Tuesday Poster Session
Category: Biliary/Pancreas
P4286 - Is Your Intragastric Balloon Squeezing Your Pancreas? An Evidence-Based Management Approach
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jeril Lasington, MD
St. Mary's General Hospital, New York Medical College
Pine Brook, NJ
Presenting Author(s)
Jeril Lasington, MD1, Preeti Yendapalli, 2, Arshiya Shabnam, MBBS, MD3
1St. Mary's General Hospital, New York Medical College, Pine Brook, NJ; 2Saint Clare's Health, New York Medical College, Rockaway, NJ; 3New York Medical College, Denville, NJ
Introduction: Intragastric balloons are endoscopic or swallowable bariatric devices, although safe, may carry a serious risk of acute pancreatitis (AP), first highlighted by the FDA in 2016.
Methods: Targeted searches in PubMed/Scopus, Cochrane and Embase (2015–2025) were done and 17 studies were reviewed and analyzed thematically.
Results: IGB-associated pancreatitis ranged from 0.06% in procedureless balloons (e.g., Elipse®) to 5.56% in high-volume devices ( >600 mL, such as Orbera®/BIB®) among the 90 cases reported worldwide.
IGB-induced pancreatitis may be due to:
Direct Compression from overfilled balloons ( >600 mL) deforming the pancreatic body or tail, causing duct obstruction and inflammation (around 70% of cases).
Duodenal Migration in adjustable balloons can obstruct the ampulla, causing biliary reflux and lipase >30,000 U/L.
Chronic Ductal Obstruction, usually subclinical ductal compression, may present with asymptomatic lipase elevations ( >3× ULN).
Ischemic injury from gastric mucosal pressure may further exacerbate pancreatic damage, especially with adjustable devices.
Presenting symptoms include epigastric pain radiating to back (92%), intractable vomiting (100%) with elevated lipase > 3× ULN. Imaging findings include pancreatic compression, duct dilation, or device migration on CT scans.
Early onset (< 72 hours) suggests acute compression, while subacute presentations (1–4 weeks) are likely due to device migration or chronic ductal obstruction.
In Mild AP with lipase < 1,000 U/L without necrosis, a 48-hour conservative approach (NPO, IV fluids) resolves about 50% of cases without device removal.
Moderate to Severe AP may have organ failure or necrosis requiring immediate endoscopic removal, with inspection for ischemia.
In Migration Complications endoscopic retrieval is first-line, if unsuccessful, surgical intervention (laparotomy) is indicated.
Discussion: We believe that pancreatitis risk may be decreased by volume restriction to limit balloon filling to ≤600 mL (≤550 mL for Elipse®); endoscopic confirmation of position in the fundus ; baseline and 24-hour post-insertion lipase monitoring for risk identification; and avoid rigid catheters in those with duodenal anomalies.
Future developments focused on device design improvements with respect to volume limitation, shape adaptive balloons, position sensors and migration prevention features, and protocols for prevention and management of instrument induced pancreatitis may help mitigate this serious complication.
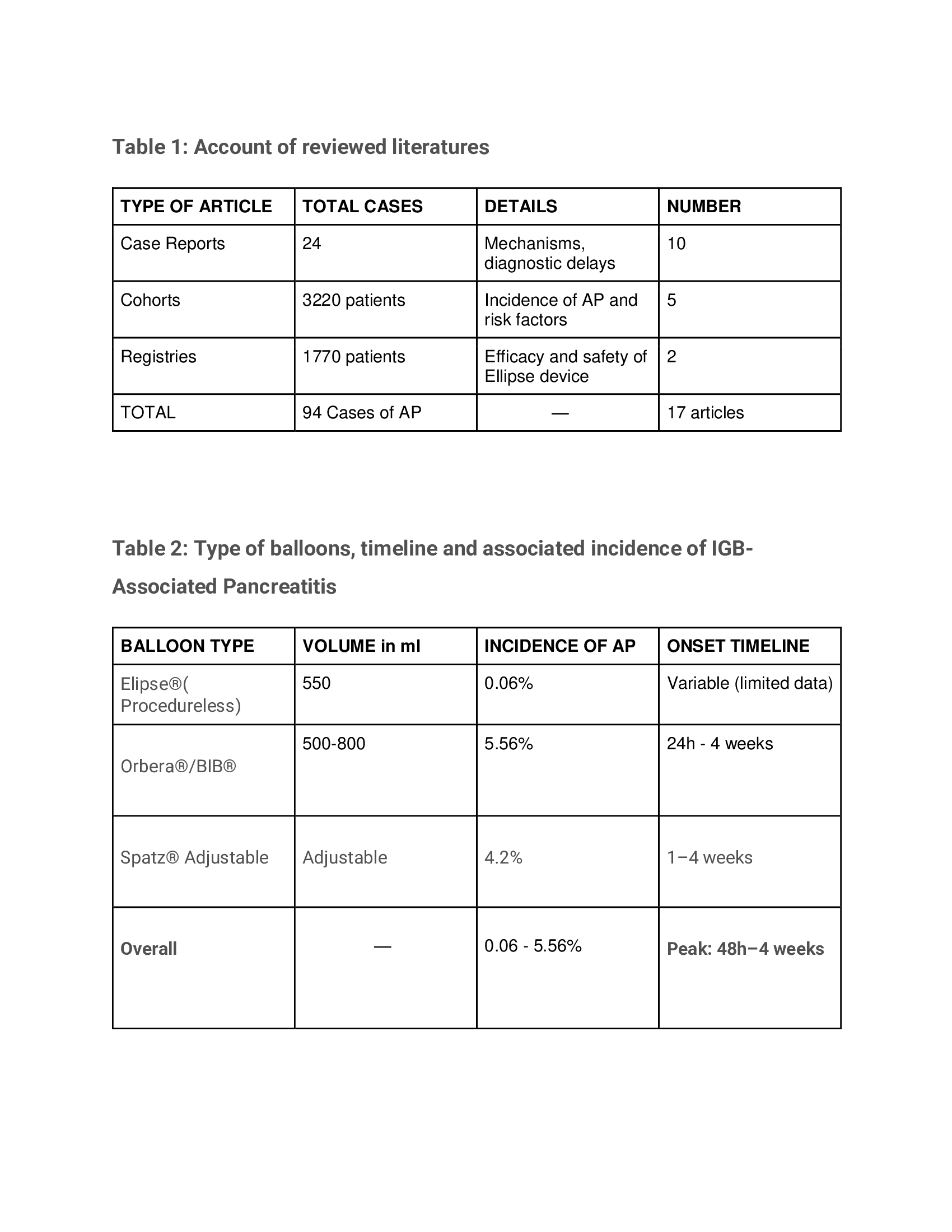
Figure: Tables 1 and 2
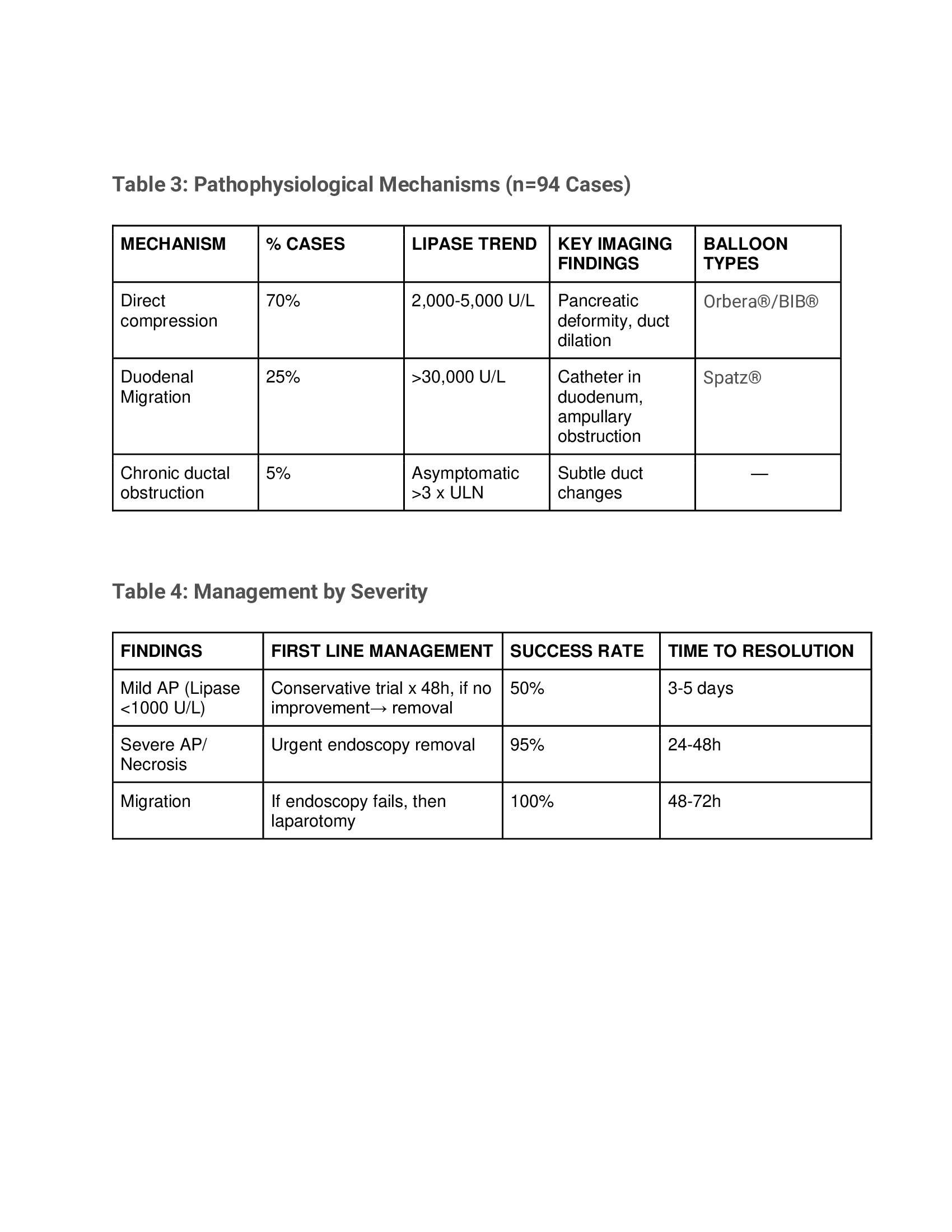
Figure: Table 3 and 4
Disclosures:
Jeril Lasington indicated no relevant financial relationships.
Preeti Yendapalli indicated no relevant financial relationships.
Arshiya Shabnam indicated no relevant financial relationships.
Jeril Lasington, MD1, Preeti Yendapalli, 2, Arshiya Shabnam, MBBS, MD3. P4286 - Is Your Intragastric Balloon Squeezing Your Pancreas? An Evidence-Based Management Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Mary's General Hospital, New York Medical College, Pine Brook, NJ; 2Saint Clare's Health, New York Medical College, Rockaway, NJ; 3New York Medical College, Denville, NJ
Introduction: Intragastric balloons are endoscopic or swallowable bariatric devices, although safe, may carry a serious risk of acute pancreatitis (AP), first highlighted by the FDA in 2016.
Methods: Targeted searches in PubMed/Scopus, Cochrane and Embase (2015–2025) were done and 17 studies were reviewed and analyzed thematically.
Results: IGB-associated pancreatitis ranged from 0.06% in procedureless balloons (e.g., Elipse®) to 5.56% in high-volume devices ( >600 mL, such as Orbera®/BIB®) among the 90 cases reported worldwide.
IGB-induced pancreatitis may be due to:
Direct Compression from overfilled balloons ( >600 mL) deforming the pancreatic body or tail, causing duct obstruction and inflammation (around 70% of cases).
Duodenal Migration in adjustable balloons can obstruct the ampulla, causing biliary reflux and lipase >30,000 U/L.
Chronic Ductal Obstruction, usually subclinical ductal compression, may present with asymptomatic lipase elevations ( >3× ULN).
Ischemic injury from gastric mucosal pressure may further exacerbate pancreatic damage, especially with adjustable devices.
Presenting symptoms include epigastric pain radiating to back (92%), intractable vomiting (100%) with elevated lipase > 3× ULN. Imaging findings include pancreatic compression, duct dilation, or device migration on CT scans.
Early onset (< 72 hours) suggests acute compression, while subacute presentations (1–4 weeks) are likely due to device migration or chronic ductal obstruction.
In Mild AP with lipase < 1,000 U/L without necrosis, a 48-hour conservative approach (NPO, IV fluids) resolves about 50% of cases without device removal.
Moderate to Severe AP may have organ failure or necrosis requiring immediate endoscopic removal, with inspection for ischemia.
In Migration Complications endoscopic retrieval is first-line, if unsuccessful, surgical intervention (laparotomy) is indicated.
Discussion: We believe that pancreatitis risk may be decreased by volume restriction to limit balloon filling to ≤600 mL (≤550 mL for Elipse®); endoscopic confirmation of position in the fundus ; baseline and 24-hour post-insertion lipase monitoring for risk identification; and avoid rigid catheters in those with duodenal anomalies.
Future developments focused on device design improvements with respect to volume limitation, shape adaptive balloons, position sensors and migration prevention features, and protocols for prevention and management of instrument induced pancreatitis may help mitigate this serious complication.
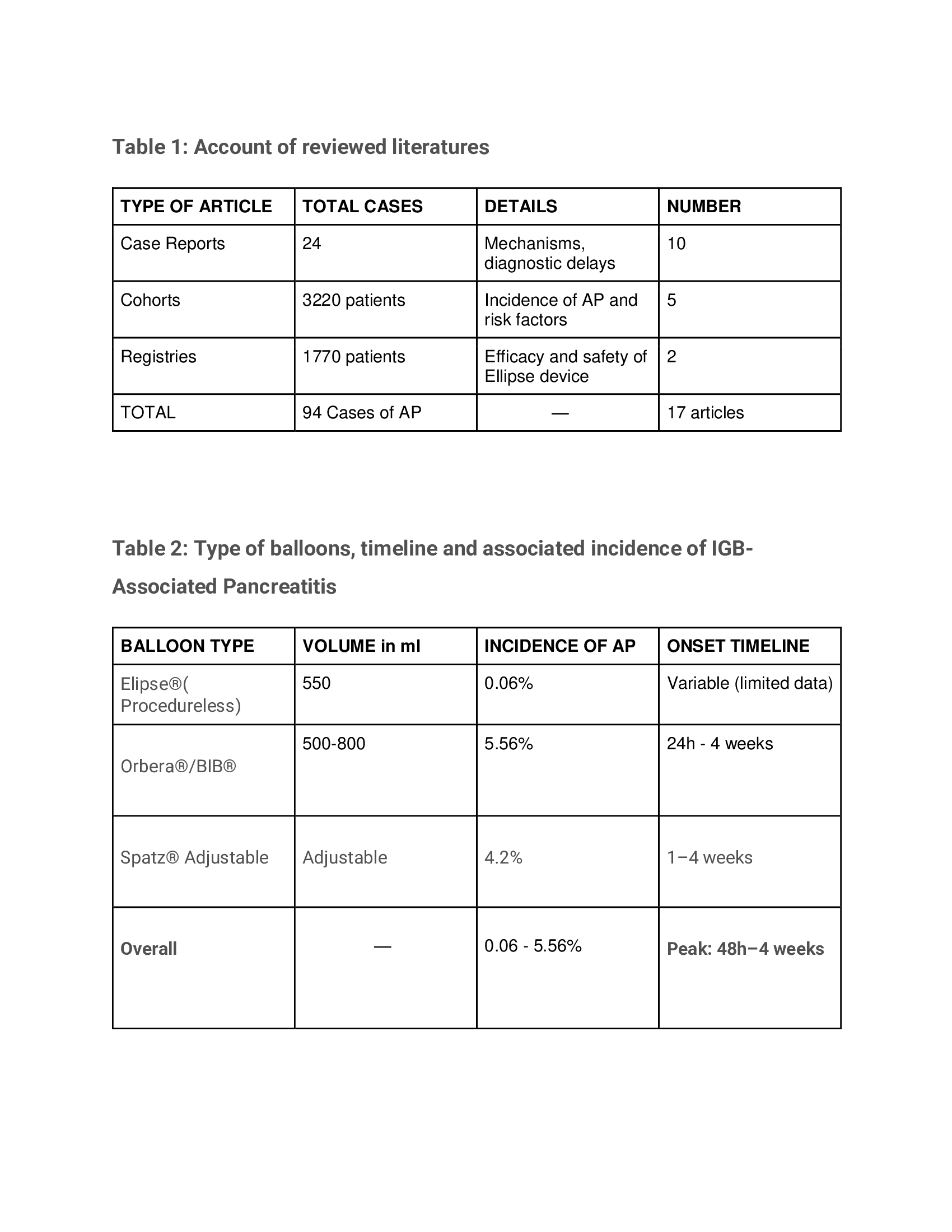
Figure: Tables 1 and 2
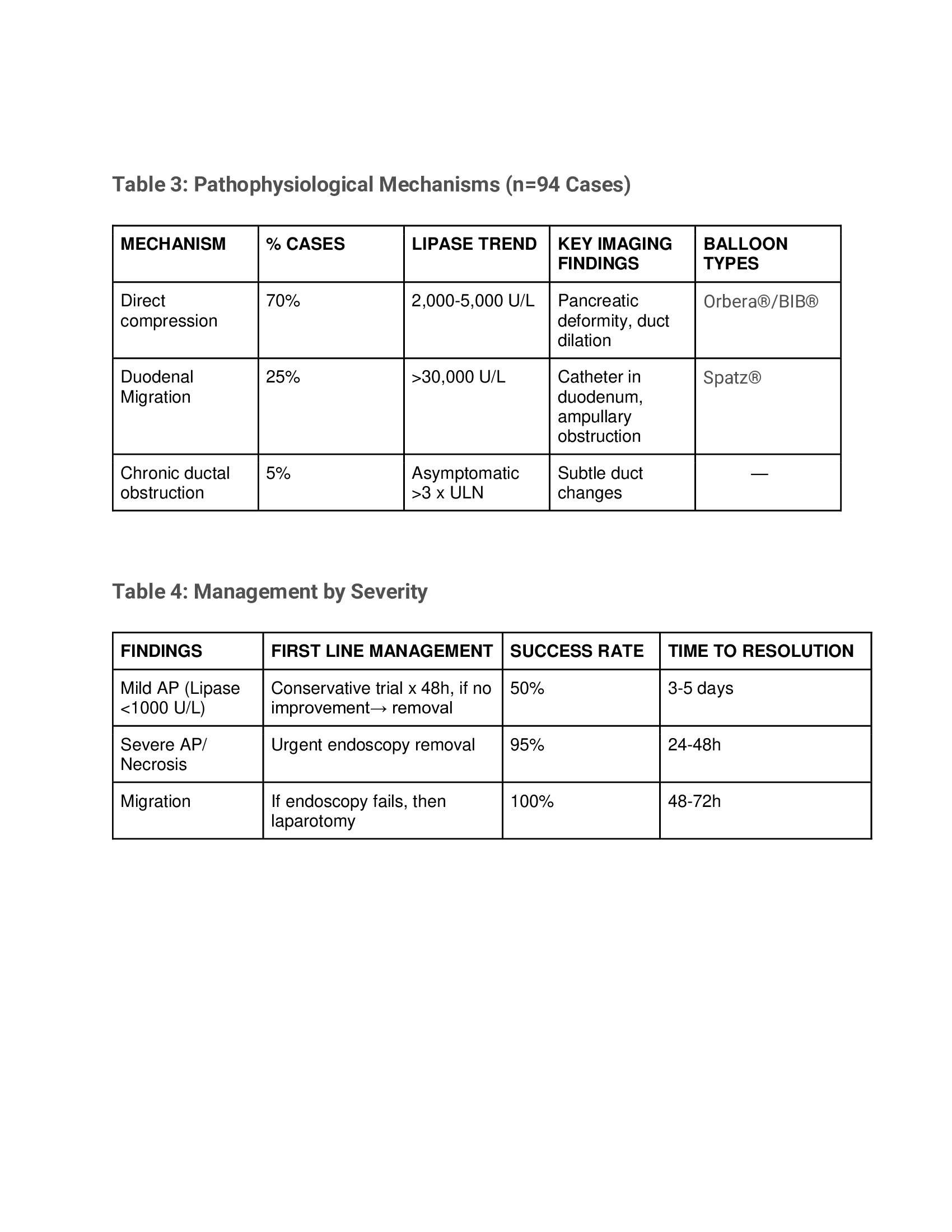
Figure: Table 3 and 4
Disclosures:
Jeril Lasington indicated no relevant financial relationships.
Preeti Yendapalli indicated no relevant financial relationships.
Arshiya Shabnam indicated no relevant financial relationships.
Jeril Lasington, MD1, Preeti Yendapalli, 2, Arshiya Shabnam, MBBS, MD3. P4286 - Is Your Intragastric Balloon Squeezing Your Pancreas? An Evidence-Based Management Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
