Monday Poster Session
Category: Liver
P3738 - Characteristics and Inpatient Outcomes of Patients With Autoimmune Hepatitis-Primary Biliary Cholangitis Overlap Syndrome vs Autoimmune Hepatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Medha Rajamanuri, MD (she/her/hers)
Medha Rajamanuri
Springfield, IL
Presenting Author(s)
Medha Rajamanuri, MD1, Sai Shanmukha Sreeram Pannala, MD2, Muaataz Azzawi, MD3, Meher Garg, 3, Uday Sankar Akash Vankayala, MBBS2, Saif Yasin, DO2, Ramprasad Jegadeesan, MD4
1Medha Rajamanuri, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3Southern Illinois University, Springfield, IL; 4Ramprasad Jegadeesan, Cumming, GA
Introduction: Primary Biliary Cholangitis (PBC) and Autoimmune Hepatitis (AIH) are autoimmune liver diseases with distinct clinical features. However, there is a subset of patients who present with an overlap syndrome of both conditions, termed AIH-PBC overlap syndrome. We aim to study the clinical outcomes of patients with AIH-PBC overlap syndrome compared to those with only AIH alone.
Methods: This is a retrospective cohort study using National inpatient sample (2016-2020). We analyzed mortality, hepatic encephalopathy (HE), ascites, variceal upper gastrointestinal bleeding (VUGIB), non-variceal upper gastrointestinal bleeding (NVUGIB), lower gastrointestinal bleeding (LGIB), pancreatitis, shock, heart failure, and acute kidney injury (AKI). We compared baseline characteristics including age, sex, Charlson Comorbidity Index, race, median household income, insurance type, liver transplant recipient status, alcohol-related liver disease, chronic viral hepatitis, and metabolic dysfunction-associated steatotic liver disease (MASLD).
Results: Among AIH patients (n=114490), 4.20% (n=5640) had AIH-PBC overlap syndrome. AIH-PBC patients were older (mean age: 59.3 vs. 56.5 years) and had more females (85.5% vs. 77%). They had a higher Charlson Comorbidity Index. No significant differences in other baseline characteristics. Adjusted analysis showed no mortality difference (OR: 0.91, p = 0.605). AIH-PBC had higher risk of ascites (OR: 1.75, p = 0.001) and variceal GI bleed (OR: 2.13, p = 0.001). Higher risk of shock (OR: 1.61, p = 0.006), and AKI (OR: 1.22, p = 0.007). No significant difference in non-variceal upper GI bleed (OR: 1.28, p = 0.34).
Discussion: Patients with AIH-PBC overlap syndrome exhibit a distinct clinical profile compared to those with only AIH, with a higher burden of comorbidities. These patients are at higher risk of complications including ascites, variceal gastrointestinal bleeding, shock, and AKI. Recognition of these baseline differences and associated outcomes is essential for tailored management strategies to optimize outcomes and reduce morbidity in this patient population.
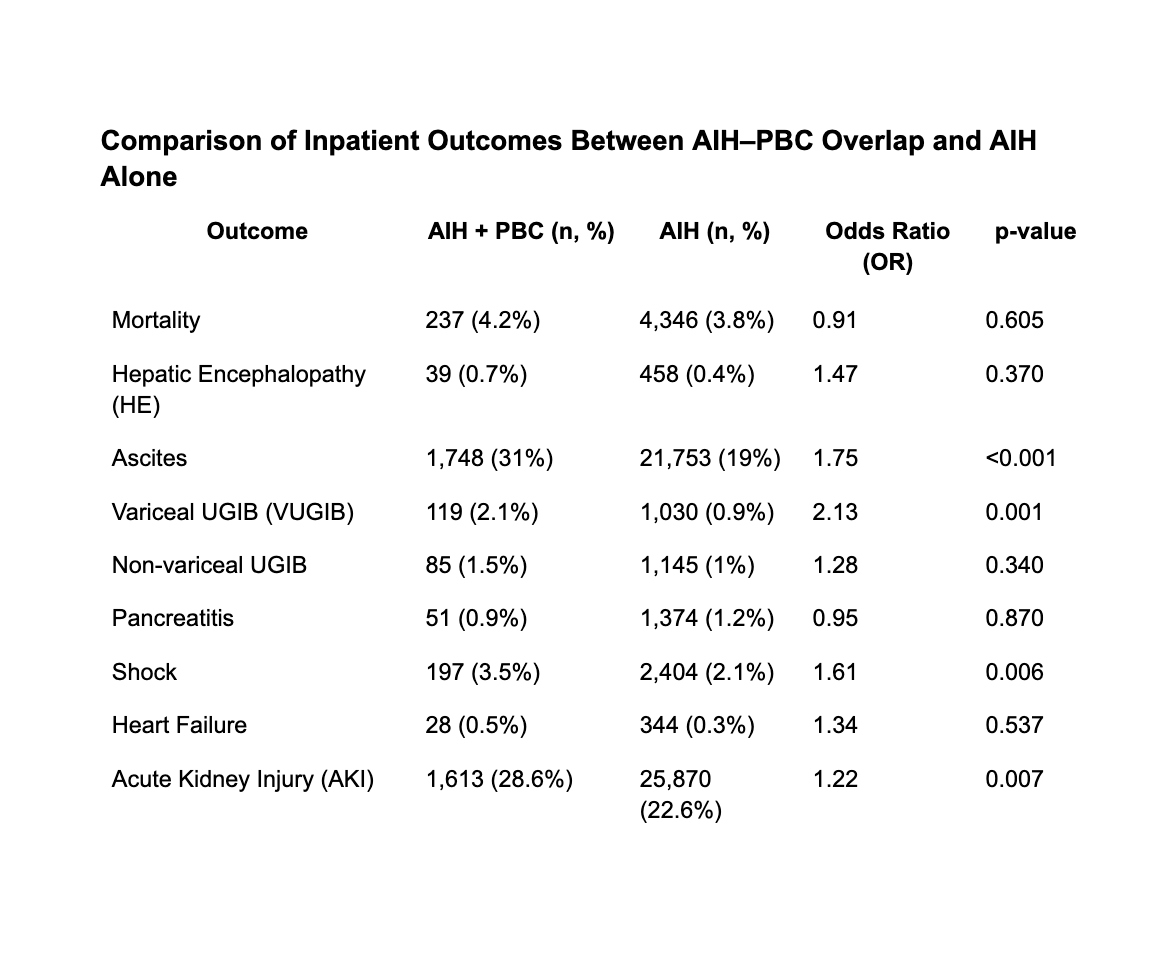
Figure: Comparison of Inpatient Outcomes Between AIH–PBC Overlap and AIH Alone
Disclosures:
Medha Rajamanuri indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Muaataz Azzawi indicated no relevant financial relationships.
Meher Garg indicated no relevant financial relationships.
Uday Sankar Akash Vankayala indicated no relevant financial relationships.
Saif Yasin indicated no relevant financial relationships.
Ramprasad Jegadeesan indicated no relevant financial relationships.
Medha Rajamanuri, MD1, Sai Shanmukha Sreeram Pannala, MD2, Muaataz Azzawi, MD3, Meher Garg, 3, Uday Sankar Akash Vankayala, MBBS2, Saif Yasin, DO2, Ramprasad Jegadeesan, MD4. P3738 - Characteristics and Inpatient Outcomes of Patients With Autoimmune Hepatitis-Primary Biliary Cholangitis Overlap Syndrome vs Autoimmune Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medha Rajamanuri, Springfield, IL; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3Southern Illinois University, Springfield, IL; 4Ramprasad Jegadeesan, Cumming, GA
Introduction: Primary Biliary Cholangitis (PBC) and Autoimmune Hepatitis (AIH) are autoimmune liver diseases with distinct clinical features. However, there is a subset of patients who present with an overlap syndrome of both conditions, termed AIH-PBC overlap syndrome. We aim to study the clinical outcomes of patients with AIH-PBC overlap syndrome compared to those with only AIH alone.
Methods: This is a retrospective cohort study using National inpatient sample (2016-2020). We analyzed mortality, hepatic encephalopathy (HE), ascites, variceal upper gastrointestinal bleeding (VUGIB), non-variceal upper gastrointestinal bleeding (NVUGIB), lower gastrointestinal bleeding (LGIB), pancreatitis, shock, heart failure, and acute kidney injury (AKI). We compared baseline characteristics including age, sex, Charlson Comorbidity Index, race, median household income, insurance type, liver transplant recipient status, alcohol-related liver disease, chronic viral hepatitis, and metabolic dysfunction-associated steatotic liver disease (MASLD).
Results: Among AIH patients (n=114490), 4.20% (n=5640) had AIH-PBC overlap syndrome. AIH-PBC patients were older (mean age: 59.3 vs. 56.5 years) and had more females (85.5% vs. 77%). They had a higher Charlson Comorbidity Index. No significant differences in other baseline characteristics. Adjusted analysis showed no mortality difference (OR: 0.91, p = 0.605). AIH-PBC had higher risk of ascites (OR: 1.75, p = 0.001) and variceal GI bleed (OR: 2.13, p = 0.001). Higher risk of shock (OR: 1.61, p = 0.006), and AKI (OR: 1.22, p = 0.007). No significant difference in non-variceal upper GI bleed (OR: 1.28, p = 0.34).
Discussion: Patients with AIH-PBC overlap syndrome exhibit a distinct clinical profile compared to those with only AIH, with a higher burden of comorbidities. These patients are at higher risk of complications including ascites, variceal gastrointestinal bleeding, shock, and AKI. Recognition of these baseline differences and associated outcomes is essential for tailored management strategies to optimize outcomes and reduce morbidity in this patient population.
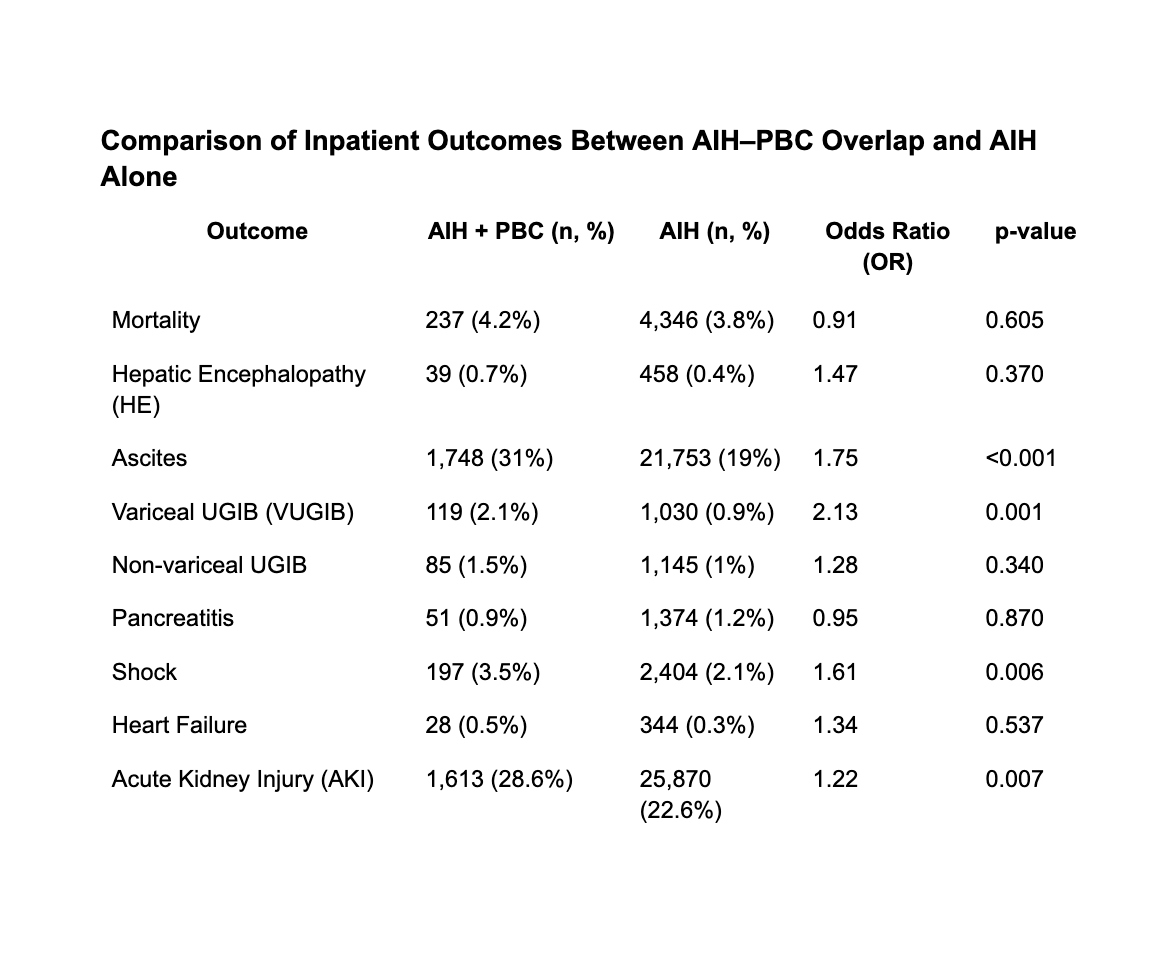
Figure: Comparison of Inpatient Outcomes Between AIH–PBC Overlap and AIH Alone
Disclosures:
Medha Rajamanuri indicated no relevant financial relationships.
Sai Shanmukha Sreeram Pannala indicated no relevant financial relationships.
Muaataz Azzawi indicated no relevant financial relationships.
Meher Garg indicated no relevant financial relationships.
Uday Sankar Akash Vankayala indicated no relevant financial relationships.
Saif Yasin indicated no relevant financial relationships.
Ramprasad Jegadeesan indicated no relevant financial relationships.
Medha Rajamanuri, MD1, Sai Shanmukha Sreeram Pannala, MD2, Muaataz Azzawi, MD3, Meher Garg, 3, Uday Sankar Akash Vankayala, MBBS2, Saif Yasin, DO2, Ramprasad Jegadeesan, MD4. P3738 - Characteristics and Inpatient Outcomes of Patients With Autoimmune Hepatitis-Primary Biliary Cholangitis Overlap Syndrome vs Autoimmune Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
