Tuesday Poster Session
Category: Biliary/Pancreas
P4359 - Correlation Between Statin Use and the Incidence of Acute Pancreatitis in Patients With Diabetes - A Global Database Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Luis Lara, MD (he/him/his)
Professor and Division Director
University of Cincinnati
Cincinnati, OH
Presenting Author(s)
Patricia Guzman Rojas, MD, MS1, Andrew Ofosu, MD, MPH2, Moamen Gabr, MD, MSc1, Rosanne Danielson, MD1, Milton Smith, MD1, Inuk Zandvakili, MD, PhD1, Wei-Wen Hsu, PhD1, Luis Lara, MD1
1University of Cincinnati, Cincinnati, OH; 2University of Cincinnati College of Medicine, Cincinnati, OH
Introduction: Statins are widely used to control serum lipids and reduce the risk of cardiovascular events. Common side-effects include myalgias, hepatotoxicity, proteinuria, and diabetes which are usually offset by the benefit. These medications have anti-inflammatory effects including down-regulation of pro-inflammatory cytokines. They have also been used to prevent post-ERCP acute pancreatitis (AP), and to prevent development of diabetes after AP, but an increased risk of AP in patients on statins has also been reported, without a clear mechanism of action. We studied the correlation with statin use and the risk of AP and severe AP (SAP) in patients with type 2 diabetes mellitus (DM2).
Methods: We used the global research database TriNetX (Cambridge, MA) which comprises over 315 million individual electronic medical records providing de-identified data. For this analysis data from 2014 to 2024 were compiled, and > 85% of the patients were from the United States. Adult patients ( >18yrs) with DM2 were included in the analysis and comprehensive exclusion criteria (39 total) were made to homogenize the comparison groups and to control confounders. Patients had no previous pancreatic disease and had to be on any statins for at least one year and were followed longitudinally. The cohorts were 1:1 propensity score matched for age sex, race, body weight, and smoking status.
Results: After matching, each cohort had 138,008 patients. The average age was 66.2 12.2 (SD), there were 47% females in each group, and 19.3% were African Americans. The risk of AP was similar, 0.275% in patients on statins and 0.337% in patients not on statins, RR 1.227, 95% CI 1.07-1.41, p =0.003. However, patients with DM2 that were not on statins had a decreased risk of developing severe AP, RR of 0.906, 95% CI 0.88-0.93, p< 0.0001. Both groups had a similar need to undergo ERCP (RR of 1.33, 95% CI 1.06-1.67, p=0.0136).
Discussion: In this retrospective cohort, the risk of AP was similar in patients with DM2 on statins. Interestingly, patients with DM2 on statins were more likely to develop SAP. It is not clear if this was associated with transient or persistent SAP or if it resulted in poorer outcomes. The effect of variables including medical history, and concomitant drug interactions may play a role in this perceived increased association. Statins metabolized by CYP3A4 may be more pancreato-toxic, so the type and dose of statin may play a role. More evidence to include statins as a cause of drug induced AP or SAP is necessary.
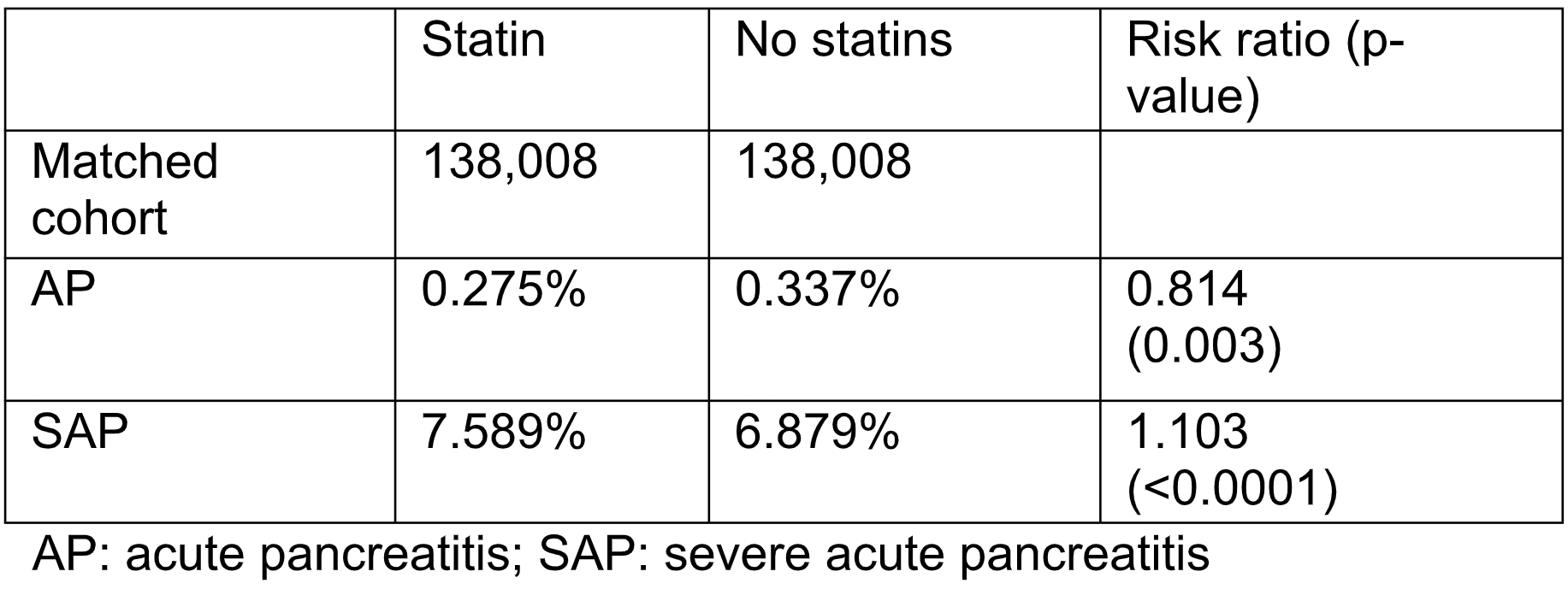
Figure: Table 1. Risk of acute pancreatitis (AP) and severe AP in patients with DM2 on statins
Disclosures:
Patricia Guzman Rojas indicated no relevant financial relationships.
Andrew Ofosu indicated no relevant financial relationships.
Moamen Gabr indicated no relevant financial relationships.
Rosanne Danielson indicated no relevant financial relationships.
Milton Smith indicated no relevant financial relationships.
Inuk Zandvakili: Eli Lilly – Consultant.
Wei-Wen Hsu indicated no relevant financial relationships.
Luis Lara: AbbVie – Consultant, Grant/Research Support, Speakers Bureau.
Patricia Guzman Rojas, MD, MS1, Andrew Ofosu, MD, MPH2, Moamen Gabr, MD, MSc1, Rosanne Danielson, MD1, Milton Smith, MD1, Inuk Zandvakili, MD, PhD1, Wei-Wen Hsu, PhD1, Luis Lara, MD1. P4359 - Correlation Between Statin Use and the Incidence of Acute Pancreatitis in Patients With Diabetes - A Global Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Cincinnati, Cincinnati, OH; 2University of Cincinnati College of Medicine, Cincinnati, OH
Introduction: Statins are widely used to control serum lipids and reduce the risk of cardiovascular events. Common side-effects include myalgias, hepatotoxicity, proteinuria, and diabetes which are usually offset by the benefit. These medications have anti-inflammatory effects including down-regulation of pro-inflammatory cytokines. They have also been used to prevent post-ERCP acute pancreatitis (AP), and to prevent development of diabetes after AP, but an increased risk of AP in patients on statins has also been reported, without a clear mechanism of action. We studied the correlation with statin use and the risk of AP and severe AP (SAP) in patients with type 2 diabetes mellitus (DM2).
Methods: We used the global research database TriNetX (Cambridge, MA) which comprises over 315 million individual electronic medical records providing de-identified data. For this analysis data from 2014 to 2024 were compiled, and > 85% of the patients were from the United States. Adult patients ( >18yrs) with DM2 were included in the analysis and comprehensive exclusion criteria (39 total) were made to homogenize the comparison groups and to control confounders. Patients had no previous pancreatic disease and had to be on any statins for at least one year and were followed longitudinally. The cohorts were 1:1 propensity score matched for age sex, race, body weight, and smoking status.
Results: After matching, each cohort had 138,008 patients. The average age was 66.2 12.2 (SD), there were 47% females in each group, and 19.3% were African Americans. The risk of AP was similar, 0.275% in patients on statins and 0.337% in patients not on statins, RR 1.227, 95% CI 1.07-1.41, p =0.003. However, patients with DM2 that were not on statins had a decreased risk of developing severe AP, RR of 0.906, 95% CI 0.88-0.93, p< 0.0001. Both groups had a similar need to undergo ERCP (RR of 1.33, 95% CI 1.06-1.67, p=0.0136).
Discussion: In this retrospective cohort, the risk of AP was similar in patients with DM2 on statins. Interestingly, patients with DM2 on statins were more likely to develop SAP. It is not clear if this was associated with transient or persistent SAP or if it resulted in poorer outcomes. The effect of variables including medical history, and concomitant drug interactions may play a role in this perceived increased association. Statins metabolized by CYP3A4 may be more pancreato-toxic, so the type and dose of statin may play a role. More evidence to include statins as a cause of drug induced AP or SAP is necessary.
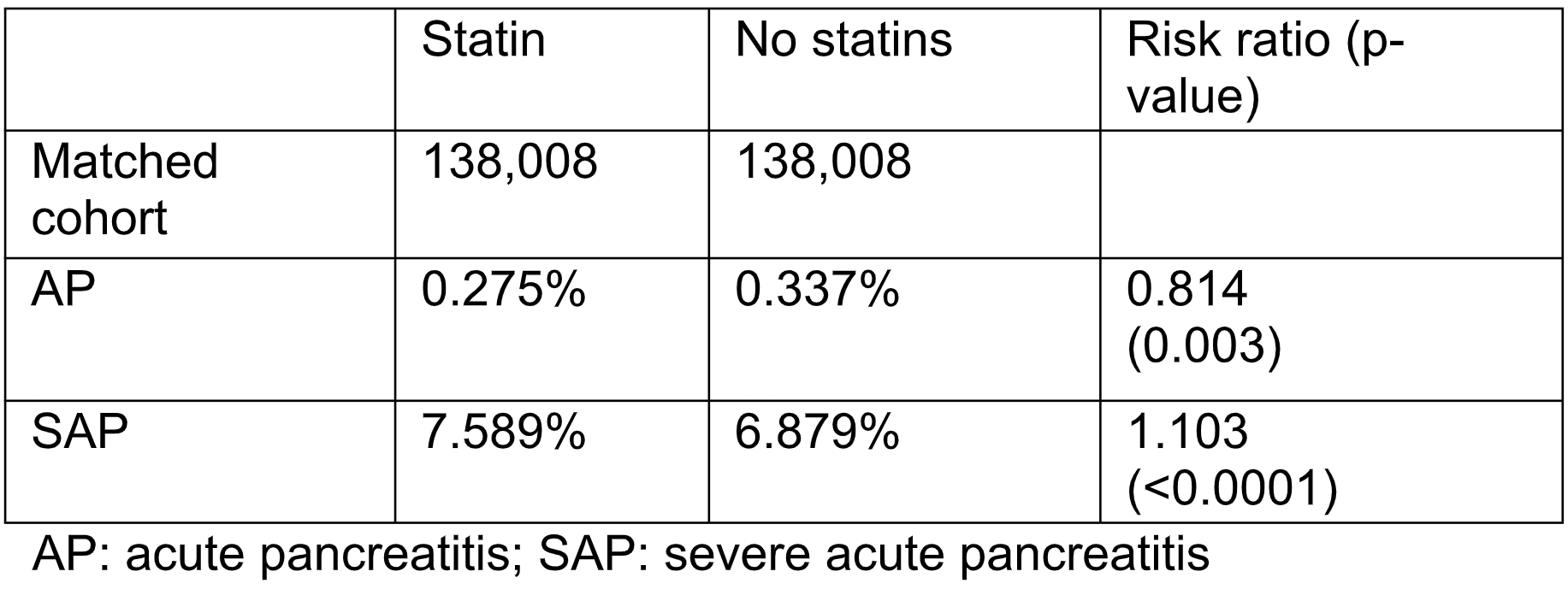
Figure: Table 1. Risk of acute pancreatitis (AP) and severe AP in patients with DM2 on statins
Disclosures:
Patricia Guzman Rojas indicated no relevant financial relationships.
Andrew Ofosu indicated no relevant financial relationships.
Moamen Gabr indicated no relevant financial relationships.
Rosanne Danielson indicated no relevant financial relationships.
Milton Smith indicated no relevant financial relationships.
Inuk Zandvakili: Eli Lilly – Consultant.
Wei-Wen Hsu indicated no relevant financial relationships.
Luis Lara: AbbVie – Consultant, Grant/Research Support, Speakers Bureau.
Patricia Guzman Rojas, MD, MS1, Andrew Ofosu, MD, MPH2, Moamen Gabr, MD, MSc1, Rosanne Danielson, MD1, Milton Smith, MD1, Inuk Zandvakili, MD, PhD1, Wei-Wen Hsu, PhD1, Luis Lara, MD1. P4359 - Correlation Between Statin Use and the Incidence of Acute Pancreatitis in Patients With Diabetes - A Global Database Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

