Monday Poster Session
Category: Liver
P3730 - Mortality After Percutaneous Liver Biopsy: Unveiling Risks Across Demographics and Liver Pathologies
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sarah Meribout, MD
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Sarah Meribout, MD1, Ahmed Salem, MD1, Anis Meribout, MD2, Saida Benmostefa, MS3, Ovanes Karslyan, MD1, Fatima Khan, MD1, Nakul Mahajan, MBBS1, Yasutoshi Shiratori, MD1
1Maimonides Medical Center, Brooklyn, NY; 2Icahn School of Medicine at Mount Sinai, Brooklyn, NY; 3Jijel University, Jijel, Constantine, Algeria
Introduction: Liver biopsy is a widely utilized diagnostic tool for assessing liver diseases. However, the risk of mortality associated with this procedure remains poorly understood, especially across different demographic groups. This study aims to identify predictors of mortality in liver biopsy patients and explore disparities based on age, gender, race, socioeconomic status, and comorbid conditions. Understanding these factors is critical to improving patient selection, enhancing procedure safety, and reducing mortality rates.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (NIS) database, analyzing data from 221,925 patients who underwent percutaneous liver biopsy between 2016 and 2019. Of these, 7,530 (3.4%) experienced mortality. Multivariate logistic regression analysis was performed to assess factors associated with mortality. Variables included demographic factors, primary payer type, socioeconomic indicators, comorbid conditions, and procedural details.
Results: Among 221,925 patients undergoing percutaneous liver biopsy, mortality occurred in 3.4% (7,530). Patients with mortality were older (mean age 66.8 vs. 59.2, p< 0.001) and more likely to be male (p< 0.001). Mortality was higher in patients with Medicare coverage (60.2%) and those with ≥3 comorbidities (78.8%, p< 0.001). Factors independently associated with increased mortality included age ≥70 (OR 2.05, 95% CI 1.84–2.30), liver malignancy (OR 1.20, 95% CI 1.10–1.32), alcoholic liver disease (OR 1.66, 95% CI 1.42–1.93), post-procedural bleeding (OR 3.46, 95% CI 2.97–4.02), and infection (OR 1.77, 95% CI 1.55–2.03). Elective admission (OR 0.40, 95% CI 0.36–0.44) and NAFLD (OR 0.60, 95% CI 0.48–0.74) were protective. Identifying these predictors can guide pre-procedure risk stratification and optimize outcomes.
Discussion: This large retrospective cohort study highlights that mortality following percutaneous liver biopsy is significantly associated with advanced age, male sex, liver malignancy, alcoholic liver disease, post-procedural complications, and high comorbidity burden. Protective factors include elective admission and NAFLD. These findings underscore the need for thorough pre-procedure risk stratification, especially in vulnerable populations, to enhance patient safety and optimize outcomes. Addressing disparities across demographics can further mitigate mortality risks associated with this widely utilized diagnostic procedure.
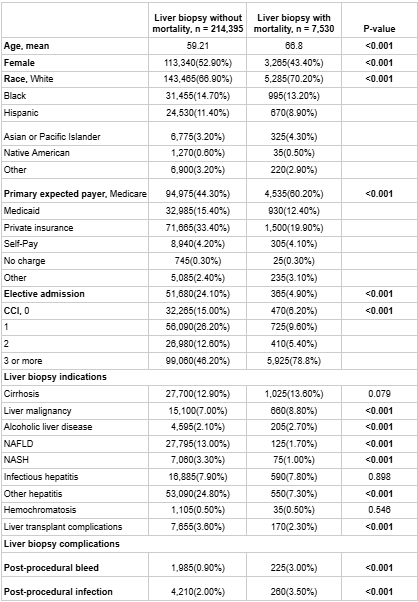
Figure: Table 1. Baseline Characteristics and Outcomes of Liver Biopsy Patients With and Without Mortality
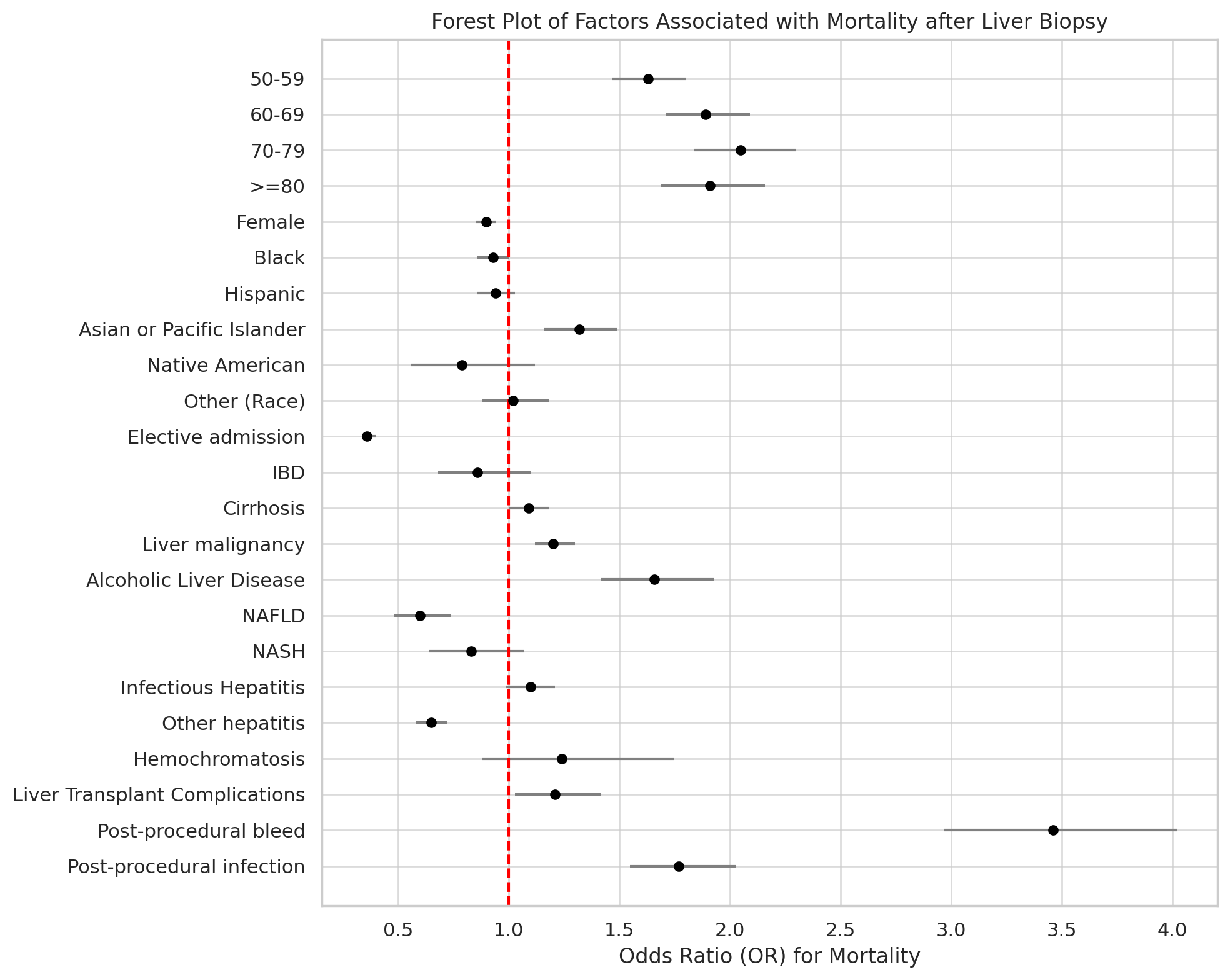
Figure: Figure 1. Forest plot of the odds ratios (ORs) and 95% confidence intervals for mortality after liver biopsy, based on multivariate logistic regression analysis.
Disclosures:
Sarah Meribout indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Anis Meribout indicated no relevant financial relationships.
Saida Benmostefa indicated no relevant financial relationships.
Ovanes Karslyan indicated no relevant financial relationships.
Fatima Khan indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Yasutoshi Shiratori indicated no relevant financial relationships.
Sarah Meribout, MD1, Ahmed Salem, MD1, Anis Meribout, MD2, Saida Benmostefa, MS3, Ovanes Karslyan, MD1, Fatima Khan, MD1, Nakul Mahajan, MBBS1, Yasutoshi Shiratori, MD1. P3730 - Mortality After Percutaneous Liver Biopsy: Unveiling Risks Across Demographics and Liver Pathologies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Icahn School of Medicine at Mount Sinai, Brooklyn, NY; 3Jijel University, Jijel, Constantine, Algeria
Introduction: Liver biopsy is a widely utilized diagnostic tool for assessing liver diseases. However, the risk of mortality associated with this procedure remains poorly understood, especially across different demographic groups. This study aims to identify predictors of mortality in liver biopsy patients and explore disparities based on age, gender, race, socioeconomic status, and comorbid conditions. Understanding these factors is critical to improving patient selection, enhancing procedure safety, and reducing mortality rates.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (NIS) database, analyzing data from 221,925 patients who underwent percutaneous liver biopsy between 2016 and 2019. Of these, 7,530 (3.4%) experienced mortality. Multivariate logistic regression analysis was performed to assess factors associated with mortality. Variables included demographic factors, primary payer type, socioeconomic indicators, comorbid conditions, and procedural details.
Results: Among 221,925 patients undergoing percutaneous liver biopsy, mortality occurred in 3.4% (7,530). Patients with mortality were older (mean age 66.8 vs. 59.2, p< 0.001) and more likely to be male (p< 0.001). Mortality was higher in patients with Medicare coverage (60.2%) and those with ≥3 comorbidities (78.8%, p< 0.001). Factors independently associated with increased mortality included age ≥70 (OR 2.05, 95% CI 1.84–2.30), liver malignancy (OR 1.20, 95% CI 1.10–1.32), alcoholic liver disease (OR 1.66, 95% CI 1.42–1.93), post-procedural bleeding (OR 3.46, 95% CI 2.97–4.02), and infection (OR 1.77, 95% CI 1.55–2.03). Elective admission (OR 0.40, 95% CI 0.36–0.44) and NAFLD (OR 0.60, 95% CI 0.48–0.74) were protective. Identifying these predictors can guide pre-procedure risk stratification and optimize outcomes.
Discussion: This large retrospective cohort study highlights that mortality following percutaneous liver biopsy is significantly associated with advanced age, male sex, liver malignancy, alcoholic liver disease, post-procedural complications, and high comorbidity burden. Protective factors include elective admission and NAFLD. These findings underscore the need for thorough pre-procedure risk stratification, especially in vulnerable populations, to enhance patient safety and optimize outcomes. Addressing disparities across demographics can further mitigate mortality risks associated with this widely utilized diagnostic procedure.
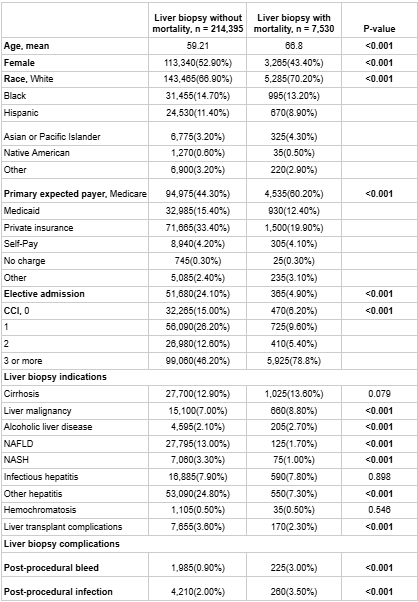
Figure: Table 1. Baseline Characteristics and Outcomes of Liver Biopsy Patients With and Without Mortality
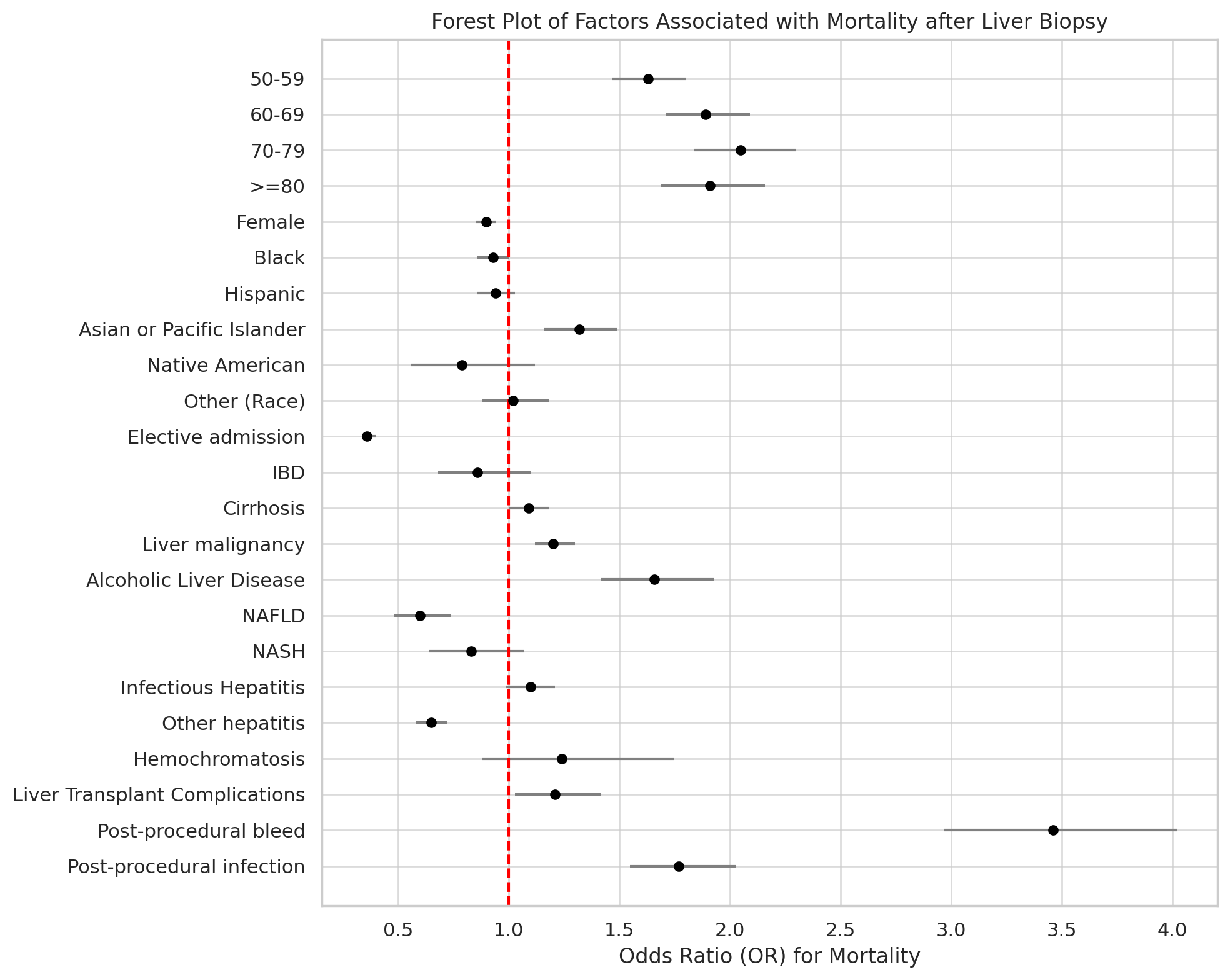
Figure: Figure 1. Forest plot of the odds ratios (ORs) and 95% confidence intervals for mortality after liver biopsy, based on multivariate logistic regression analysis.
Disclosures:
Sarah Meribout indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Anis Meribout indicated no relevant financial relationships.
Saida Benmostefa indicated no relevant financial relationships.
Ovanes Karslyan indicated no relevant financial relationships.
Fatima Khan indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Yasutoshi Shiratori indicated no relevant financial relationships.
Sarah Meribout, MD1, Ahmed Salem, MD1, Anis Meribout, MD2, Saida Benmostefa, MS3, Ovanes Karslyan, MD1, Fatima Khan, MD1, Nakul Mahajan, MBBS1, Yasutoshi Shiratori, MD1. P3730 - Mortality After Percutaneous Liver Biopsy: Unveiling Risks Across Demographics and Liver Pathologies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
