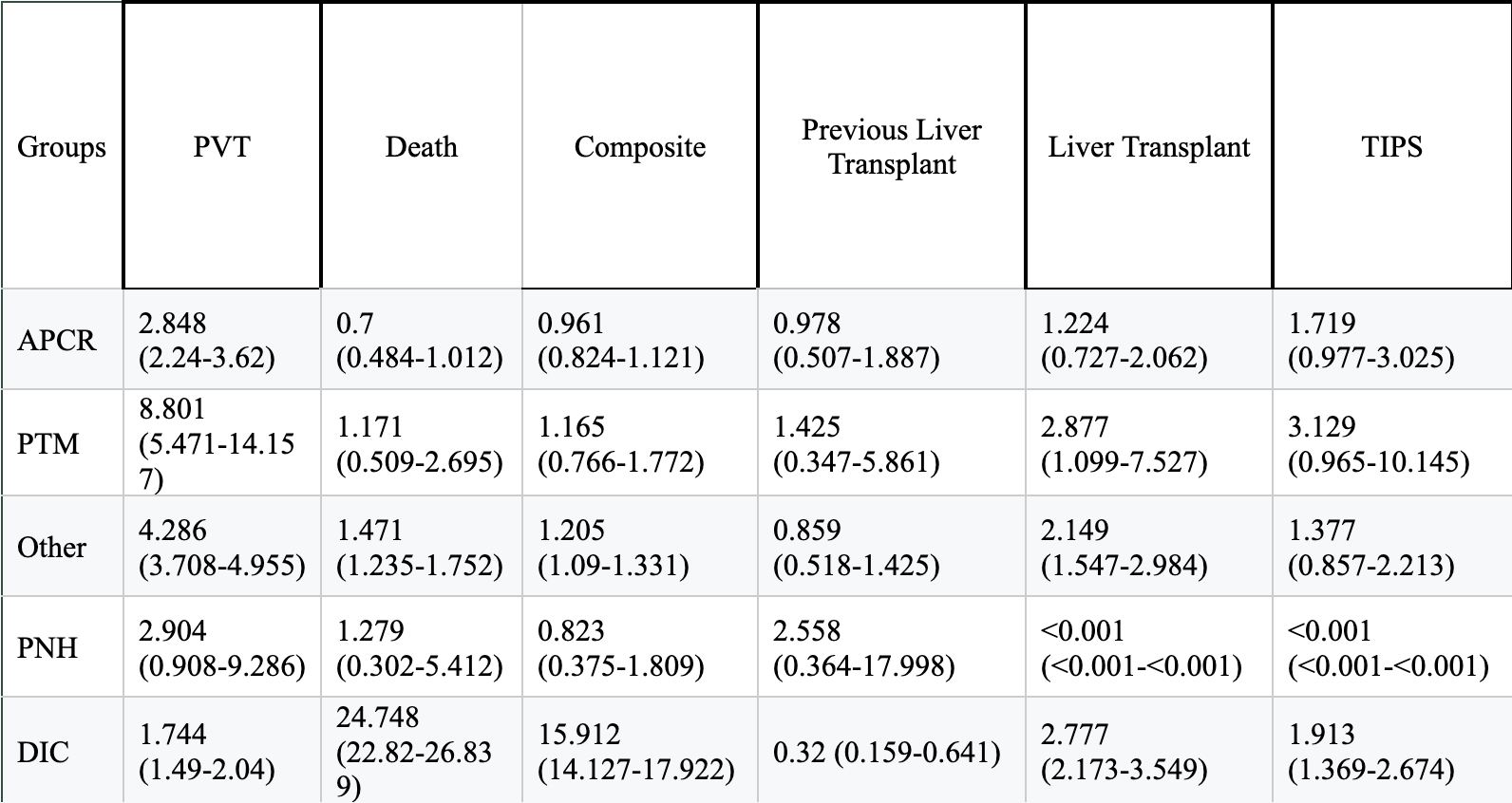
Figure: Outcomes for Patients Admitted for PVT in Cirrhotics Stratified by Clotting Disorder
Disclosures:
Andrej Sodoma indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Samuel Greenberg indicated no relevant financial relationships.
Tayab Kirmani indicated no relevant financial relationships.
Jaspreet Singh indicated no relevant financial relationships.
Andrej M. Sodoma, DO1, James Pellegrini, MD2, Samuel Greenberg, BA3, Tayab Kirmani, MD4, Jaspreet Singh, MD4. P3739 - Rates of Portal Venous Thrombosis in Cirrhotics With or Without Clotting Disorders: A 7-Year Nationwide Study on Rates of PVT, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

