Monday Poster Session
Category: Liver
P3732 - Is BMI an Independent Risk Factor for Post-Liver Transplant Outcomes?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- EE
Ebehiwele Ebhohon, MD, MPH, MS (she/her/hers)
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Ebehiwele Ebhohon, MD, MPH, MS1, David Lee, MD, MS1, Sabtain Saroya, BS2, Michael Chang, MD1, Ashton Harmacinski, MD1, Patrick McCarthy, MD1, Rukaiya Bashir Hamidu, MD1, Nathalie Urrunaga, MD, MS3
1University of Maryland Medical Center, Baltimore, MD; 2College of Medicine, Howard University, Washington, DC; 3University of Maryland, Baltimore, MD
Introduction: Understanding the role of body mass index (BMI) as an independent risk factor for post-liver transplant outcomes is crucial in optimizing patient management. This study examines the association between BMI and key transplant-related outcomes.
Methods: A retrospective cohort analysis was conducted using the UMMC liver transplant database (2016–2018). Patients were stratified into BMI categories: underweight (BMI < 18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25–29.9), and obese (BMI ≥30). Outcomes analyzed were acute cellular rejection, biliary strictures, and all-cause mortality. Adjusted hazard ratios (HRs) were calculated for each outcome, controlling for age, sex, and race
Results: Among 323 patients, BMI was not independently associated with acute rejection, or biliary strictures. Also, mortality rates across BMI categories showed no significant differences, with adjusted HRs of 1.02 (underweight), 0.68 (overweight), and 0.98 (obese) relative to normal weight. Obese patients had longer ICU stays and higher incidence of ERCP utilization but comparable biliary stricture rates. While AST and ALT levels were highest among overweight patients, 1-year graft function outcomes were not significantly different across BMI groups.
Discussion: BMI does not independently predict most common adverse post-transplant outcomes, including mortality, rejection, or biliary strictures, but BMI ≥30 is associated with higher ICU stay and ERCP utilization. These findings suggest BMI alone should not guide transplant eligibility but may impact healthcare.
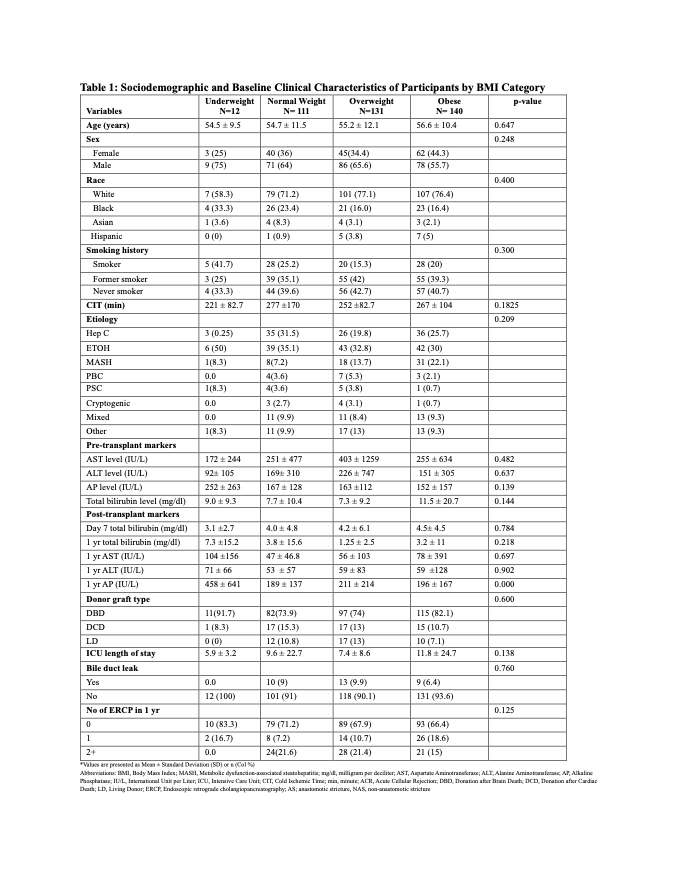
Figure: Table 1: Sociodemographic and Baseline Clinical Characteristics of Participants by BMI Category
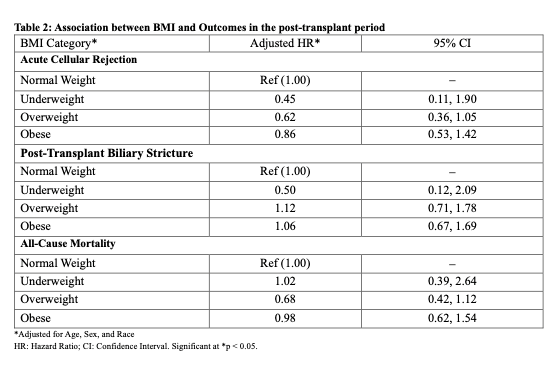
Figure: Table 2: Association between BMI and Outcomes in the post-transplant period
Disclosures:
Ebehiwele Ebhohon indicated no relevant financial relationships.
David Lee indicated no relevant financial relationships.
Sabtain Saroya indicated no relevant financial relationships.
Michael Chang indicated no relevant financial relationships.
Ashton Harmacinski indicated no relevant financial relationships.
Patrick McCarthy indicated no relevant financial relationships.
Rukaiya Bashir Hamidu indicated no relevant financial relationships.
Nathalie Urrunaga indicated no relevant financial relationships.
Ebehiwele Ebhohon, MD, MPH, MS1, David Lee, MD, MS1, Sabtain Saroya, BS2, Michael Chang, MD1, Ashton Harmacinski, MD1, Patrick McCarthy, MD1, Rukaiya Bashir Hamidu, MD1, Nathalie Urrunaga, MD, MS3. P3732 - Is BMI an Independent Risk Factor for Post-Liver Transplant Outcomes?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2College of Medicine, Howard University, Washington, DC; 3University of Maryland, Baltimore, MD
Introduction: Understanding the role of body mass index (BMI) as an independent risk factor for post-liver transplant outcomes is crucial in optimizing patient management. This study examines the association between BMI and key transplant-related outcomes.
Methods: A retrospective cohort analysis was conducted using the UMMC liver transplant database (2016–2018). Patients were stratified into BMI categories: underweight (BMI < 18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25–29.9), and obese (BMI ≥30). Outcomes analyzed were acute cellular rejection, biliary strictures, and all-cause mortality. Adjusted hazard ratios (HRs) were calculated for each outcome, controlling for age, sex, and race
Results: Among 323 patients, BMI was not independently associated with acute rejection, or biliary strictures. Also, mortality rates across BMI categories showed no significant differences, with adjusted HRs of 1.02 (underweight), 0.68 (overweight), and 0.98 (obese) relative to normal weight. Obese patients had longer ICU stays and higher incidence of ERCP utilization but comparable biliary stricture rates. While AST and ALT levels were highest among overweight patients, 1-year graft function outcomes were not significantly different across BMI groups.
Discussion: BMI does not independently predict most common adverse post-transplant outcomes, including mortality, rejection, or biliary strictures, but BMI ≥30 is associated with higher ICU stay and ERCP utilization. These findings suggest BMI alone should not guide transplant eligibility but may impact healthcare.
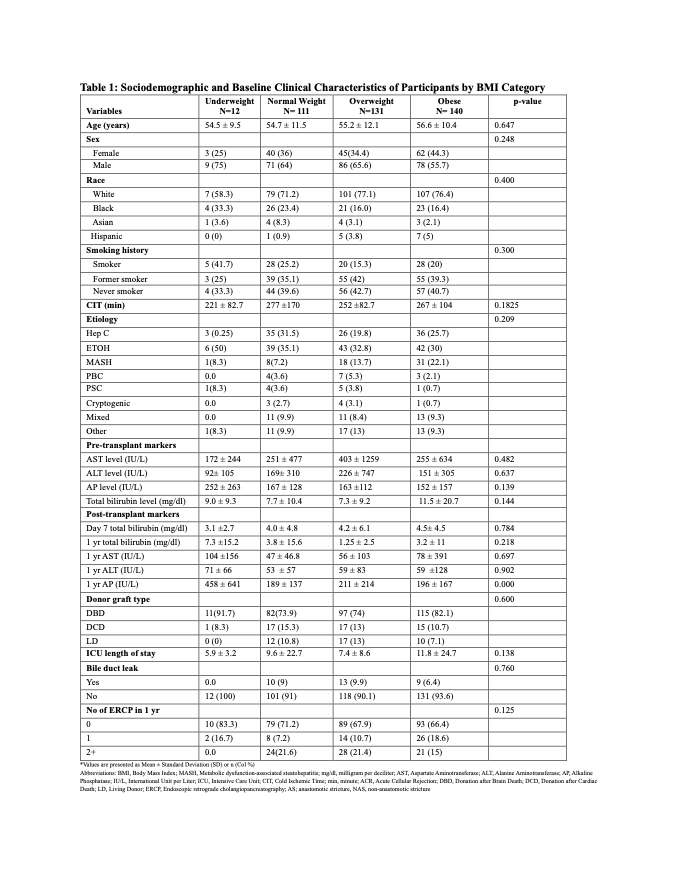
Figure: Table 1: Sociodemographic and Baseline Clinical Characteristics of Participants by BMI Category
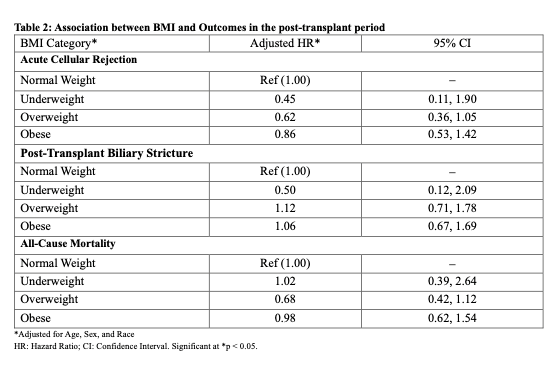
Figure: Table 2: Association between BMI and Outcomes in the post-transplant period
Disclosures:
Ebehiwele Ebhohon indicated no relevant financial relationships.
David Lee indicated no relevant financial relationships.
Sabtain Saroya indicated no relevant financial relationships.
Michael Chang indicated no relevant financial relationships.
Ashton Harmacinski indicated no relevant financial relationships.
Patrick McCarthy indicated no relevant financial relationships.
Rukaiya Bashir Hamidu indicated no relevant financial relationships.
Nathalie Urrunaga indicated no relevant financial relationships.
Ebehiwele Ebhohon, MD, MPH, MS1, David Lee, MD, MS1, Sabtain Saroya, BS2, Michael Chang, MD1, Ashton Harmacinski, MD1, Patrick McCarthy, MD1, Rukaiya Bashir Hamidu, MD1, Nathalie Urrunaga, MD, MS3. P3732 - Is BMI an Independent Risk Factor for Post-Liver Transplant Outcomes?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
