Monday Poster Session
Category: Liver
P3733 - Portal Hypertension Mortality in the United States (1999–2023): Insights from the CDC WONDER Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HH
Het Hirpara, MBBS (he/him/his)
C.U.Shah Medical College and Hospital
Surendranagar, Gujarat, India
Presenting Author(s)
Raymond Haward, MBBS1, Nikhil Duseja, MBBS2, Het Hirpara, MBBS3, Rachel Haward, MBBS4
1Vydehi Institute of Medical Sciences and Research Centre, Bangalore, Karnataka, India; 2Karachi Medical & Dental College, Karachi, Sindh, Pakistan; 3C.U.Shah Medical College and Hospital, Surendranagar, Gujarat, India; 4KVG Medical College & Hospital, Sullia, Karnataka, India
Introduction: Portal hypertension, a key complication of advanced liver disease, contributes to variceal bleeding and encephalopathy. Despite advances in cirrhosis care, national mortality trends remain undercharacterized. This study analyzes U.S. mortality data from 1999 to 2023 to assess long-term trends and identify high-risk populations, aiming to inform targeted liver disease management strategies.
Methods: We performed a retrospective analysis using CDC WONDER data to identify portal hypertension deaths (ICD-10: K76.6) from 1999–2023. Age-adjusted mortality rates (AAMRs) were examined by year and stratified by sex, race/ethnicity, region, and urban–rural status. Joinpoint regression estimated Annual and Average Annual Percent Change (APC, AAPC); p < 0.05 was considered significant. Ethical review was not required.
Results: A total of 34,551 portal hypertension deaths occurred from 1999 to 2023. Overall, AAMRs rose from 0.6 in 1999 to 0.7 in 2023 (AAPC = 0.58; 95% CI: -0.08 to 1.33). Men had higher AAMR compared to women, while women had a higher rate of increase (AAPC = 2.33*; 95% CI: 1.02 to 3.69). Region-wise analysis showed western regions had the highest AAPC (AAPC = 2.68*; 95% CI: 1.82 to 3.49), followed by the South (AAPC = 2.48*; 95% CI: 1.82 to 3.15). and Midwest (AAPC = 1.72*; 95% CI: 0.93 to 2.50), and the lowest being Northeast (AAPC = 0.29; 95% CI: -0.63 to 1.21). From 1999 to 2020, rural areas had higher average AAMR and had a higher rate of increase (AAPC = 2.22*; 95% CI: 1.13 to 3.23).
Discussion: Portal hypertension mortality in the U.S. declined or plateaued in the early 2000s but began rising around 2015, paralleling national trends in cirrhosis. Males consistently had higher mortality, likely due to greater alcohol-related liver disease, though rates are now rising in both sexes. The sharp increase in nonalcoholic fatty liver disease (NAFLD) mortality—especially among women—and a resurgence in alcohol-associated cirrhosis appear to be key drivers of this trend. In contrast, hepatitis C-related cirrhosis has declined following improved antiviral therapies post-2014.
Geographically, the South reports the highest mortality, and rural areas exhibit higher and more rapidly rising mortality than urban regions, likely due to limited access to hepatology care, delayed diagnoses, and lower transplant availability. These findings point to the need for targeted interventions to combat NAFLD and alcohol misuse and to expand liver care access in vulnerable regions.
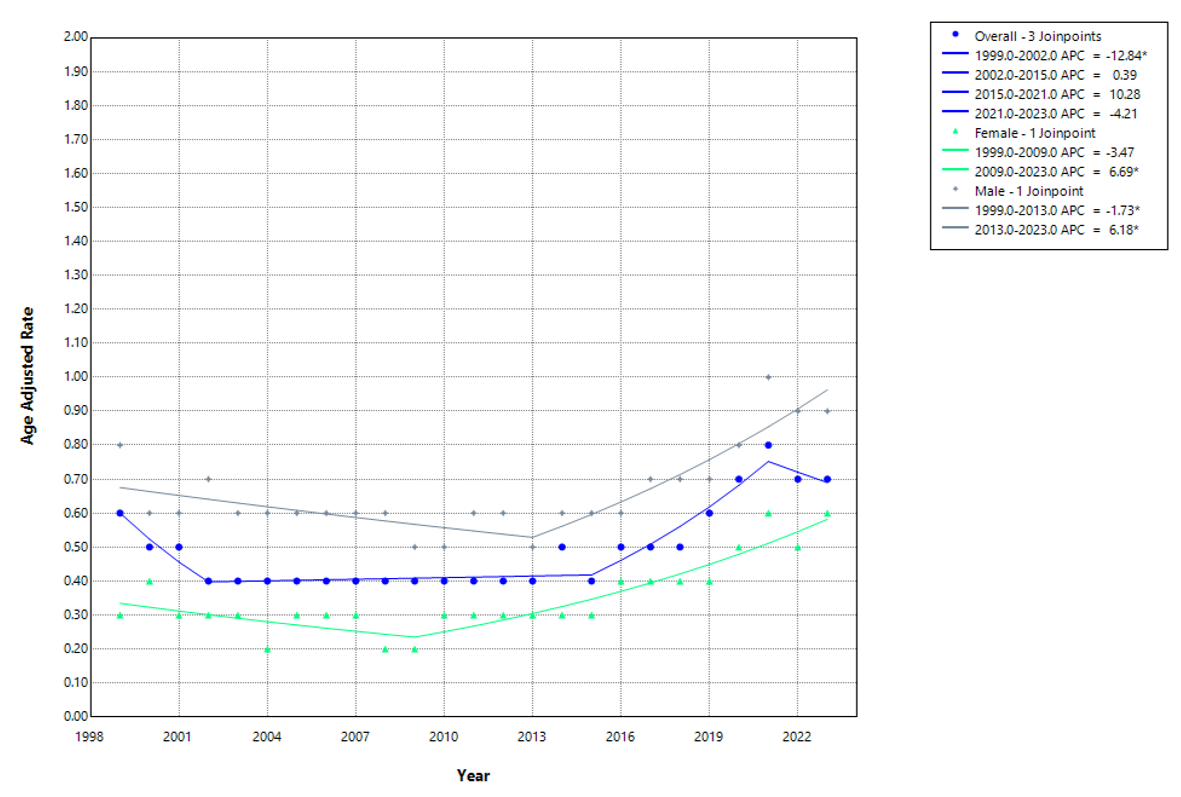
Figure: Temporal Trends in Portal Hypertension Mortality in the U.S.: Insights from CDC WONDER Database, 1999–2023
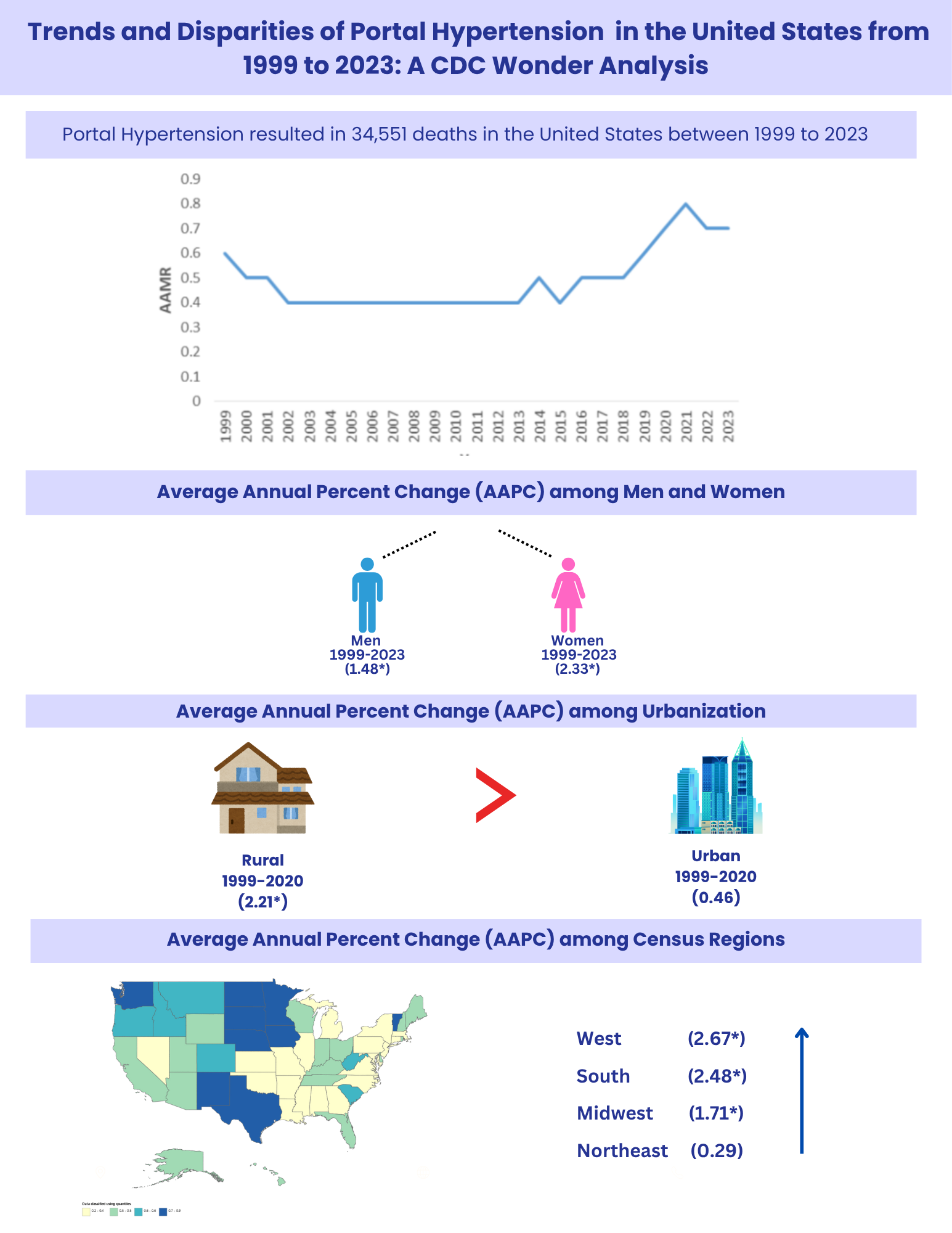
Figure: Graphical Analysis of Overall and Gender-Specific Trends in Portal Hypertension Mortality (1999–2023)
Disclosures:
Raymond Haward indicated no relevant financial relationships.
Nikhil Duseja indicated no relevant financial relationships.
Het Hirpara indicated no relevant financial relationships.
Rachel Haward indicated no relevant financial relationships.
Raymond Haward, MBBS1, Nikhil Duseja, MBBS2, Het Hirpara, MBBS3, Rachel Haward, MBBS4. P3733 - Portal Hypertension Mortality in the United States (1999–2023): Insights from the CDC WONDER Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Vydehi Institute of Medical Sciences and Research Centre, Bangalore, Karnataka, India; 2Karachi Medical & Dental College, Karachi, Sindh, Pakistan; 3C.U.Shah Medical College and Hospital, Surendranagar, Gujarat, India; 4KVG Medical College & Hospital, Sullia, Karnataka, India
Introduction: Portal hypertension, a key complication of advanced liver disease, contributes to variceal bleeding and encephalopathy. Despite advances in cirrhosis care, national mortality trends remain undercharacterized. This study analyzes U.S. mortality data from 1999 to 2023 to assess long-term trends and identify high-risk populations, aiming to inform targeted liver disease management strategies.
Methods: We performed a retrospective analysis using CDC WONDER data to identify portal hypertension deaths (ICD-10: K76.6) from 1999–2023. Age-adjusted mortality rates (AAMRs) were examined by year and stratified by sex, race/ethnicity, region, and urban–rural status. Joinpoint regression estimated Annual and Average Annual Percent Change (APC, AAPC); p < 0.05 was considered significant. Ethical review was not required.
Results: A total of 34,551 portal hypertension deaths occurred from 1999 to 2023. Overall, AAMRs rose from 0.6 in 1999 to 0.7 in 2023 (AAPC = 0.58; 95% CI: -0.08 to 1.33). Men had higher AAMR compared to women, while women had a higher rate of increase (AAPC = 2.33*; 95% CI: 1.02 to 3.69). Region-wise analysis showed western regions had the highest AAPC (AAPC = 2.68*; 95% CI: 1.82 to 3.49), followed by the South (AAPC = 2.48*; 95% CI: 1.82 to 3.15). and Midwest (AAPC = 1.72*; 95% CI: 0.93 to 2.50), and the lowest being Northeast (AAPC = 0.29; 95% CI: -0.63 to 1.21). From 1999 to 2020, rural areas had higher average AAMR and had a higher rate of increase (AAPC = 2.22*; 95% CI: 1.13 to 3.23).
Discussion: Portal hypertension mortality in the U.S. declined or plateaued in the early 2000s but began rising around 2015, paralleling national trends in cirrhosis. Males consistently had higher mortality, likely due to greater alcohol-related liver disease, though rates are now rising in both sexes. The sharp increase in nonalcoholic fatty liver disease (NAFLD) mortality—especially among women—and a resurgence in alcohol-associated cirrhosis appear to be key drivers of this trend. In contrast, hepatitis C-related cirrhosis has declined following improved antiviral therapies post-2014.
Geographically, the South reports the highest mortality, and rural areas exhibit higher and more rapidly rising mortality than urban regions, likely due to limited access to hepatology care, delayed diagnoses, and lower transplant availability. These findings point to the need for targeted interventions to combat NAFLD and alcohol misuse and to expand liver care access in vulnerable regions.
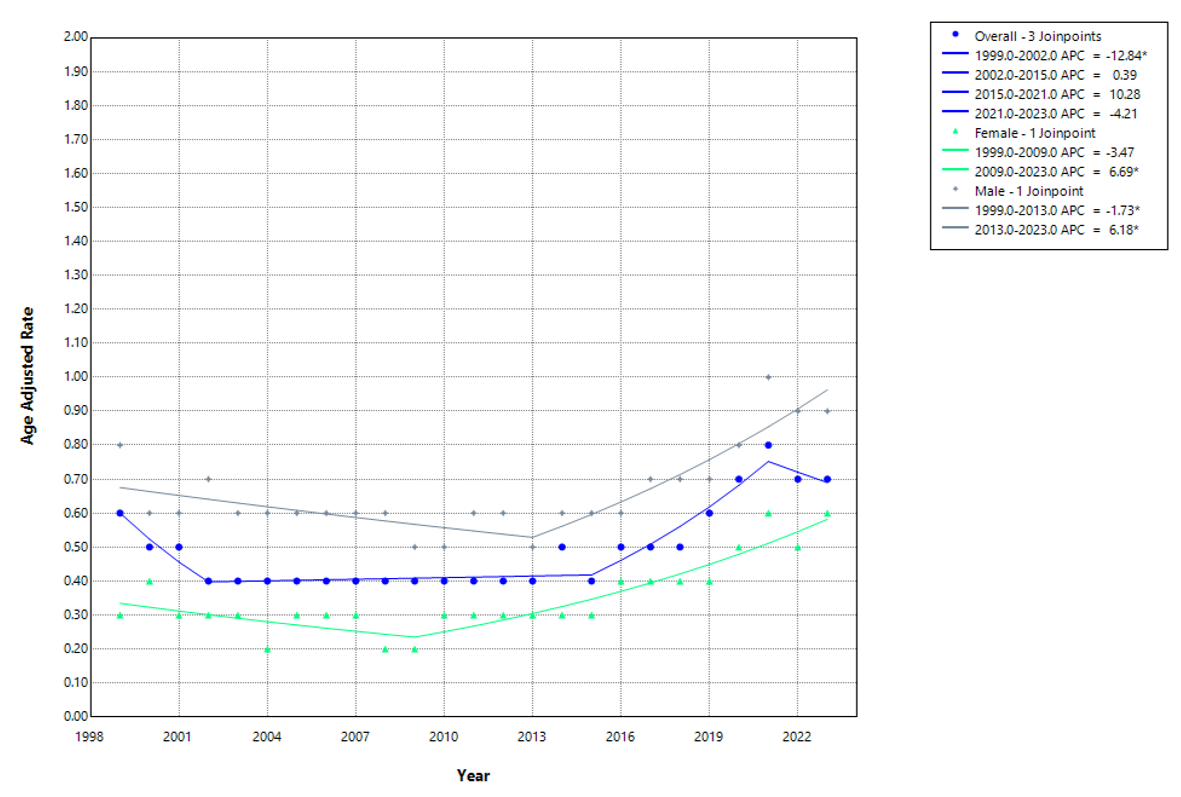
Figure: Temporal Trends in Portal Hypertension Mortality in the U.S.: Insights from CDC WONDER Database, 1999–2023
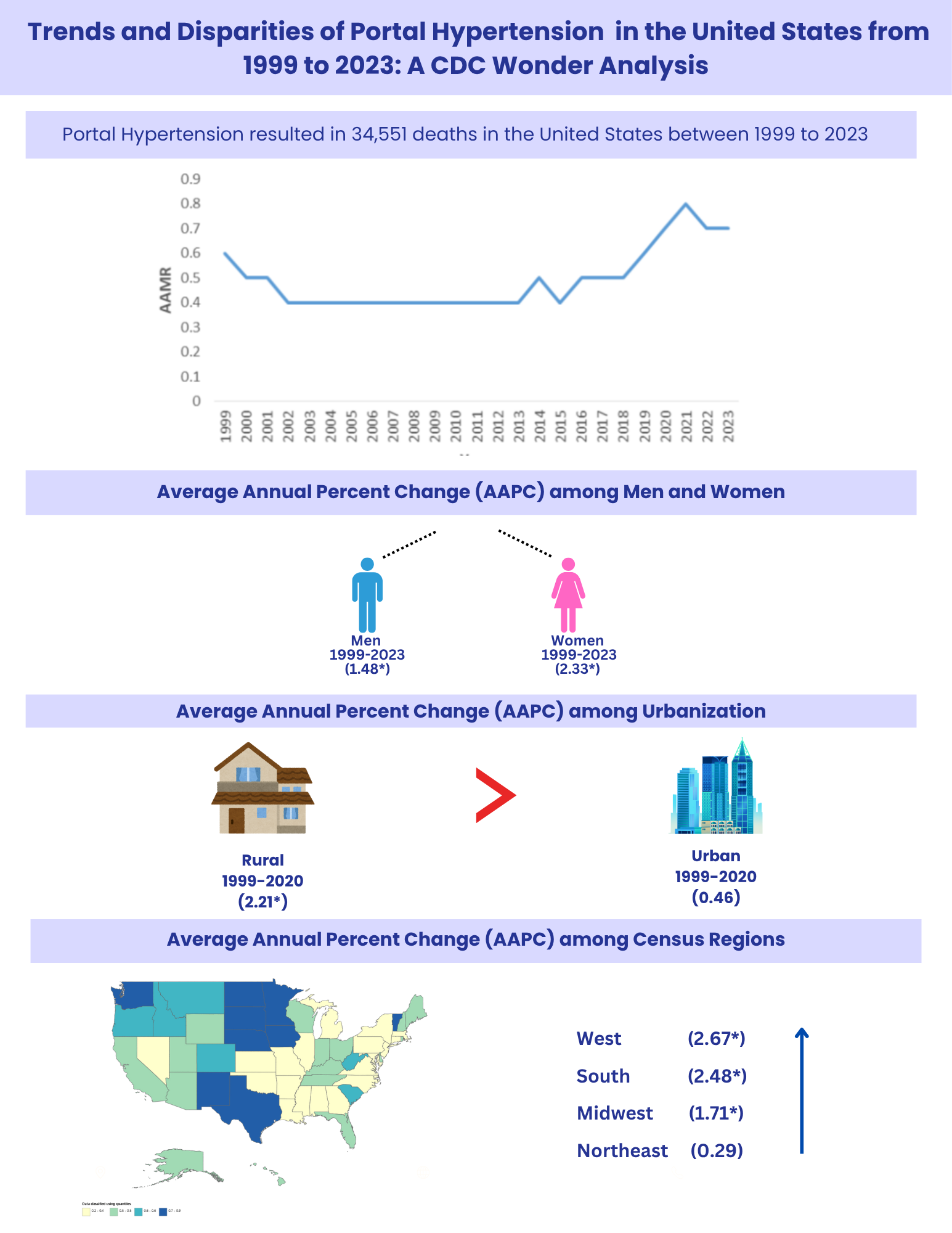
Figure: Graphical Analysis of Overall and Gender-Specific Trends in Portal Hypertension Mortality (1999–2023)
Disclosures:
Raymond Haward indicated no relevant financial relationships.
Nikhil Duseja indicated no relevant financial relationships.
Het Hirpara indicated no relevant financial relationships.
Rachel Haward indicated no relevant financial relationships.
Raymond Haward, MBBS1, Nikhil Duseja, MBBS2, Het Hirpara, MBBS3, Rachel Haward, MBBS4. P3733 - Portal Hypertension Mortality in the United States (1999–2023): Insights from the CDC WONDER Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

