Monday Poster Session
Category: Liver
P3729 - Racial Disparities in Prevalence of Cirrhosis and Extrahepatic Manifestations in Alcohol-Associated Liver Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pradhan Hariharan, BS (he/him/his)
University of Arizona College of Medicine - Phoenix
Phoenix, AZ
Presenting Author(s)
Pradhan Hariharan, BS1, Majd Aboona, MD1, Janet A. Foote, PhD1, Leith Ghani, DO2, Vanessa Eller, MD3, Ryan Toledo, MD1, Pooja Rangan, MBBS, MPH4, David Garcia, PhD5, Vincent L. Chen, MD, MS6, Donghee Kim, MD, PhD7, Juan Pablo Arab, MD8, Mazen Noureddin, MD9, Luis Antonio Diaz, MD10, Michael Fallon, MD1, Karn Wijarnpreecha, MD, MPH2
1University of Arizona College of Medicine - Phoenix, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, Phoenix, AZ; 4University of Arizona College of Medicine – Phoenix, Phoenix, AZ; 5University of Arizona Mel and Enid Zuckerman College of Public Health - Tucson, Tucson, AZ; 6University of Michigan, Ann Arbor, MI; 7Stanford University School of Medicine, Stanford, CA; 8Virginia Commonwealth University School of Medicine, Richmond, VA; 9Houston Research Institute and Houston Methodist Hospital, Houston, TX; 10University of California San Diego, San Diego, CA
Introduction: Alcohol-associated liver disease (ALD) is the leading cause of cirrhosis in Western countries and is responsible for 25% of cirrhosis-related deaths. Alcohol can contribute to the development of extrahepatic manifestations. However, limited literature exists regarding extrahepatic outcomes of ALD in diverse patient populations. This study assesses racial disparities in the prevalence of cirrhosis and extrahepatic manifestations in ALD from a diverse cohort.
Methods: We included patients with ALD in the Banner Health System, representing hospitals across Arizona, California, Nevada, Wyoming, and Colorado, from 2012 to 2024 using ICD codes with randomly selected chart review of over 250 cases to validate ICD codes for ALD and extrahepatic outcomes. We excluded patients with other causes of liver disease and baseline decompensated cirrhosis. The primary outcomes are the prevalence of any cardiovascular disease (CVD), coronary artery disease (CAD), peripheral artery disease (PAD), cerebrovascular accident (CVA), congestive heart failure (CHF), cirrhosis, and type 2 diabetes mellitus (T2DM) among racial groups. A multivariate logistic regression analysis was performed and adjusted for age, sex, hypertension, T2DM, use of aspirin, statin, glucagon-like peptide-1 receptor agonist, alcohol use treatment, and smoking.
Results: The cohort included 16,693 patients with ALD. 66.7% were Non-Hispanic White, 17.9% Hispanic, 11.8% Native American/Alaskan Native (NA), 3.2% Black, and 0.4% Asian/Pacific Islanders. Compared to Non-Hispanic White patients, Hispanic patients had a higher prevalence of cirrhosis (adjusted odds ratio (aOR) 1.38; 95% confidence interval (CI): 1.26–1.51) and T2DM (aOR 2.17; 95%CI: 1.96–2.39). Black patients had a higher prevalence of any CVD (aOR 1.41; 95%CI: 1.13–1.76), CVA (aOR 1.56; 95%CI: 1.11–2.19), CHF (aOR 1.72; 95%CI: 1.31–2.26), and T2DM (aOR 1.58; 95%CI: 1.29–1.94). NA individuals had a higher prevalence of cirrhosis (aOR 2.22; 95%CI: 1.99-2.47) and T2DM (aOR 3.64; 95%CI: 3.23-4.09).
Discussion: In this cohort of patients with ALD, Hispanic and NA patients had a higher prevalence of cirrhosis and DM than Non-Hispanic White patients. Additionally, Black patients had a higher prevalence of CVD. These findings suggest these racial groups may have worse metabolic profiles and cirrhosis, leading to poorer clinical outcomes. Further attention to racial disparities and liver and cardiometabolic risk stratification in patients with ALD is warranted to address these inequities.
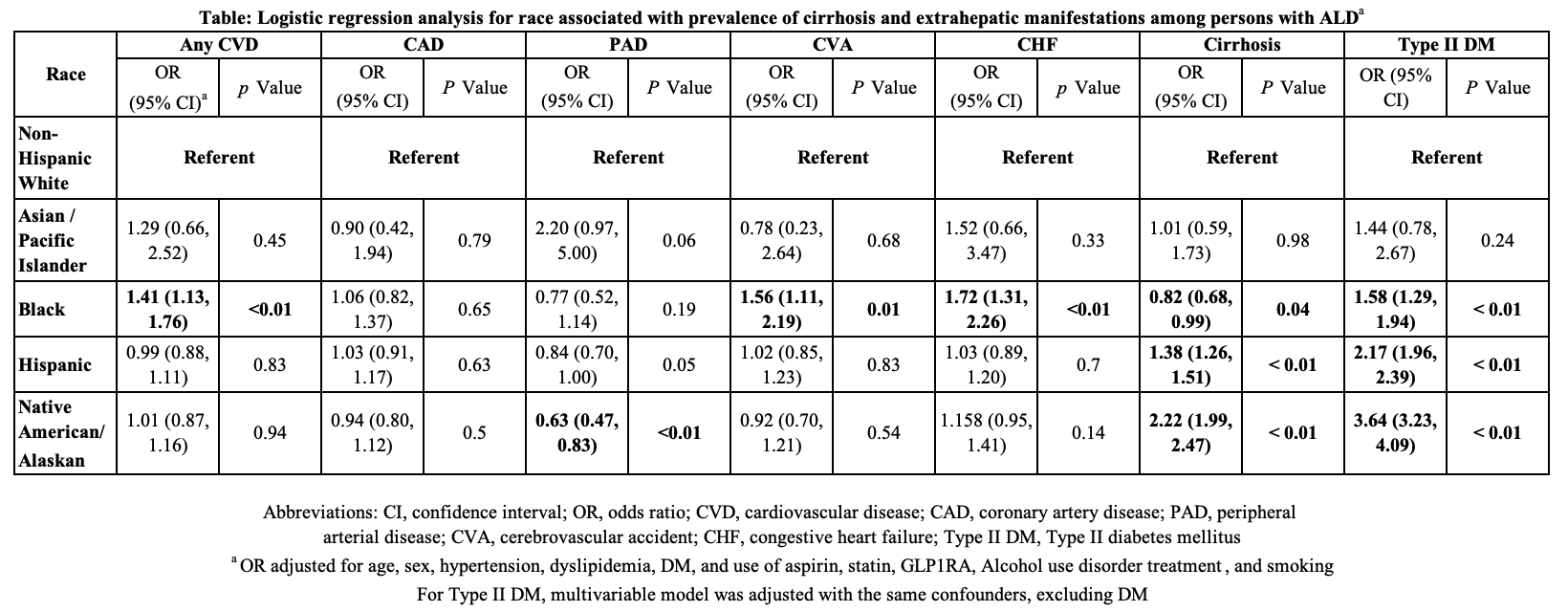
Figure: Table: Logistic regression analysis for race associated with prevalence of cirrhosis and extrahepatic manifestations among persons with ALD
Disclosures:
Pradhan Hariharan indicated no relevant financial relationships.
Majd Aboona indicated no relevant financial relationships.
Janet Foote indicated no relevant financial relationships.
Leith Ghani indicated no relevant financial relationships.
Vanessa Eller indicated no relevant financial relationships.
Ryan Toledo indicated no relevant financial relationships.
Pooja Rangan indicated no relevant financial relationships.
David Garcia indicated no relevant financial relationships.
Vincent Chen: AstraZeneca – Grant/Research Support. Ipsen – Grant/Research Support. KOWA – Grant/Research Support.
Donghee Kim indicated no relevant financial relationships.
Juan Pablo Arab indicated no relevant financial relationships.
Mazen Noureddin: Madrigal Pharmaceuticals – Advisor or Review Panel Member, Consultant, Royalties, Speakers Bureau.
Luis Antonio Diaz indicated no relevant financial relationships.
Michael Fallon indicated no relevant financial relationships.
Karn Wijarnpreecha indicated no relevant financial relationships.
Pradhan Hariharan, BS1, Majd Aboona, MD1, Janet A. Foote, PhD1, Leith Ghani, DO2, Vanessa Eller, MD3, Ryan Toledo, MD1, Pooja Rangan, MBBS, MPH4, David Garcia, PhD5, Vincent L. Chen, MD, MS6, Donghee Kim, MD, PhD7, Juan Pablo Arab, MD8, Mazen Noureddin, MD9, Luis Antonio Diaz, MD10, Michael Fallon, MD1, Karn Wijarnpreecha, MD, MPH2. P3729 - Racial Disparities in Prevalence of Cirrhosis and Extrahepatic Manifestations in Alcohol-Associated Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine - Phoenix, Phoenix, AZ; 2University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix, Phoenix, AZ; 4University of Arizona College of Medicine – Phoenix, Phoenix, AZ; 5University of Arizona Mel and Enid Zuckerman College of Public Health - Tucson, Tucson, AZ; 6University of Michigan, Ann Arbor, MI; 7Stanford University School of Medicine, Stanford, CA; 8Virginia Commonwealth University School of Medicine, Richmond, VA; 9Houston Research Institute and Houston Methodist Hospital, Houston, TX; 10University of California San Diego, San Diego, CA
Introduction: Alcohol-associated liver disease (ALD) is the leading cause of cirrhosis in Western countries and is responsible for 25% of cirrhosis-related deaths. Alcohol can contribute to the development of extrahepatic manifestations. However, limited literature exists regarding extrahepatic outcomes of ALD in diverse patient populations. This study assesses racial disparities in the prevalence of cirrhosis and extrahepatic manifestations in ALD from a diverse cohort.
Methods: We included patients with ALD in the Banner Health System, representing hospitals across Arizona, California, Nevada, Wyoming, and Colorado, from 2012 to 2024 using ICD codes with randomly selected chart review of over 250 cases to validate ICD codes for ALD and extrahepatic outcomes. We excluded patients with other causes of liver disease and baseline decompensated cirrhosis. The primary outcomes are the prevalence of any cardiovascular disease (CVD), coronary artery disease (CAD), peripheral artery disease (PAD), cerebrovascular accident (CVA), congestive heart failure (CHF), cirrhosis, and type 2 diabetes mellitus (T2DM) among racial groups. A multivariate logistic regression analysis was performed and adjusted for age, sex, hypertension, T2DM, use of aspirin, statin, glucagon-like peptide-1 receptor agonist, alcohol use treatment, and smoking.
Results: The cohort included 16,693 patients with ALD. 66.7% were Non-Hispanic White, 17.9% Hispanic, 11.8% Native American/Alaskan Native (NA), 3.2% Black, and 0.4% Asian/Pacific Islanders. Compared to Non-Hispanic White patients, Hispanic patients had a higher prevalence of cirrhosis (adjusted odds ratio (aOR) 1.38; 95% confidence interval (CI): 1.26–1.51) and T2DM (aOR 2.17; 95%CI: 1.96–2.39). Black patients had a higher prevalence of any CVD (aOR 1.41; 95%CI: 1.13–1.76), CVA (aOR 1.56; 95%CI: 1.11–2.19), CHF (aOR 1.72; 95%CI: 1.31–2.26), and T2DM (aOR 1.58; 95%CI: 1.29–1.94). NA individuals had a higher prevalence of cirrhosis (aOR 2.22; 95%CI: 1.99-2.47) and T2DM (aOR 3.64; 95%CI: 3.23-4.09).
Discussion: In this cohort of patients with ALD, Hispanic and NA patients had a higher prevalence of cirrhosis and DM than Non-Hispanic White patients. Additionally, Black patients had a higher prevalence of CVD. These findings suggest these racial groups may have worse metabolic profiles and cirrhosis, leading to poorer clinical outcomes. Further attention to racial disparities and liver and cardiometabolic risk stratification in patients with ALD is warranted to address these inequities.
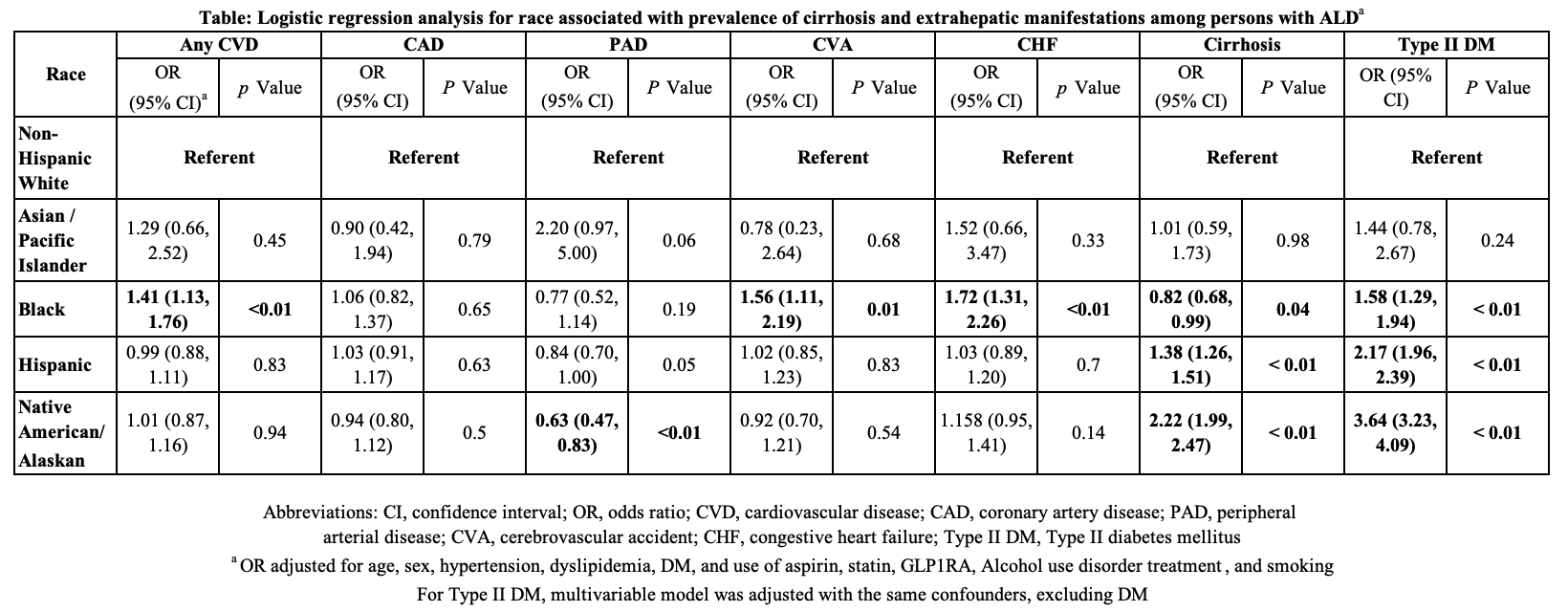
Figure: Table: Logistic regression analysis for race associated with prevalence of cirrhosis and extrahepatic manifestations among persons with ALD
Disclosures:
Pradhan Hariharan indicated no relevant financial relationships.
Majd Aboona indicated no relevant financial relationships.
Janet Foote indicated no relevant financial relationships.
Leith Ghani indicated no relevant financial relationships.
Vanessa Eller indicated no relevant financial relationships.
Ryan Toledo indicated no relevant financial relationships.
Pooja Rangan indicated no relevant financial relationships.
David Garcia indicated no relevant financial relationships.
Vincent Chen: AstraZeneca – Grant/Research Support. Ipsen – Grant/Research Support. KOWA – Grant/Research Support.
Donghee Kim indicated no relevant financial relationships.
Juan Pablo Arab indicated no relevant financial relationships.
Mazen Noureddin: Madrigal Pharmaceuticals – Advisor or Review Panel Member, Consultant, Royalties, Speakers Bureau.
Luis Antonio Diaz indicated no relevant financial relationships.
Michael Fallon indicated no relevant financial relationships.
Karn Wijarnpreecha indicated no relevant financial relationships.
Pradhan Hariharan, BS1, Majd Aboona, MD1, Janet A. Foote, PhD1, Leith Ghani, DO2, Vanessa Eller, MD3, Ryan Toledo, MD1, Pooja Rangan, MBBS, MPH4, David Garcia, PhD5, Vincent L. Chen, MD, MS6, Donghee Kim, MD, PhD7, Juan Pablo Arab, MD8, Mazen Noureddin, MD9, Luis Antonio Diaz, MD10, Michael Fallon, MD1, Karn Wijarnpreecha, MD, MPH2. P3729 - Racial Disparities in Prevalence of Cirrhosis and Extrahepatic Manifestations in Alcohol-Associated Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

