Tuesday Poster Session
Category: Biliary/Pancreas
P4358 - Prior Biliary Sphincterotomy and Peri-procedural Rectal Indomethacin Administration Significantly Reduce Post-ERCP Pancreatitis Incidence Compared to Index ERCP
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rahul Sandella, MD (he/him/his)
University of Chicago Medicine
Chicago, IL
Presenting Author(s)
Grace E. Kim, MD, Rahul Sandella, MD, Sebastian Dobrow, MD, Eric Montminy, MD, Uzma D. Siddiqui, MD, FACG, Dennis Chen, MD
University of Chicago Medicine, Chicago, IL
Introduction: Rectal indomethacin (RI) has been shown to reduce the risk of post-ERCP pancreatitis (PEP) in high-risk patients. Limited data exist on the protective effect of RI in non-high-risk patients, and administration in this setting varies based on provider preference. Previous research found patients with prior sphincterotomy still had a 2.7% rate of PEP (1). This study population did not routinely receive RI. Our aim was to examine the impact of RI on PEP rates in patients with prior sphincterotomy undergoing repeat ERCP (rERCP) compared to index ERCP (iERCP).
Methods: Patients who had initial ERCP with biliary sphincterotomy and at least one subsequent ERCP at a single tertiary referral center from 2022 to 2024 were identified using a procedure database. All patients received RI peri-procedurally. Demographics, procedure details, and PEP data were retrospectively collected.
Results: 158 patients undergoing 423 ERCPs met the inclusion criteria (Table 1). The most common indications were malignant obstruction for iERCP and anastomotic stricture for rERCP. Pancreatic duct (PD) manipulation occurred in 43.7% of iERCPs with PD stent placement in 89.9% of them; PD manipulation and stent placement occurred in 0.8% of rERCPs.
PEP incidence was significantly lower for rERCP (n=1) compared to iERCP (n=12; 0.4% vs. 7.6%, p=0.00005; Figure 1). The rERCP patient who developed PEP did not have PEP after his iERCP, and PD was not manipulated during the rERCP. Age, gender, inpatient status, PD manipulation, PD stenting, and peri-procedural administration of lactated ringers were not associated with PEP occurrence.
Discussion: Our study demonstrates a drastic reduction in PEP rates at rERCP compared with iERCP in patients who underwent RI administration. Compared to the published PEP rate of 2.7% for rERCP without routine RI (1), our PEP rate of 0.4% suggests a protective benefit of RI in these low-risk patients. Our study also utilized a novel design by examining the same population of patients for iERCP and rERCP to mitigate external confounding factors. Further prospective studies are needed to confirm the PEP-reducing benefit of RI for patients with prior sphincterotomy and evaluate the cost effectiveness of administering RI in all patients undergoing ERCP.
Reference
(1) Holt N, Saber E, et al. ERCP in patients with prior sphincterotomy has a 50% lower rate of post-ERCP pancreatitis and fewer unplanned hospital admissions. Scand J Gastroenterol. 2022 Dec;57(12):1517-1521
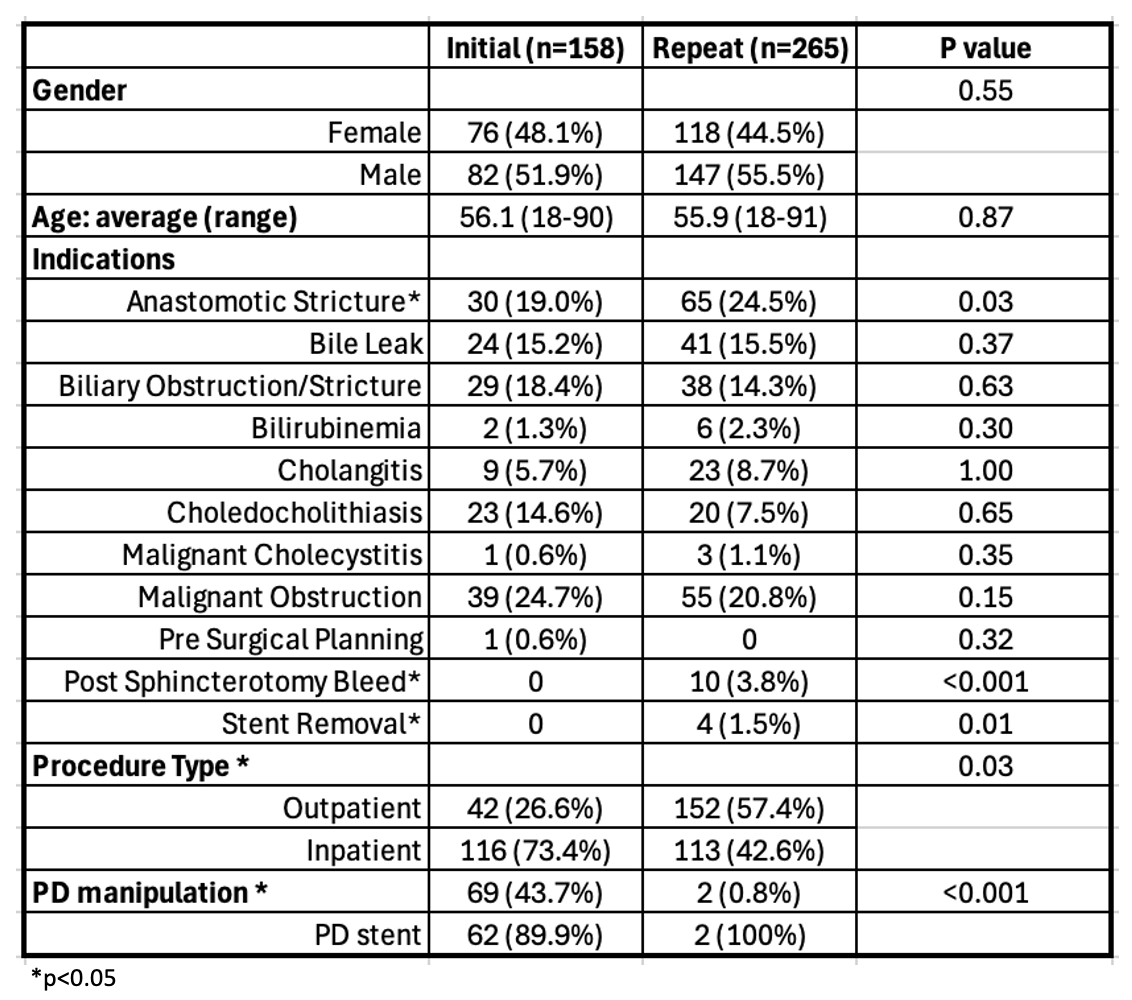
Figure: Figure 1: Comparison of post-ERCP pancreatitis incidence between initial and repeat ERCP among patients who underwent rectal indomethacin administration
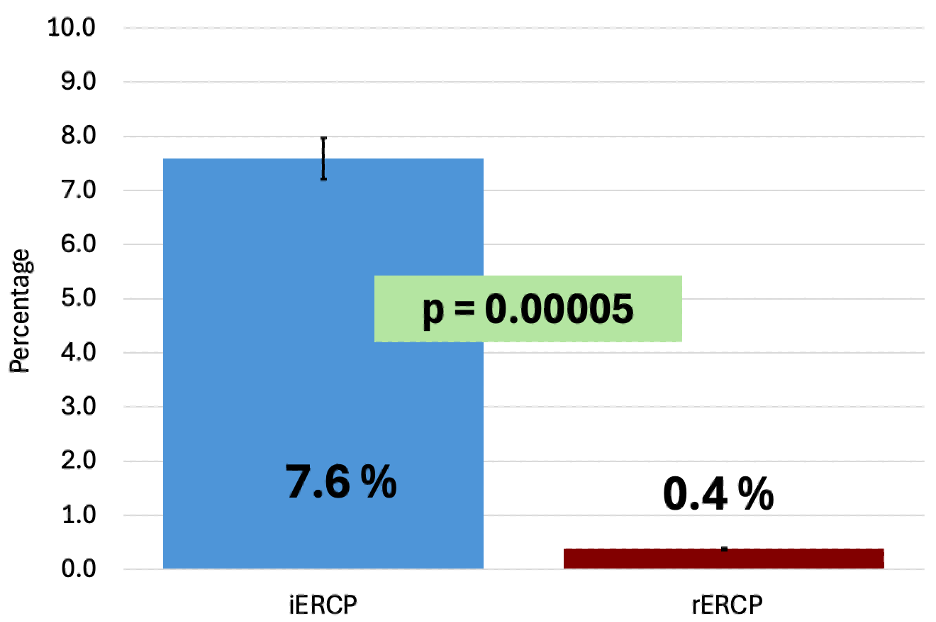
Figure: Table 1: Characteristics associated with initial vs repeat ERCP
Disclosures:
Grace Kim indicated no relevant financial relationships.
Rahul Sandella indicated no relevant financial relationships.
Sebastian Dobrow indicated no relevant financial relationships.
Eric Montminy indicated no relevant financial relationships.
Uzma Siddiqui: Boston Scientific – Consultant, Grant/Research Support, Speakers Bureau. ConMed – Consultant, Speakers Bureau. Cook – Consultant, Speakers Bureau. Medtronic – Consultant, Speakers Bureau. Olympus – Consultant, Grant/Research Support, Speakers Bureau.
Dennis Chen indicated no relevant financial relationships.
Grace E. Kim, MD, Rahul Sandella, MD, Sebastian Dobrow, MD, Eric Montminy, MD, Uzma D. Siddiqui, MD, FACG, Dennis Chen, MD. P4358 - Prior Biliary Sphincterotomy and Peri-procedural Rectal Indomethacin Administration Significantly Reduce Post-ERCP Pancreatitis Incidence Compared to Index ERCP, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Chicago Medicine, Chicago, IL
Introduction: Rectal indomethacin (RI) has been shown to reduce the risk of post-ERCP pancreatitis (PEP) in high-risk patients. Limited data exist on the protective effect of RI in non-high-risk patients, and administration in this setting varies based on provider preference. Previous research found patients with prior sphincterotomy still had a 2.7% rate of PEP (1). This study population did not routinely receive RI. Our aim was to examine the impact of RI on PEP rates in patients with prior sphincterotomy undergoing repeat ERCP (rERCP) compared to index ERCP (iERCP).
Methods: Patients who had initial ERCP with biliary sphincterotomy and at least one subsequent ERCP at a single tertiary referral center from 2022 to 2024 were identified using a procedure database. All patients received RI peri-procedurally. Demographics, procedure details, and PEP data were retrospectively collected.
Results: 158 patients undergoing 423 ERCPs met the inclusion criteria (Table 1). The most common indications were malignant obstruction for iERCP and anastomotic stricture for rERCP. Pancreatic duct (PD) manipulation occurred in 43.7% of iERCPs with PD stent placement in 89.9% of them; PD manipulation and stent placement occurred in 0.8% of rERCPs.
PEP incidence was significantly lower for rERCP (n=1) compared to iERCP (n=12; 0.4% vs. 7.6%, p=0.00005; Figure 1). The rERCP patient who developed PEP did not have PEP after his iERCP, and PD was not manipulated during the rERCP. Age, gender, inpatient status, PD manipulation, PD stenting, and peri-procedural administration of lactated ringers were not associated with PEP occurrence.
Discussion: Our study demonstrates a drastic reduction in PEP rates at rERCP compared with iERCP in patients who underwent RI administration. Compared to the published PEP rate of 2.7% for rERCP without routine RI (1), our PEP rate of 0.4% suggests a protective benefit of RI in these low-risk patients. Our study also utilized a novel design by examining the same population of patients for iERCP and rERCP to mitigate external confounding factors. Further prospective studies are needed to confirm the PEP-reducing benefit of RI for patients with prior sphincterotomy and evaluate the cost effectiveness of administering RI in all patients undergoing ERCP.
Reference
(1) Holt N, Saber E, et al. ERCP in patients with prior sphincterotomy has a 50% lower rate of post-ERCP pancreatitis and fewer unplanned hospital admissions. Scand J Gastroenterol. 2022 Dec;57(12):1517-1521
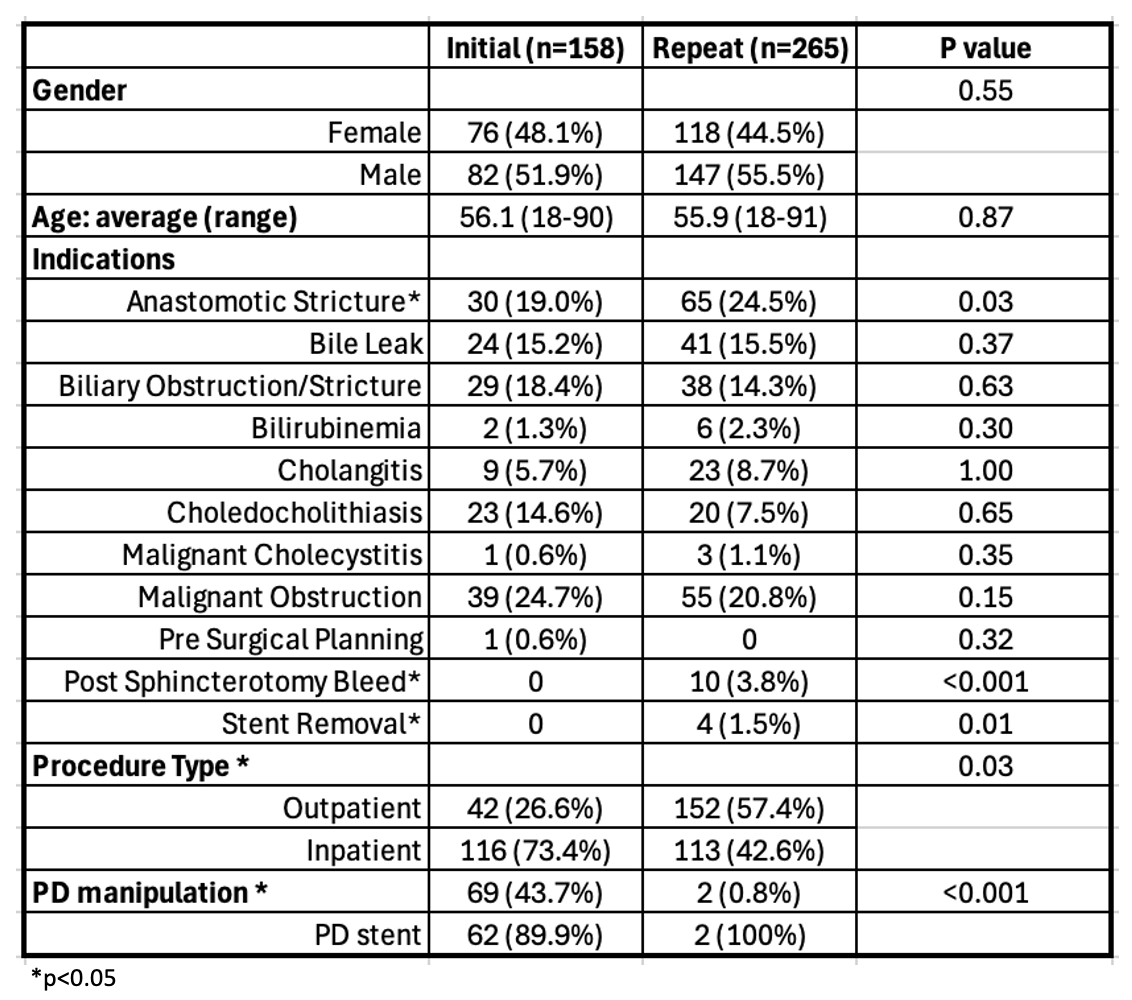
Figure: Figure 1: Comparison of post-ERCP pancreatitis incidence between initial and repeat ERCP among patients who underwent rectal indomethacin administration
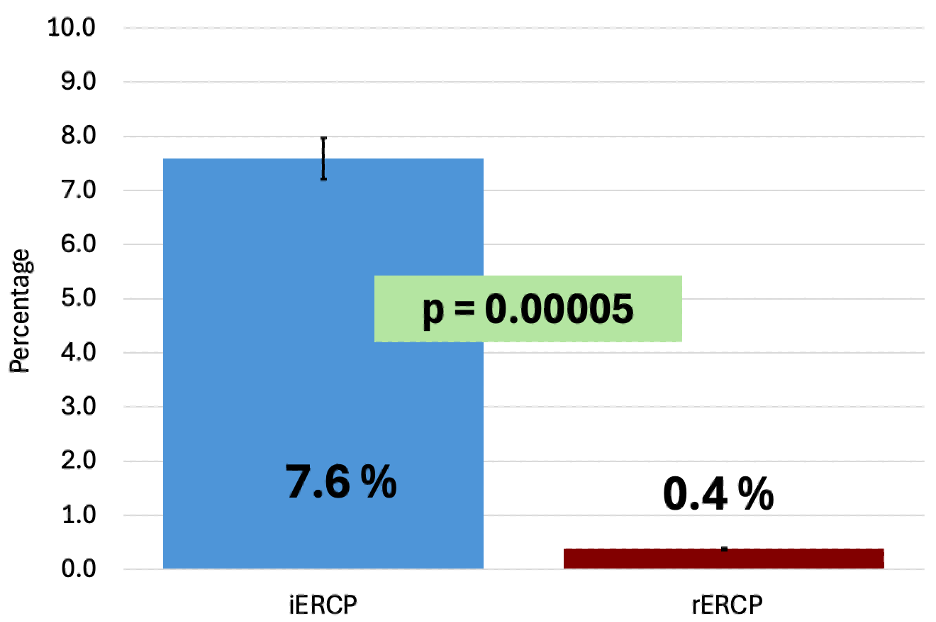
Figure: Table 1: Characteristics associated with initial vs repeat ERCP
Disclosures:
Grace Kim indicated no relevant financial relationships.
Rahul Sandella indicated no relevant financial relationships.
Sebastian Dobrow indicated no relevant financial relationships.
Eric Montminy indicated no relevant financial relationships.
Uzma Siddiqui: Boston Scientific – Consultant, Grant/Research Support, Speakers Bureau. ConMed – Consultant, Speakers Bureau. Cook – Consultant, Speakers Bureau. Medtronic – Consultant, Speakers Bureau. Olympus – Consultant, Grant/Research Support, Speakers Bureau.
Dennis Chen indicated no relevant financial relationships.
Grace E. Kim, MD, Rahul Sandella, MD, Sebastian Dobrow, MD, Eric Montminy, MD, Uzma D. Siddiqui, MD, FACG, Dennis Chen, MD. P4358 - Prior Biliary Sphincterotomy and Peri-procedural Rectal Indomethacin Administration Significantly Reduce Post-ERCP Pancreatitis Incidence Compared to Index ERCP, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

