Tuesday Poster Session
Category: Biliary/Pancreas
P4356 - The Incidence of Exocrine Pancreatic Insufficiency Following an Index Episode of Acute Necrotizing Pancreatitis: A Propensity-Matched Analysis of US Collaborative Network Data
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ujwala Pamidimukkala, MD (she/her/hers)
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Ujwala Pamidimukkala, MD1, Vikram Ram. Rajagopalan, MBBS1, Azizullah Beran, MD1, Mina Batarseh, MD1, Hussein Baydoun, MD1, Awais Ahmed, MD1, Nasir Saleem, MD1, Daryl Ramai, MD, MPH, MSc2, Mohannad Yousef, MD3, Aladdin Dahbour, MD1, Indira Bhavsar-Burke, MD4, Mohammad Al-Haddad, MD1, Itegbemie Obaitan, MD, MPH1
1Indiana University School of Medicine, Indianapolis, IN; 2Brigham and Women’s Hospital, Harvard Medical School, Salt Lake City, UT; 3Michigan State University/Hurley Medical Center, Flint, MI; 4University of Texas Southwestern School of Medicine, Dallas, TX
Introduction: Acute necrotizing pancreatitis (ANP), a severe form of acute pancreatitis, can lead to long-term metabolic complications including exocrine pancreatic insufficiency (EPI), which may cause weight loss, steatorrhea, and associated conditions such as anemia and osteoporosis which arise as a consequence of malabsorption. The incidence of EPI after acute pancreatitis has been previously described in small single- and multi-center cohort studies; however, the comparative long-term incidence of EPI in ANP and acute interstitial pancreatitis patients using real-world nationally representative data has not been previously quantified.
Methods: We searched the United States (U.S.) Collaborative Network on the platform TriNetX from inception to May 23, 2025 using International Classification of Diseases, Tenth Revision (ICD-10) codes appropriate to ANP and acute interstitial pancreatitis. We identified all patients with a documented fecal elastase value less than 200ug/L placed on pancreatic enzymes supplementation during a 12-month follow-up period. One-to-one propensity score matching was carried out based on demographic variables and all comorbidities associated with malabsorption (Table 1). The primary outcome (EPI) was calculated and expressed as an odds ratio (OR) along with a 95% confidence interval (CI). Statistical significance was defined as a two-sided p-value < 0.05.
Results: Our database search found 148,135 patients with a diagnosis of acute pancreatitis and EPI in the follow-up window. After propensity-score matching was carried out, 17,176 patients were included into our study (8,588 patients in each cohort). We found an EPI incidence of 8.7% in the ANP cohort over the follow-up period, compared to an EPI incidence of 2.2% in the acute interstitial pancreatitis cohort. There were increased odds of EPI in patients with an index episode of ANP compared to patients with acute interstitial pancreatitis (OR 4.2, 95% CI 3.595, 4.991, p=0.000) (Table 2).
Discussion: There are significantly higher odds of developing EPI in patients with ANP over a 12-month period compared to patients with acute interstitial pancreatitis. Our findings highlight the importance of careful long-term monitoring for EPI to prevent downstream malabsorption-related complications in this patient population. Prospective studies are needed to validate our findings.
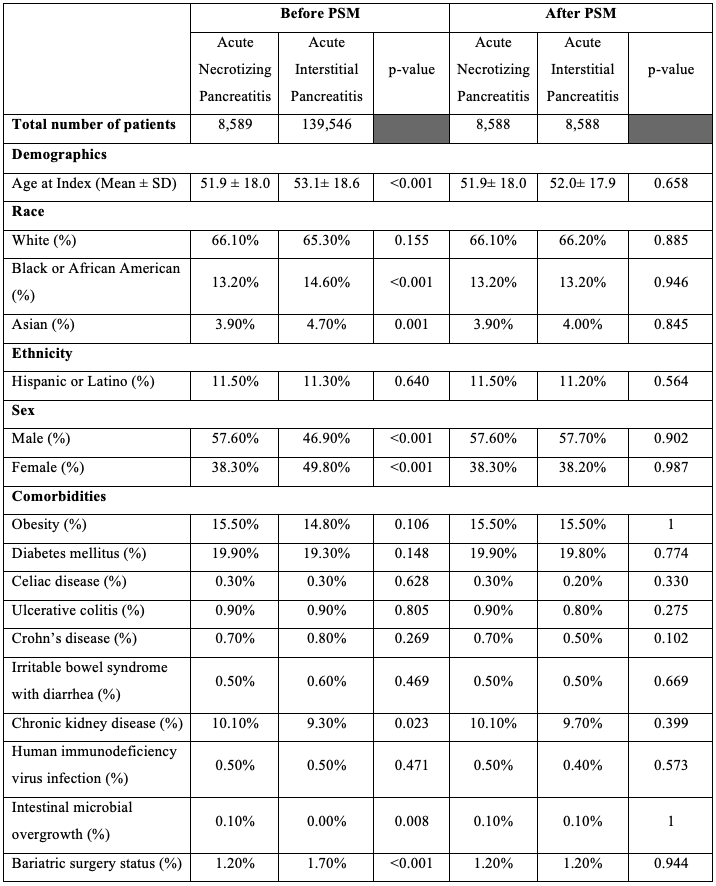
Figure: Table 1: Baseline patient characteristics in acute necrotizing pancreatitis and acute interstitial pancreatitis before and after propensity-score matching. Abbreviations: PSM: propensity-score matching, SD: standard deviation.
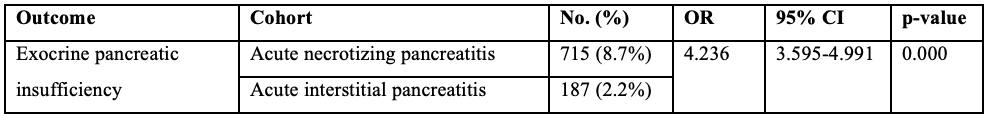
Figure: Table 2: Incidence of exocrine pancreatic insufficiency within 1 year after acute necrotizing pancreatitis and acute interstitial pancreatitis. Abbreviations: OR: odds ratio, CI: confidence interval.
Disclosures:
Ujwala Pamidimukkala indicated no relevant financial relationships.
Vikram Rajagopalan indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Mina Batarseh indicated no relevant financial relationships.
Hussein Baydoun indicated no relevant financial relationships.
Awais Ahmed indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
Daryl Ramai indicated no relevant financial relationships.
Mohannad Yousef indicated no relevant financial relationships.
Aladdin Dahbour indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace diagnostics – Consultant.
Itegbemie Obaitan indicated no relevant financial relationships.
Ujwala Pamidimukkala, MD1, Vikram Ram. Rajagopalan, MBBS1, Azizullah Beran, MD1, Mina Batarseh, MD1, Hussein Baydoun, MD1, Awais Ahmed, MD1, Nasir Saleem, MD1, Daryl Ramai, MD, MPH, MSc2, Mohannad Yousef, MD3, Aladdin Dahbour, MD1, Indira Bhavsar-Burke, MD4, Mohammad Al-Haddad, MD1, Itegbemie Obaitan, MD, MPH1. P4356 - The Incidence of Exocrine Pancreatic Insufficiency Following an Index Episode of Acute Necrotizing Pancreatitis: A Propensity-Matched Analysis of US Collaborative Network Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Brigham and Women’s Hospital, Harvard Medical School, Salt Lake City, UT; 3Michigan State University/Hurley Medical Center, Flint, MI; 4University of Texas Southwestern School of Medicine, Dallas, TX
Introduction: Acute necrotizing pancreatitis (ANP), a severe form of acute pancreatitis, can lead to long-term metabolic complications including exocrine pancreatic insufficiency (EPI), which may cause weight loss, steatorrhea, and associated conditions such as anemia and osteoporosis which arise as a consequence of malabsorption. The incidence of EPI after acute pancreatitis has been previously described in small single- and multi-center cohort studies; however, the comparative long-term incidence of EPI in ANP and acute interstitial pancreatitis patients using real-world nationally representative data has not been previously quantified.
Methods: We searched the United States (U.S.) Collaborative Network on the platform TriNetX from inception to May 23, 2025 using International Classification of Diseases, Tenth Revision (ICD-10) codes appropriate to ANP and acute interstitial pancreatitis. We identified all patients with a documented fecal elastase value less than 200ug/L placed on pancreatic enzymes supplementation during a 12-month follow-up period. One-to-one propensity score matching was carried out based on demographic variables and all comorbidities associated with malabsorption (Table 1). The primary outcome (EPI) was calculated and expressed as an odds ratio (OR) along with a 95% confidence interval (CI). Statistical significance was defined as a two-sided p-value < 0.05.
Results: Our database search found 148,135 patients with a diagnosis of acute pancreatitis and EPI in the follow-up window. After propensity-score matching was carried out, 17,176 patients were included into our study (8,588 patients in each cohort). We found an EPI incidence of 8.7% in the ANP cohort over the follow-up period, compared to an EPI incidence of 2.2% in the acute interstitial pancreatitis cohort. There were increased odds of EPI in patients with an index episode of ANP compared to patients with acute interstitial pancreatitis (OR 4.2, 95% CI 3.595, 4.991, p=0.000) (Table 2).
Discussion: There are significantly higher odds of developing EPI in patients with ANP over a 12-month period compared to patients with acute interstitial pancreatitis. Our findings highlight the importance of careful long-term monitoring for EPI to prevent downstream malabsorption-related complications in this patient population. Prospective studies are needed to validate our findings.
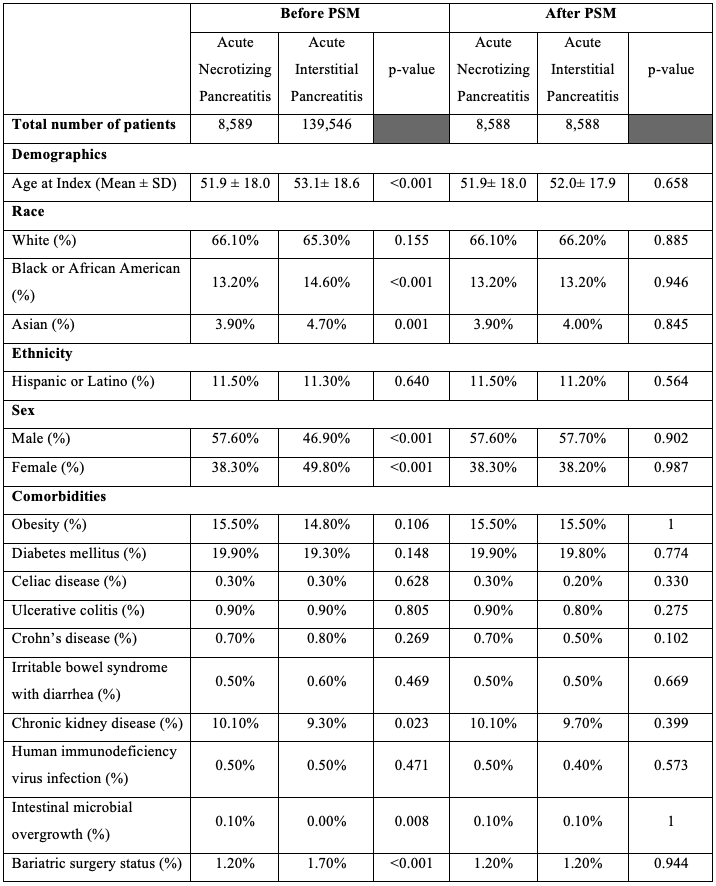
Figure: Table 1: Baseline patient characteristics in acute necrotizing pancreatitis and acute interstitial pancreatitis before and after propensity-score matching. Abbreviations: PSM: propensity-score matching, SD: standard deviation.
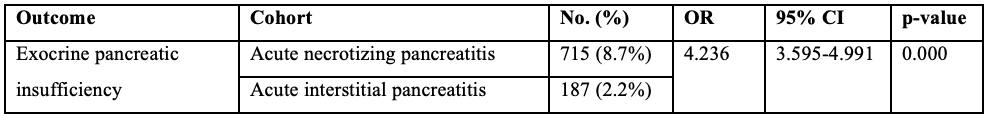
Figure: Table 2: Incidence of exocrine pancreatic insufficiency within 1 year after acute necrotizing pancreatitis and acute interstitial pancreatitis. Abbreviations: OR: odds ratio, CI: confidence interval.
Disclosures:
Ujwala Pamidimukkala indicated no relevant financial relationships.
Vikram Rajagopalan indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Mina Batarseh indicated no relevant financial relationships.
Hussein Baydoun indicated no relevant financial relationships.
Awais Ahmed indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
Daryl Ramai indicated no relevant financial relationships.
Mohannad Yousef indicated no relevant financial relationships.
Aladdin Dahbour indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace diagnostics – Consultant.
Itegbemie Obaitan indicated no relevant financial relationships.
Ujwala Pamidimukkala, MD1, Vikram Ram. Rajagopalan, MBBS1, Azizullah Beran, MD1, Mina Batarseh, MD1, Hussein Baydoun, MD1, Awais Ahmed, MD1, Nasir Saleem, MD1, Daryl Ramai, MD, MPH, MSc2, Mohannad Yousef, MD3, Aladdin Dahbour, MD1, Indira Bhavsar-Burke, MD4, Mohammad Al-Haddad, MD1, Itegbemie Obaitan, MD, MPH1. P4356 - The Incidence of Exocrine Pancreatic Insufficiency Following an Index Episode of Acute Necrotizing Pancreatitis: A Propensity-Matched Analysis of US Collaborative Network Data, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
