Tuesday Poster Session
Category: Biliary/Pancreas
P4284 - Infectious Complications and Safety Outcomes in Cholangioscopy: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shivangini Duggal, MD
Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Akshay Sharma, MBBS2, Vishali Moond, MD3, Simran Joshi, MD4, Mehak Sachdeva, MBBS5, Nirav Thosani, MD6, Prateek Harne, MD7
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Luminis Health Anne Arundel Medical Center, Annapolis, MD; 3Saint Peter's University Hospital/Robert Wood Johnson Medical School loc, New Brunswick, NJ; 4Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 5University of Central Florida, HCA Healthcare GME, Ocala, FL; 6University of Texas Health, McGovern Medical School, Houston, TX; 7Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Peroral cholangioscopy enables direct visualization of the biliary tree and has become increasingly utilized for the management of choledocholithiasis and indeterminate biliary strictures. However, concerns remain regarding post-procedural infectious complications, including bacteremia and cholangitis. Current guidelines offer limited guidance on prophylactic antibiotic use during cholangioscopy. We aimed to evaluate the pooled rates of bacteremia and other adverse events associated with cholangioscopy, assess procedural success, and examine the impact of antibiotic prophylaxis.
Methods: A systematic review and meta-analysis was conducted according to PRISMA guidelines. Literature searches were performed across PubMed, Embase, Scopus, Cochrane Library, and Google Scholar through March 2025. Thirteen studies encompassing 4,413 cholangioscopy-guided procedures were included. Pooled proportions for technical/clinical success and adverse events were calculated using random-effects models. Subgroup analyses evaluated the role of pre-procedural antibiotic use and biopsy.
Results: Pooled technical and clinical success rates were 97.3% (95% CI: 94.8%–98.6%) and 88.4% (95% CI: 80.5%–93.3%), respectively. Bacteremia was the most frequent infectious complication (6.8%; 95% CI: 3.1%–14.3%), followed by cholangitis (4.1%) and pancreatitis (3.6%). When adverse events were categorized using the ASGE lexicon, mild events were most common (7.5%; 95% CI: 4.1%–13.2%; I² = 93%), with rare severe (0.7%) or fatal (0.4%) complications. Studies without pre-procedural antibiotics or those involving biopsy showed higher bacteremia rates. Despite widespread use of prophylactic antibiotics, no consistent reduction in infectious complications was observed. Evidence of publication bias was detected (p < 0.01).
Discussion: Cholangioscopy is highly effective and generally safe; however, bacteremia remains a notable complication, particularly in high-risk patients and with biopsy use. The role of antibiotic prophylaxis remains unclear. Future studies should aim to standardize infection prevention protocols and define high-risk subgroups to optimize prophylactic strategies.
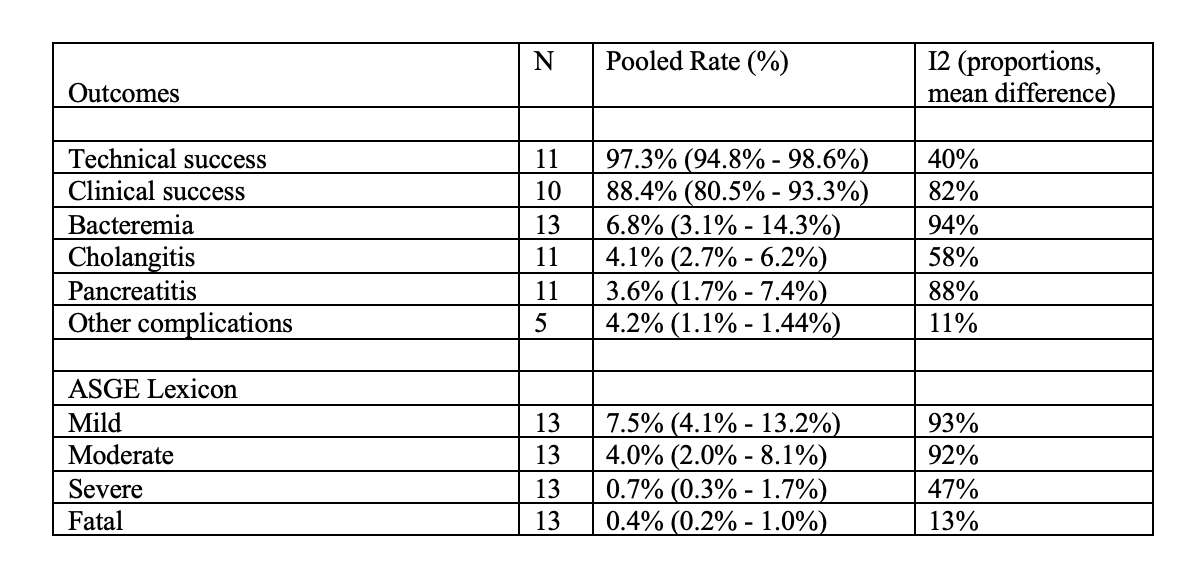
Figure: Table 1. Displays the results across each outcome for this meta-analysis.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Akshay Sharma indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Simran Joshi indicated no relevant financial relationships.
Mehak Sachdeva indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Prateek Harne indicated no relevant financial relationships.
Shivangini Duggal, MD1, Akshay Sharma, MBBS2, Vishali Moond, MD3, Simran Joshi, MD4, Mehak Sachdeva, MBBS5, Nirav Thosani, MD6, Prateek Harne, MD7. P4284 - Infectious Complications and Safety Outcomes in Cholangioscopy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Luminis Health Anne Arundel Medical Center, Annapolis, MD; 3Saint Peter's University Hospital/Robert Wood Johnson Medical School loc, New Brunswick, NJ; 4Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 5University of Central Florida, HCA Healthcare GME, Ocala, FL; 6University of Texas Health, McGovern Medical School, Houston, TX; 7Allegheny Center for Digestive Health, Pittsburgh, PA
Introduction: Peroral cholangioscopy enables direct visualization of the biliary tree and has become increasingly utilized for the management of choledocholithiasis and indeterminate biliary strictures. However, concerns remain regarding post-procedural infectious complications, including bacteremia and cholangitis. Current guidelines offer limited guidance on prophylactic antibiotic use during cholangioscopy. We aimed to evaluate the pooled rates of bacteremia and other adverse events associated with cholangioscopy, assess procedural success, and examine the impact of antibiotic prophylaxis.
Methods: A systematic review and meta-analysis was conducted according to PRISMA guidelines. Literature searches were performed across PubMed, Embase, Scopus, Cochrane Library, and Google Scholar through March 2025. Thirteen studies encompassing 4,413 cholangioscopy-guided procedures were included. Pooled proportions for technical/clinical success and adverse events were calculated using random-effects models. Subgroup analyses evaluated the role of pre-procedural antibiotic use and biopsy.
Results: Pooled technical and clinical success rates were 97.3% (95% CI: 94.8%–98.6%) and 88.4% (95% CI: 80.5%–93.3%), respectively. Bacteremia was the most frequent infectious complication (6.8%; 95% CI: 3.1%–14.3%), followed by cholangitis (4.1%) and pancreatitis (3.6%). When adverse events were categorized using the ASGE lexicon, mild events were most common (7.5%; 95% CI: 4.1%–13.2%; I² = 93%), with rare severe (0.7%) or fatal (0.4%) complications. Studies without pre-procedural antibiotics or those involving biopsy showed higher bacteremia rates. Despite widespread use of prophylactic antibiotics, no consistent reduction in infectious complications was observed. Evidence of publication bias was detected (p < 0.01).
Discussion: Cholangioscopy is highly effective and generally safe; however, bacteremia remains a notable complication, particularly in high-risk patients and with biopsy use. The role of antibiotic prophylaxis remains unclear. Future studies should aim to standardize infection prevention protocols and define high-risk subgroups to optimize prophylactic strategies.
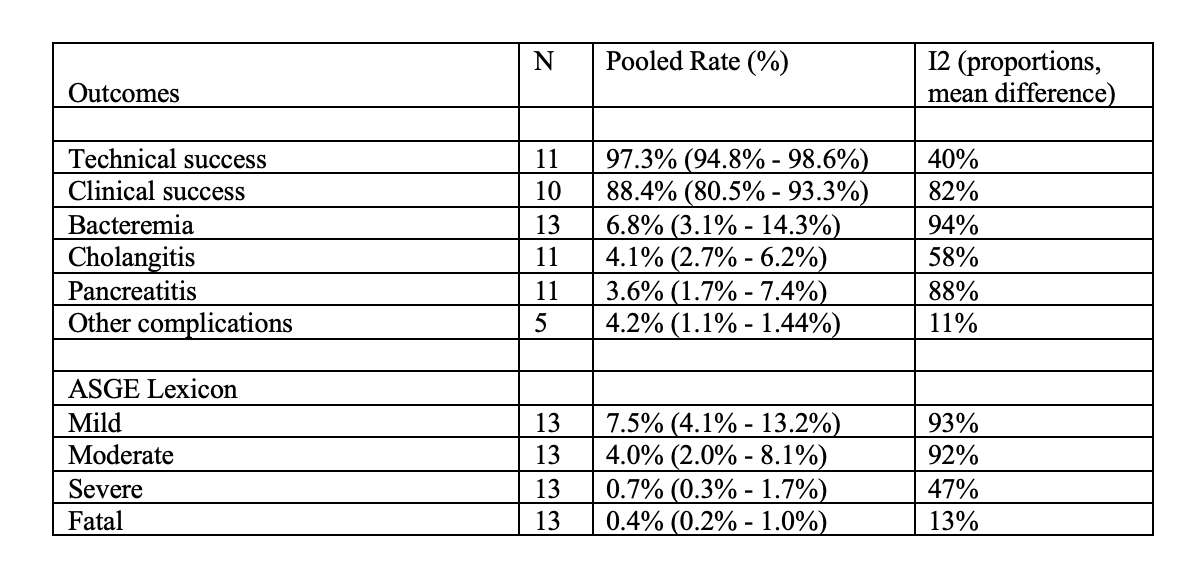
Figure: Table 1. Displays the results across each outcome for this meta-analysis.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Akshay Sharma indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Simran Joshi indicated no relevant financial relationships.
Mehak Sachdeva indicated no relevant financial relationships.
Nirav Thosani: Alpfa medical – Consultant. Roseaid – Creatorship rights.
Prateek Harne indicated no relevant financial relationships.
Shivangini Duggal, MD1, Akshay Sharma, MBBS2, Vishali Moond, MD3, Simran Joshi, MD4, Mehak Sachdeva, MBBS5, Nirav Thosani, MD6, Prateek Harne, MD7. P4284 - Infectious Complications and Safety Outcomes in Cholangioscopy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
