Tuesday Poster Session
Category: Biliary/Pancreas
P4282 - Weekend Admission and Outcomes in Percutaneous Transhepatic Biliary Drainage: A National Inpatient Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SG
Shubham Gupta, MD
Virtua Health System
Philadelphia, PA
Presenting Author(s)
Nakul Ganju, MD1, Shubham Gupta, MD2, Shaunak Ganju, BS3, Mesay Asfaw, MD4, Juan C. Santiago-Gonzalez, MD, MSc5, Farshad Aduli, MD5
1Department of Medicine, Howard University Hospital, Washington, DC; 2Virtua Health System, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 4Howard University, Washington, DC; 5Howard University Hospital, Washington, DC
Introduction: Percutaneous transhepatic biliary drainage (PTBD) is a key intervention for malignant or complex biliary obstruction when endoscopic access is not feasible. While effective, it carries risks including sepsis and in-hospital mortality. Prior studies have demonstrated worse outcomes for weekend admissions across various procedures, but its impact on PTBD outcomes remains unclear. This study aimed to evaluate whether weekend admission influences clinical outcomes or resource utilization in PTBD cases using a nationally representative database.
Methods: We conducted a retrospective analysis of the 2018–2021 National Inpatient Sample. Adult hospitalizations involving PTBD were identified and categorized by weekend vs. weekday admission. Primary outcomes included in-hospital mortality, length of stay (LOS), and total hospital charges. Multivariable logistic and linear regression models were used to adjust for demographic, clinical, and hospital-level variables.
Results: Among ~1,200 PTBD hospitalizations, 32% occurred on weekends. Mortality was similar between groups (3.5% weekend vs. 3.9% weekday, p=0.87). Weekend admissions showed a trend toward longer LOS (17.1 vs. 13.8 days, p=0.11) and higher charges ($221,647 vs. $172,678, p=0.23), though not statistically significant. In adjusted models, weekend admission was not associated with mortality (OR 0.91, 95% CI 0.45–1.82). However, sepsis significantly increased the odds of mortality (OR 4.87, 95% CI 1.97–12.02) and was associated with higher hospital charges (p< 0.001). Figures 1 and 2 illustrate LOS and charge differences by admission day.
Discussion: Despite concerns about the “weekend effect,” PTBD outcomes did not differ significantly by admission day. Consistent mortality may reflect the reliability of interventional radiology and standardized protocols across admission times. However, trends toward prolonged LOS and increased costs on weekends suggest potential delays in ancillary services or discharge coordination. Sepsis emerged as a strong driver of mortality and resource use, emphasizing the need for early recognition and management. These findings underscore the importance of system-level efficiency in urgent biliary interventions, regardless of admission timing.
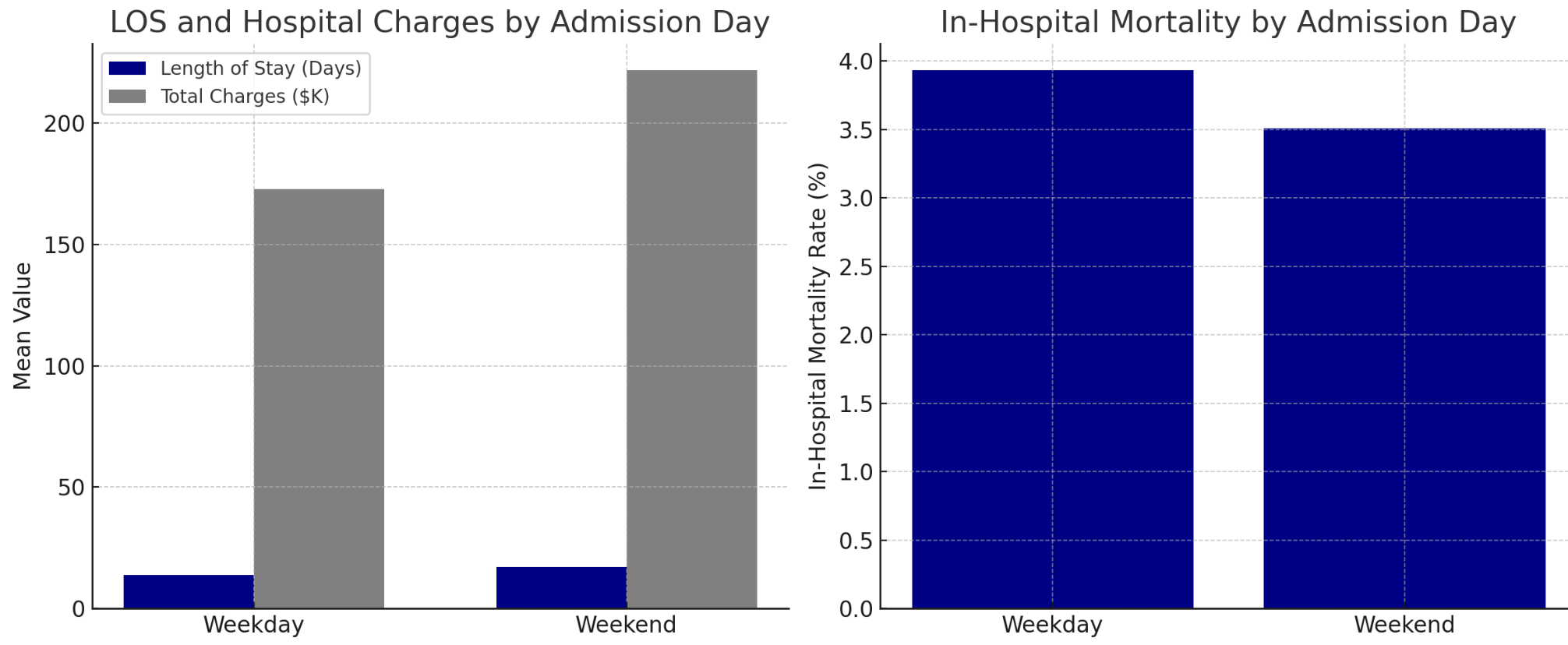
Figure: Figure 1. Inpatient outcomes for PTBD hospitalizations by admission day.
Left: Average length of stay and total charges (in $K) were higher for weekend admissions, though not statistically significant.
Right: In-hospital mortality rates were similar between groups, indicating no observed “weekend effect” in mortality.

Figure: Figure 2. In-hospital mortality rates for PTBD admissions stratified by age group and admission day. Bars are annotated with sample size (n). Mortality increased with age but remained consistent across weekdays and weekends. Low rates in younger groups reflect fewer events, not absence of admissions.
Disclosures:
Nakul Ganju indicated no relevant financial relationships.
Shubham Gupta indicated no relevant financial relationships.
Shaunak Ganju indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Nakul Ganju, MD1, Shubham Gupta, MD2, Shaunak Ganju, BS3, Mesay Asfaw, MD4, Juan C. Santiago-Gonzalez, MD, MSc5, Farshad Aduli, MD5. P4282 - Weekend Admission and Outcomes in Percutaneous Transhepatic Biliary Drainage: A National Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Medicine, Howard University Hospital, Washington, DC; 2Virtua Health System, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 4Howard University, Washington, DC; 5Howard University Hospital, Washington, DC
Introduction: Percutaneous transhepatic biliary drainage (PTBD) is a key intervention for malignant or complex biliary obstruction when endoscopic access is not feasible. While effective, it carries risks including sepsis and in-hospital mortality. Prior studies have demonstrated worse outcomes for weekend admissions across various procedures, but its impact on PTBD outcomes remains unclear. This study aimed to evaluate whether weekend admission influences clinical outcomes or resource utilization in PTBD cases using a nationally representative database.
Methods: We conducted a retrospective analysis of the 2018–2021 National Inpatient Sample. Adult hospitalizations involving PTBD were identified and categorized by weekend vs. weekday admission. Primary outcomes included in-hospital mortality, length of stay (LOS), and total hospital charges. Multivariable logistic and linear regression models were used to adjust for demographic, clinical, and hospital-level variables.
Results: Among ~1,200 PTBD hospitalizations, 32% occurred on weekends. Mortality was similar between groups (3.5% weekend vs. 3.9% weekday, p=0.87). Weekend admissions showed a trend toward longer LOS (17.1 vs. 13.8 days, p=0.11) and higher charges ($221,647 vs. $172,678, p=0.23), though not statistically significant. In adjusted models, weekend admission was not associated with mortality (OR 0.91, 95% CI 0.45–1.82). However, sepsis significantly increased the odds of mortality (OR 4.87, 95% CI 1.97–12.02) and was associated with higher hospital charges (p< 0.001). Figures 1 and 2 illustrate LOS and charge differences by admission day.
Discussion: Despite concerns about the “weekend effect,” PTBD outcomes did not differ significantly by admission day. Consistent mortality may reflect the reliability of interventional radiology and standardized protocols across admission times. However, trends toward prolonged LOS and increased costs on weekends suggest potential delays in ancillary services or discharge coordination. Sepsis emerged as a strong driver of mortality and resource use, emphasizing the need for early recognition and management. These findings underscore the importance of system-level efficiency in urgent biliary interventions, regardless of admission timing.
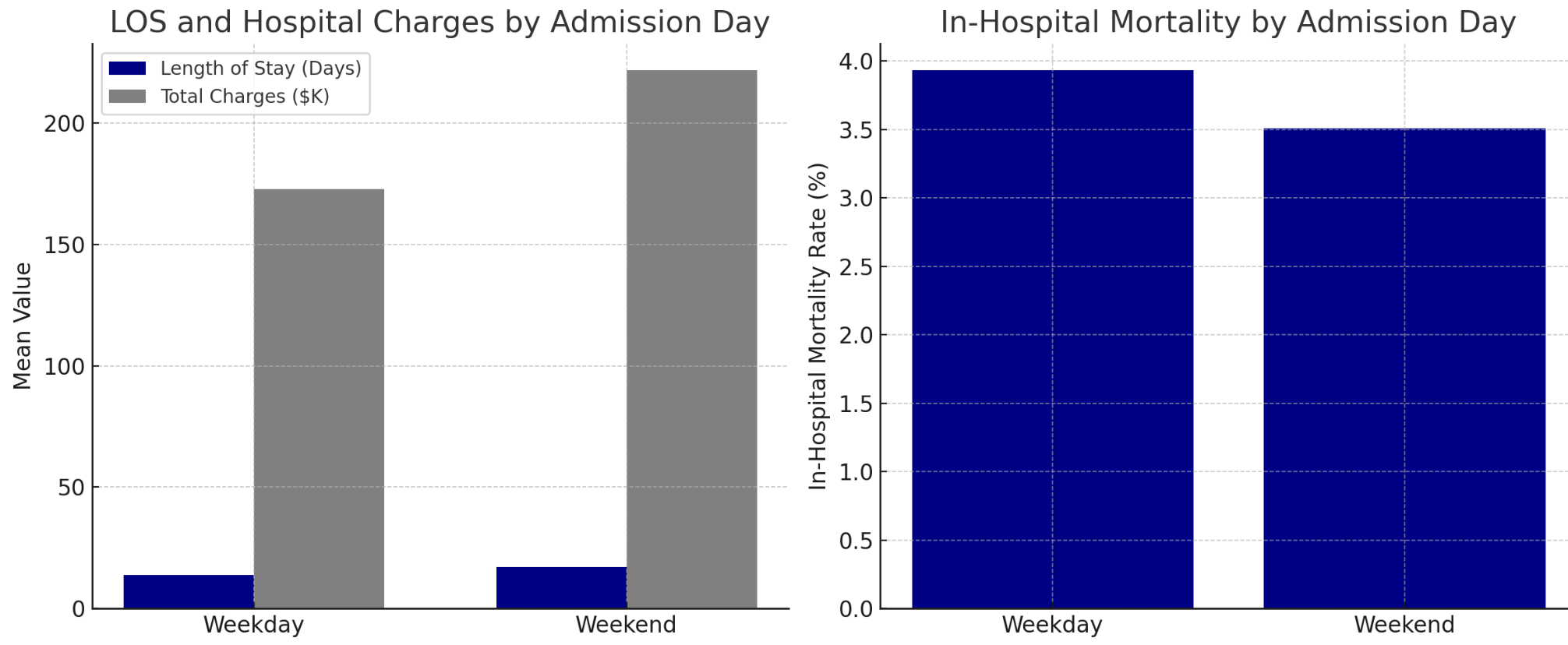
Figure: Figure 1. Inpatient outcomes for PTBD hospitalizations by admission day.
Left: Average length of stay and total charges (in $K) were higher for weekend admissions, though not statistically significant.
Right: In-hospital mortality rates were similar between groups, indicating no observed “weekend effect” in mortality.

Figure: Figure 2. In-hospital mortality rates for PTBD admissions stratified by age group and admission day. Bars are annotated with sample size (n). Mortality increased with age but remained consistent across weekdays and weekends. Low rates in younger groups reflect fewer events, not absence of admissions.
Disclosures:
Nakul Ganju indicated no relevant financial relationships.
Shubham Gupta indicated no relevant financial relationships.
Shaunak Ganju indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Nakul Ganju, MD1, Shubham Gupta, MD2, Shaunak Ganju, BS3, Mesay Asfaw, MD4, Juan C. Santiago-Gonzalez, MD, MSc5, Farshad Aduli, MD5. P4282 - Weekend Admission and Outcomes in Percutaneous Transhepatic Biliary Drainage: A National Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
